Abstract
Mycobacterium marinum, an aerobic, non-tuberculous, environmental mycobacterium, is the etiologic agent responsible for "fish tank granuloma." (1) Found in aquatic environments, particularly where water is relatively still or stagnant, M. marinum produces infection in fish, as well as humans. Infection follows exposure to contaminated water and direct inoculation of the organism via breaks in the skin. (1) The resulting primary lesion is usually a red-to-violaceous plaque or nodule, which can have an overlying crust or verrucous surface that may ulcerate and, in some cases, may be accompanied by satellite lesions and lymphangitic spread. We present an aggressive case of M. marinum infection with prominent lymph node involvement in an otherwise healthy 34-year-old woman whose course was complicated by delayed diagnosis and treatment with systemic steroids.
Case Report
A 34-year-old Hispanic woman presented with a 6-week history of a non-healing "insect bite" on her left thumb and mildly tender nodules along the length of her left arm. Approximately one month before presenting to the dermatology clinic, the patient visited the emergency department, at which time she was started on a course of cephalexin. Prior to this visit, treatment had consisted solely of cleansing the wound with hydrogen peroxide, which was not helpful. She returned to the emergency department 3 days later because of an apparent allergic reaction to her medication, which prompted discontinuation of the cephalexin and institution of a 2-week course of azithromycin, as well as a course of oral methylprednisolone starting at 48 mg daily on day one and tapering to 8 mg daily by day 6. Despite completing her course of azithromycin, the patient developed a new abscess on her left arm, proximal to her other lesions, which prompted her to visit another emergency department. She was found to have an elevated white blood cell count, fever, and several palpable lymph nodes tracking along her left arm. The new abscess was cultured and debrided, and the patient was placed on ciprofloxacin. Culture results were negative for fungus or bacteria. The patient was subsequently referred to the dermatology service.
The patient was unable to recall any insect bites, and she denied any gardening activities. Three weeks prior to the appearance of the initial lesion on her left thumb, she had cleaned her tropical fish tank after 4 cardinal tetras (Paracheirodon axelrodi) had died, but she denied placing her left hand or arm into the tank. The patient expressed concern over 2 enlarging purple ulcers, and the mildly tender, enlarging bumps that seemed to be spreading along her left arm. She denied any systemic or joint complaints, and her past medical history was unremarkable.
On physical examination, a purple nodule with central ulceration was present over the posterior metacarpophalangeal joint of the left thumb (Figure 1). On the left forearm, at the site where a lesion had undergone debridement, there was a purple scar with granulation tissue and central ulceration (Figure 2). Examination of the left arm demonstrated 4 mildly tender lymph nodes, measuring 1 to 3 cm in a linear array at the wrist, lateral mid-forearm, elbow, and left axilla; the first two lymph nodes were surmounted by cutaneous nodules (Figure 3).
[FIGURE 1 OMITTED]
[FIGURE 2 OMITTED]
[FIGURE 3 OMITTED]
[FIGURE 4 OMITTED]
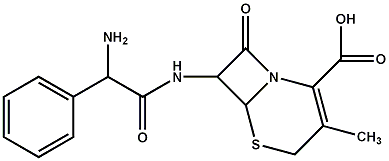
Given the severity of the patient's presentation and the previously negative culture results from one of the abscesses, fine needle aspiration (FNA) was performed on the epitrochlear lymph node and an excisional biopsy was performed on the lymph node at the wrist. A punch biopsy specimen taken from the nodule on the proximal thumb revealed well-formed granulomas with a lymphoid rim, consistent with an infectious granulomatous dermatitis (Figure 4). Tissue gram stain, staining for acid-fast bacilli, and Gomori-methenamine-silver staining failed to identify any organisms in the punch biopsy specimen. Four weeks later, cultures from the FNA and lymph node biopsy grew Mycobacterium marinum.
