Between 1987 and 1990, seven children presented with acute cerebellar symptoms and serologic evidence suggestive of recent varicella infection. The neurological symptoms lasted for 1 to 3 weeks. Symptoms resolved spontaneously in all patients without residual signs or symptoms during a 2- to 3-year follow-up.
Key words. Chickenpox; cerebellar ataxia; child; disease. (J Fam Pract 1995; 40:494-496)
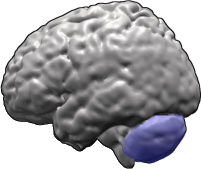
Neurological complications are relatively rare in chicken-pox.(1)(2)(3) Acute cerebellar ataxia is the most common, occurring in about one in 4000 varicella cases among children younger than 15 years of age.(1)
Acute varicella-associated cerebellar ataxia occurs primarily in children and is characterized by ataxia with nystagmus, headache, nausea, vomiting, and nuchal rigidity. The symptoms of varicella encephalitis may begin as early as 11 days before and up to 21 days after the onset of the rash.(4)
We describe seven children with acute cerebellar ataxia associated with varicella virus infection and review the pertinent literature.
Case Reports
Between 1987 and 1990, seven children presented with acute cerebellar ataxia. In one of the patients, ataxia preceded the development of varicella by 10 days. In six patients, the ataxia occurred 12 to 21 days after the onset of the varicella rash. Patient ages ranged from 2 to 6 years (Table).
[TABULAR DATA OMITTED]
Cerebellar symptoms consisted of truncal ataxia, intention tremor, and abnormal results on finger-to-nose and heel-to-shin tests. There was no clinical evidence of meningeal irritation, and mental status was normal. Cranial nerves, sensory findings, muscle strength, and muscle tone were all normal. None of the patients had myoclonus or opsoclonus. Cerebellar symptoms lasted between 7 and 20 days, resolving spontaneously in all patients. No residual neurological effects were observed during a 2- to 3-year follow-up. At the time of evaluation, all seven patients had serologic evidence of recent varicella infection, as indicated by the results of an enzyme-linked immunosorbent assay for IgM antibodies. All patients exhibited at least a fourfold increase in complement fixation antibodies (Table).
Lumbar puncture performed in all patients revealed pleocytosis (9 to 28 white blood cells [WBC]/[mm.sup.3]) with lymphocytic predominance. The protein and glucose determinations on all cerebrospinal fluids (CSF) were normal.
Patient 4 (Table) presented with an unusual case of varicella. He was brought to the hospital because of vomiting, lethargy, slurred speech, and difficulty in walking. The patient had been in excellent health until 2 days before admission. His brother had had varicella 2 weeks previously. The physical examination at admission revealed an irritable but cooperative child. His neck was supple. Brudzinski's and Kernig's signs were negative. A neurological examination revealed no abnormality of cranial nerves except for nystagmus upon lateral gaze to either side.
Finger-to-nose and heel-to-shin tests, as well as rapid alternating movements, suggested severe bilateral cerebellar dysfunction. There seemed to be a decrease in tone in all four extremities. Deep tendon reflexes were pendular in quality but symmetrical in both the upper and lower extremities. Fundi were normal. The rest of the physical and neurological examination was normal. A lumbar puncture performed at admission revealed clean, colorless spinal fluid under normal pressure, containing 24 WBC/m[m.sup.3], of which 75% were lymphocytes. The protein content was 18 mg/dL (0.18 g/L) (Table), and glucose content was 80 mg/dL (0.8 g/L).
Ten days after admission to the hospital, vesicles developed on the patient's arms, legs, and trunk. He began to improve neurologically as soon as the varicella skin lesions appeared. He became less lethargic and his ataxia diminished. A serum specimen drawn at admission had shown a varicella titer of 1:16; the titer was 1:128 on the day of his discharge 2 weeks later. At a follow-up examination 2 months later, he showed full neurological recovery. There was no serologic evidence of recent mumps, echovirus, coxsackievirus B, measles, rubella, or poliomyelitis.
