An increased level of colon lithocholic acid, a potential tumor promoter, accompanies a highfat diet. Lithocholic acid can bind to the intestinal vitamin D receptor and thereby induce the cytochrome CYP3A, which detoxifies lithocholic acid by catabolic reactions.
Key Words: bile acids, lithocholic acid, 1,25-dihydroxyvitamin D3, vitamin D receptor, cytochrome CYP3A, colon.
Epidemiologic studies have, with some exceptions, observed an association between high-fat diets and a high risk of colon cancer.1 Early theories as to the cause have suggested that free fatty acids, in their ionized state, could act as tumor promoters.2 Several epidemiologic studies have shown an inverse correlation between risk of colon cancer and calcium and vitamin D intake.3 Calcium ions were thought to convert the anionic fatty acids into neutral soaps and the vitamin would aid in increasing calcium uptake.4 A more direct action of vitamin D in suppressing tumor promotion in colon has also been suggested.5,6 It is of interest that the highest death rates of colon cancer occur in areas with a high incidence of rickets.3
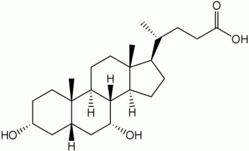
A high-fat diet is accompanied by an increased secretion of bile. For instance, a doubling of the excretion of bile acids in feces in healthy young men eating a high-fat diet was reported long ago. Experimentally, bile acids have been established as tumor promoters.8 Bile acids (Figure 1), the end products of cholesterol metabolism, are synthesized in the liver as cholic acid and chenodeoxycholic acid and secreted in bile conjugated with glycine and taurine (primary bile acids). Their function is to aid in the solubilization, digestion, and absorption of lipids in the gut. More than 95% of the bile acids are saved from loss in feces by the enterohepatic circulation, reabsorption in the ileum and return to the liver.1 The unabsorbed portion, representing in the human 20% of the bile acid pool, is metabolized by the colonic microflora to the secondary bile acids-first by deconjugation, then by oxidation-to deoxycholic acid, which is partly reabsorbed, and to lithocholic acid (LCA) (Figure 1), which is almost insoluble and not significantly reabsorbed. LCA represents approximately 5% of the total bile acid pool.1
LCA at a high concentration has been found to be a powerful tumor promoter,5 quite likely by inhibiting DNA repair enzymes.9 Vitamin D, in one of its active forms (la-hydroxyvitamin DO, inhibited the tumor-promoting action of LCA upon treatment of rats with the colon carcinogen N-methyl-N'-nitrosourea.5
LCA in the colon is detoxified by the P450 enzyme CYP3A, which oxidizes LCA to 3-ketolithocholic acid. 10 Experiments with intestinal cells in culture showed that the active form of vitamin D, 1,25-dihydroxyvitamin D3 (1,25(OH)2D3), when liganded to the vitamin D receptor protein (VDR) as a heterodimer with the receptor RXR, induced the expression of CYP3A. 11
In a recent report, Makishima et al. 12 tested the hypothesis that LCA might activate VDR, thereby inducing CYP3A and promoting the detoxification of LCA. The method the investigators used was a ligand-screening procedure developed by the same group. 13 The method makes use of the interaction of nuclear receptors with their coactivators. Upon binding to a ligand (e.g., 1,25(OH)2D3), the ensuing conformational change of the receptor increases its affinity for its coactivator. To determine which one of a number of receptors interacts with a particular ligand, transcriptional activity was assayed with a luciferase reporter gene. In particular, Makishima et al.12 fused the DNA of the receptor-interacting domain of the coactivator SRC- 1 to that of the DNAbinding domain of the yeast transcription factor GAL4. The gene of the nuclear receptor to be tested was fused to the transactivation domain of the herpes virus VP16 DNA. Then the expression plasmids for GALA-SRCI and the particular receptor-VP16 were transfected into human kidney cells in culture, together with the plasmid for the reporter, the GALA-responsive luciferase plasmid.
By screening a number of known nuclear receptors (including the VDR, the liver xenobiotic receptor PXR, the liver farnesoid receptor FXR, the RXR and RAR receptors, and others with LCA as ligand and SRC 1 as coactivator, investigators found that the only responsive receptors were the VDR and FXR (Figure 2). The FXR is a nuclear receptor from liver, where it senses bile acids and activates the "bile acid efflux pump," protecting the organism from excessive bile acid levels.14 The authors'2 also screened the array of nuclear receptors with another ligand, 1,25(OH)^sub 2^D^sub 3^, and found that it activated the VDR, as expected, but not FXR. Thus, the only receptor reacting with both LCA and 1,25(OH)2D3 is the VDR. Interestingly, the primary bile acids, though active as ligands for FXR, were quite ineffective in activating the VDR. Dose dependence experiments showed that LCA showed a median effective concentration of 8 (mu)M, well below the pharmacologic range. By means of competition experiments with [^sup 3^H]-1,25(OH)^sub 2^D^sub 3^, the authors 12 proved that LCA actually binds to the VDR.