Discussion
Mycobacterium marinum is a rod-shaped, aerobic, non-tuberculous, photochromogenic, atypical mycobacterium. A non-sporulating organism, M. marinum grows best at 31[degrees]C, albeit slowly, requiring 2 to 3 weeks before becoming apparent in culture. (2) When M. marinum infects fish, it causes fish tuberculosis (TB), which is characterized by anorexia, emaciation, exophthalmia, skin defects, spinal deformities, distention of the abdomen, and sudden death. (3) Both freshwater and marine fish can develop fish TB; the more commonly afflicted fish families include fish readily available to aquarists, especially Characidae (tetras) and Cyprinidae (barbs, goldfish, koi). (4) Interestingly, an in vitro model for the study of M. marinum virulence mechanisms using carp (Cyprinus carpio) monocytic cell lines was developed because fish monocytes can differentiate between pathogenic and non-pathogenic mycobacterial species. (5)
Superficial skin infection in humans caused by M. marinum is known by many names, including swimming pool granuloma, fish tank granuloma, fish fancier's finger, mariner's TB, Buruli ulcer, Bairnsdale ulcer, and Searle's ulcer. (6) The estimated yearly incidence of skin infection is 2.7 per million adults. (7) Approximately 25% of these patients are aquarium hobbyists, for whom the most common site of infection is the dominant right hand. (1,8) The age of onset is usually the second to fourth decade, and males are affected more often than females, probably because of occupational exposure. (7)
M. marinum infection requires damaged skin as a portal for inoculation. The primary lesion usually presents as a red-to-violaceous plaque or nodule with a crusted or verrucous surface, which may ulcerate and suppurate. (1,2) The first signs of cutaneous disease are apparent within 2 to 3 weeks after inoculation. (9) Most patients present with multiple lesions in a sporotrichoid pattern; occasionally, patients present with a solitary lesion. (1,10-13) Because M. marinum prefers to grow at temperatures below 37[degrees]C, infection tends to confine itself to skin; consequently, lymphadenopathy is uncommon, and mild when it does occur, and disseminated disease, which occurs almost exclusively in immunocompromised hosts, is exceptional. (12-15) Rarely, involvement of deeper structures may occur, producing arthritis, tenosynovitis, and osteomyelitis. (7,12) Lesions may persist for months to years without treatment; however, the prognosis is often good for limited disease, since in many cases, spontaneous regression occurs with scarring. (16)
The treatment of M. marinum infection has not been standardized. Suggested first-line therapies include monotherapy with minocycline, 100 to 200 mg daily for 6 to 12 weeks, (10) or combination therapy using a macrolide antibiotic, especially clarithromycin, or possibly azithromycin, with ethambutol or rifampin. (1) Monotherapy with tetracycline antibiotics has been associated with a low rate of treatment failure, although infections reportedly treated in this manner have generally been limited to skin and soft tissues. (12) Because of the unreliability of susceptibility testing for M. marinum and the possibility of emerging resistance, some suggest avoiding monotherapy altogether and advocate treating with 2 agents for 1 to 2 months after resolution of all lesions. (1) Disseminated infection, as well as deep infection, which may require surgical debridement, may benefit from treatment with 3 antibiotics. (1)
The differential diagnosis for unilesional cutaneous M. marinum disease includes bromoderma, iododerma, deep fungal infections, foreign body reaction, other atypical mycobacterioses (eg, M. chelonae, M. fortuitum, M. gordonae), nocardiosis, sporotrichosis, syphilis, neoplasia, tuberculosis verrucosa cutis, tularemia, verruca vulgaris, and yaws. (16) The differential diagnosis for cutaneous M. marinum infections with lymphangitic spread includes actinomycosis, deep fungal infections, leishmaniasis, nocardiosis, sporotrichosis, staphylococcal or group A streptococcal lymphangitis, and tularemia. (16)
Although M. marinum infection tends to be superficial and only occasionally associated with lymphadenopathy, our case, which was characterized by a sporotrichoid presentation, is notable for prominent lymphadenopathy and abscesses in a young and otherwise healthy woman. Two factors may have contributed to this unusual pattern of involvement. First, the patient was placed on methylprednisolone by physicians suspecting a drug eruption, which likely rendered her temporarily immunodeficient. Second, there was a significant delay before she received effective antibiotic therapy, which was the result of a delay in diagnosis. The patient had taken cephalexin for 3 days, azithromycin for 2 weeks and later ciprofloxacin for 2 weeks. Azithromycin and ciprofloxacin have been shown to be effective only when taken concurrently. (19) Most reported cases are characterized by a substantial time lag, ranging from weeks to several years, between the onset of skin lesions and correct diagnosis, during which time the patient is likely to receive ineffective, or even inappropriate, treatment that may eventuate in unusual presentations. (13,17-19)
In our case, diagnosis and appropriate treatment were delayed by the initial negative culture results. When performed properly, cultures of M. marinum lesions are positive approximately 70% to 80% of the time. (6) Negative lesional culture results necessitate a high index of suspicion and more aggressive diagnostic approaches, such as FNA or lymph node biopsy for culture, or even polymerase chain reaction (PCR) studies. (20) After M. marinum infection was confirmed by both FNA and lymph node biopsy culture, our patient was started on minocycline, 100 mg twice daily, which she took for 3 months, and within 2 weeks, she experienced rapid involution of the enlarged lymph nodes. Healing of her ulcers was complete after 3 months. One year later, she remains disease free.