Discussion
Acute cerebellar ataxia is a relatively common neurological disorder among children. Its association with a large variety of infectious agents has been described. These include varicella, echovirus type 9, Epstein-Barr virus, coxsackievirus B, poliomyelitis, measles, mumps and rubella, and mycoplasma pneumonias. Of these, varicella appears to be the pathogen most commonly identified.(5)(6)
Cerebellar ataxia accounts for more than one half of all the neurological complications of varicella-zoster virus (VZV) infection.(7) Acute varicella-associated cerebellar ataxia occurs primarily in children and is characterized by ataxia with nystagmus, headache, nausea, vomiting, and nuchal rigidity.(4)(7) The symptoms of varicella encephalitis may begin as early as 11 days before and up to 21 days after the onset of the rash.(2)(7)
Examination of CSF in varicella-associated cerebellar ataxia reveals nonspecific findings, with a cell count ranging from 0 to 68 cells/m[m.sup.3]. Lymphocytic pleocytosis and elevated protein may occur in 20% to 30% of the cases. The CSF glucose is normal, and polymorphonuclear cells may be present in the early course of the disease.(2)(7)(8) In complicated cases, an electroencephalogram (EEG), a computed tomography (CT) scan, and on some occasions, magnetic resonance imaging (MRI) are necessary. On the EEG, slow, diffuse wave activity has been noted in 20% of the cases(8); CT is usually normal, although MRI studies have revealed abnormalities, even in benign cases. In mild cases, no further evaluation is recommended.(8)
The neurological complications of varicella that precede or accompany the exanthematous manifestation are likely to be directly related to viral invasion of the nervous system. On the other hand, neurological complications that occur after the appearance of cutaneous lesions are most likely the result of a nonspecific, postinfectious autoimmune process.(6)(9) Although pre-eruptive neurological complications may occur, cerebellar symptoms are reported to precede the skin rash only in very rare cases. It is worth noting that most of these pre-eruptive patients were male and that the interval between the onset and the appearance of the eruption was relatively long (more than 10 days).(9)(10)(11)
Peters et a[l.sup.2] were the first to demonstrate the presence of varicella antigen in CSF cells by means of an immunofluorescent technique, suggesting direct invasion of the central nervous system in patients with acute cerebellar ataxia. Antibodies to VZV also have been demonstrated in the CSF of patients with varicella.(8)
The cerebellar manifestations of varicella are usually self-limited, mortality is low, and the majority of patients recover without sequelae.(8) It is a benign complication of VZV infection in children and does not generally require hospitalization. No specific therapy, eg, acyclovir, is indicated at this time for patients with central nervous system involvement caused by VZV.(8)(9)(10) In some patients with pre-eruptive varicella cerebellitis, polymerase chain reaction may be extremely useful for rapid confirmation of the diagnosis.(10)
The cerebellar symptoms in our patients were followed by complete neurological recovery. No residual neurological complications were noted during a 2- to 3-year follow-up, suggesting that acute varicella-associated cerebellar ataxia follows a benign, self-limited course.
References
(1.)Guess HA, Broughton DD, Melton LJ, Kurland LT. Populationbased studies of varicella complications. Pediatrics 1986; 78:723-7.
(2.)Peters AC, Versteeg J, Lindeman J, Bots GT. Varicella and acute cerebellar ataxia. Arch Neurol 1978; 35:769-71.
(3.)Jackson MA, Burry VJ, Olson LC. Complications of varicella requiring hospitalization in previously healthy children. Pediatr Infect Dis 1992; 11:441-5.
(4.)Straus SE, Ostrove JM, Inchauspe G, Felser JM, Freifeld A, Croen KD, Sawyer MH. Varicella-zoster virus infections: biology, natural history, treatment and prevention. Ann Intern Med 1988; 108: 221-37.
(5.)Bell WE. Ataxia in childhood--clinical approach and differential diagnosis. Lancet 1965; 2:85.
(6.)Dreyfus PM, Senter TP. Acute cerebellar ataxia of childhood: an unusual case of varicella. West J Med 1974; 120:161-3.
(7.)Johnson R, Milbourn PE. Central nervous system manifestations of chickenpox. Can Med Assoc J 1970; 102:831-4.
(8.)Scheld WM, Whitley RJ, Durack DT. Infections of the central nervous system. New York, NY: Raven Press, 1991:59.
(9.)Goldston AS, Millichap JG, Miller RH. Cerebellar ataxia with preeruptive varicella. Am J Dis Child 1963; 106:197-200.
(10.)Dangond F, Engle E, Yessayan L, Sawyer MH. Pre-eruptive varicella cerebellitis confirmed by PCR. Pediatr Neurol 1993; 9:491-3.
(11.)Takeuchi Y, Yoshihara T, Ishimuru K, Amano T, Kadomoto Y, Sawada T. Recurrent pre-eruptive acute cerebellar ataxia--a rare case of varicella. Pediatr Neurol 1987; 3:240-1.
From the Department of Pediatrics "C," Children's Medical Center of Israel, Petach Tikvah, Israel. Requests for reprints should be addressed to Moshe Nussinovitch, MD, Department of Pediatrics "C," Children's Medical Center of Israel, Petach Tikvah, Israel.
COPYRIGHT 1995 Dowden Health Media, Inc.
COPYRIGHT 2004 Gale Group