Makishima's12 next step in support of the hypothesis was to demonstrate that LCA, when bound to the VDR could induce expression of the LCA-detoxifying enzyme, CYP3A. Thummel et al.11 had already shown that 1,25(OH)2D3 bound to the VDR could induce CYP3A in intestinal cells. Makishima et al.12 tested the hypothesis that LCA (instead of 1,25(OH)2D3) bound to the VDR could also induce CYP3A. They prepared [32p]-labeled oligonucleotides corresponding to the promoter regions of mouse, rat, and human CYP3A genes and, by means of electrophoretic mobility shift assays, showed that a VDR-RXR heterodimer bound to each of the CYP3A gene promoters. They then inserted the CYP3A-VDR response elements of the CYP3A genes into a luciferase reporter plasmid and transfected it, together with VDR and RXR expression plasmids, into HEK293 cells. They observed equally powerful activation of the CYP3A gene by adding either 1 nM 1,25(OH)2D3 or 10 nM LCA to the cells, thus confirming that the vitamin D derivative could induce CYP3A and proving that LCA could induce the enzyme that effects its own detoxification. The human CYP3A gene element was the most sensitive by responding most strongly to LCA.
In their final experiment, the authors'2 determined the in vivo response in mouse intestine to la-hydroxyvitamin D^sub 3^ (a substitute for 1,25(OH^sub )^2D^sub 3^) and to LCA. They fed mice by gavage with either the vitamin or the bile acid for 3 days and isolated intestinal mRNA for Northern blot analysis. Both the vitamin and the bile acid increased expression of CYP3A mRNA in intestine. The experiment "demonstrated that the VDR can function as an LCA sensor in vivo, resulting in increased expression of CYP3A ... and leading to detoxification of LCA."12
In summary, the work of Makishima et al.12 revealed the pivotal role played by the VDR in intestine (Figure 3): * Through binding the potentially harmful LCA, VDR induces the detoxifying enzyme CYP3A, which detoxifies LCA.
* Through binding the active form of vitamin D, 1,25(OH)^sub 2^D^sub 3^, VDR can also induce CYP3A, thus possibly explaining the antitumor-promoter activity of vitamin D.5,6
In its classical function, through binding 1,25(OH)2D3, VDR promotes the intestinal uptake of calcium and phosphate necessary for maintaining serum calcium and phosphate levels and bone mineralization.15
1. Nagengast FM, Grubben MAL, van Munster IP. Role of bile acids in colorectal carcinogenesis. Eur J Cancer 1995;31A:1067-70
2. Bull AW, Soullier BK, Wilson PS, et al. Promotion of
azoxymethane-induced intestinal cancer by high-fat diet in rats. Cancer Res 1979;39:4956-9
3. Garland CF, Garland FC, Gorham ED. Calcium and vitamin D: their potential role in colon and breast cancer prevention. Ann N YAcad Sci 1999;889:107-19
4. Newmark HL, Wargovich MJ, Bruce WR. Colon cancer and dietary fat, phosphate and calcium: a hypothesis. J Natl Cancer Inst 1984;72:1323-5
5. Kawaura A, Tanida N, Sawada K, et al. Supplemental administration of 1 a-hydroxyvitamin D3 inhibits promotion by intrarectal instillation of lithocholic acid in N-methyl-N-nitrosourea-induced colonic tumorigenesis in rats. Carcinogenesis 1989;10:647-9
6. Mehta RG, Mehta RR. Vitamin D and cancer. J Nutr Biochem 2002;13:252-64
7. Cummings JH, Wiggins HS, Jenkins DJ, et al. Influence of diets high and low in animal fat on bowel habit, gastrointestinal transit time, fecal microflora, bile acid and fat excretion. J Clin Invest 1978;61: 953-63
8. Narisawa T, Magadia NE, Weisburger JH, Wynder EL. Promoting effect of bile acids on colon carcinogenesis after intrarectal instillation of N-methyl-N'nitro-N-nitrosoguanidine in rats. J Nati Cancer Inst 1974;53:1093-7
9. Ogawa A, Murate T, Suzuki M, et al. Lithocholic acid, a putative tumor promoter inhibits mammalian DNA polymerase beta. Jpn J Cancer Res 1998;89:1154-9
10. Araya Z, Wikvall K. 6-Alpha-hydroxylation of taurochenodeoxycholic acid and lithocholic acid by CYP3A4 in human liver microsomes. Biochim Biophys Acta 1999;1438:47-54
11. Thummel KE, Brimer C, Yasuda K, et al. Transcriptional control of intestinal cytochrome P4503A by 1-alpha-25-hydroxyvitamin D3. Mol Pharmacol 2001;60:1399-406
12. Makishima M, Lu TT, Xie W, et al. Vitamin D receptor as an intestinal bile acid sensor. Science 2002;296: 1313-6
13. Makishima M, Okamoto AY, Repa JJ, et al. Identification of a nuclear receptor for bile acids. Science 1999;284:1362-5
14. Chawla A, Repa JJ, Evans RM, Mangelsdorf DJ. Nuclear receptors and lipid physiology: opening the X-files. Science 2001;294:1866-70
15. Jones G, Strugnell SA, DeLuca HF. Current understanding of the molecular actions of vitamin D. Physiol Rev 1998;78:1193-231
This review was prepared by George Wolf, D.Phil., Department of Nutritional Sciences and Toxicology, University of California, Berkeley, CA 94720-3104, USA. Please address all reprint requests to the Nutrition Reviews Editorial Office, 711 Washington Street, Boston, MA 02111, USA.
Copyright International Life Sciences Institute and Nutrition Foundation Sep 2002
Provided by ProQuest Information and Learning Company. All rights Reserved