References
1. Lewis FMT, Marsh BJ, Fordham von Reyn C. Fish tank exposure and cutaneous infections due to Mycobacterium marinum: tuberculin skin testing, treatment, and prevention. Clinical Infectious Disease. 2003;37:390-397.
2. Brooks GF, Butel JS, Morse SA. Jawetz, Melnick, & Adelberg's Medical Microbiology. 21st ed. Stamford, Conn: Appleton & Lange; 1998;287.
3. Bassler, Gerald. Diseases in Marine Aquarium Fish: Causes, Symptoms, Treatment. Bassleer Biofish, Westmeerbeek, Belgium; 1996;51-52.
4. Provet healthcare information. Copyright 1999-2004. Mycobacterium Marinum. Available at: http://www.provet.co.uk. Accessed July 6, 2005.
5. El-etre S, Yan L, Cirillo J. Fish monocytes as a model for Mycobacterial host-pathogen interactions. Infection and Immunity. 2001;69:7310-7317.
6. Ramos M-e-Silva, Ribeiro de Castro MC. Mycobacterial infections. In: Bolognia JL, Jorizzo JL, Rapini R, et al, eds. Dermatology. St. Louis: Mosby; 2003:1159.
7. Edelstein H. Mycobacterium marinum skin infections. Report of 31 cases and review of the literature. Arch Intern Med. 1994;154:1359-64.
8. Schomoor P, Descamps V, Bouscarat F, et al. Tropical fish salesmen's knowledge and behaviour concerning "fish tank granuloma." Ann Dermatol Venereol. 2003. 130:425-7.
9. Laing RB. Antibiotic treatment of fish tank granuloma. J Hand Surg [Br]. 1997; 22:135-7.
10. Hiroko A, Hiroshi N, Ryukichi N. Mycobacterium marinum infection of the skin in Japan. J Dermatol. 1984;11:37-42.
11. Hautman G, Lotti T. Atypical mycobacterial infections of the skin. Dermatol Clin. 1994;12:657-68.
12. Aubry A, Chosidow O, Caumes E, Robert J, et al. Sixty-three cases of Mycobacterium marinum infection. Arch Intern Med. 2002;162:1746-1752.
13. Huminer D, Pitlik SD, Block C, Kaufman L, et al. Aquarium-borne Mycobacterium marinum skin infection. Arch Dermatol. 1986;122:698-703.
14. Weedon D. Skin Pathology, 2nd ed. St. Louis: Churchill Livingstone; 2002:628.
15. Tchornobay AM, Claudy AL, Perrot JL, Levigne V, Denis M. Fatal disseminated Mycobacterium marinum infection. Int J Dermatol. 1992;31:286-287.
16. Fitzpatrick TB, et al. Color Atlas & Synopsis of Clinical Dermatology, 4th ed. St. Louis: McGraw-Hill, 2001:667-668.
17. Ang P, et al. Retrospective study of Mycobacterium marinum skin infections. Int J Dermatol. 2000; 39:343.
18. Gombert ME et al. Disseminated Mycobacterium marinum infection after renal transplantation. Ann Intern Med. 1981;94:486-487.
19. Lee MW, Brenan J. Mycobacterium marinum: chronic and extensive infections of the lower limbs in South Pacific Islanders. Australas J Dermatol. 1998;39:173-176.
20. Posteraro B, Sanguinetti M, Garcovich A, et al. Polymerase chain reaction-reverse cross blot hybridization assay in the diagnosis of sporotrichoid Mycobacterium marinum infection. Br J Dermatol. 1998;139:872-876.
Address for Correspondence
Ran H. Bang MD
Department of Dermatology
University of New Mexico School of Medicine
1021 Medical Arts Avenue, N.E.
Albuquerque, New Mexico, 87102
Phone: 505-272-6000
Fax: 505-272-6003
e-mail: rbang@salud.unm.edu
Joseph P. Janik MD, Ran H. Bang MD, Charles H. Palmer MD
Department of Dermatology, University of New Mexico School of Medicine, Albuquerque, NM
COPYRIGHT 2005 Journal of Drugs in Dermatology, Inc.
COPYRIGHT 2005 Gale Group