Backgrouud & objectives: The emergence of antibiotic-resistant bacteria is a phenomenon of concern to the clinician as well as to the pharmaceutical industry, because it is the major cause of failure in the treatment of infectious diseases. The genetic exchange of plasmids containing antibiotic resistant determinants (R-plasmids) between organisms of the same or different species is believed to play a crucial role in the evolution of antibiotic resistant bacteria. Staphylococcus aureus is well known for its multi-drug resistance (MDR). This work was undertaken to study the intraspecies transfer of a chloramphenicol (C) resistance staphylococcal R-plasmid among different clinical isolates of S. aureus.
Methods: From a MDR S. aureus MC524 strain, a small plasmid pMC524/MBM was isolated. Lysostaphin lysis and sucrose mediated detergent lysis were used for plasmid preparation. Agarose gel electrophoresis, transformation experiments, Southern blotting and hybridization were done. Restriction cndonuclease (RE) digestions were performed.
Results: pMC524/MBM, which codes for C resistance could be transferred into some C sensitive clinical strains of S. aureus. The size and the RE digestion patterns of the plasmids isolated from the S. aureus transformants were identical to those of pMC524/MBM.
Interpretation & conclusion: These results suggest that pMCS24/MBM, without any modification is capable of transferring, maintaining, replicating and expressing itself in different clinical strains of S. aureus and hence may be responsible for the spread of C resistance.
Key words Antibiotic resistance plasmid - chloramphenicol resistance plasmid - intraspecies plasmid transfer plasmid transformation - staphylococcal plasmid
The development and spread of bacterial strains that are resistant to antibacterial drugs has emerged as a global problem1. The transmission of antibiotic resistance genes from streptomycetes and other soil bacteria to clinically important species may have occurred through the exchange of antibiotic resistance plasmids (R-plasmids) or transposons during the last 50 yr of widespread antibiotic use and therapy2. The appearance of antibiotic resistant bacteria over the past decades has been regarded as an inevitable genetic response to the strong selective pressure imposed by antimicrobial chemotherapy, which plays a crucial role in the evolution of antibiotic resistant bacteria. These bacteria then pass the antibiotic resistance plasmid among other bacterial cells and species3.
With a view to understand the spread of antibiotic resistance in bacteria, we studied the antibiotic resistance plasmid of Staphylococcus aureus, a Gram positive pathogen responsible for 9 to 10 per cent of all nosocomial infections world-wide4,5. More than 51 per cent of all S. aureus isolates from clinical sources from Kolkata were found to be multiple antibiotic resistant6. Plasmid mediated antibiotic resistance in S. aureus has been reported from many laboratories7-11.
We isolated a multiple antibiotic resistant clinical S. aureus strain MC524, resistant to ampicillin (A), chloramphenicol (C), kanamycm (K) and streptomycin (S), which possessed a single plasmid and we designated this as pMC524/MBM12. In this paper, we report some of the characteristics of this plasmid, and its capability to transfer itself to different clinical strains of S. aureus.
Material & Methods
Bacterial strains: S. aureus MC524 (phage type 47,95 RTD) strain was isolated from a sample of pus from an indoor patient admitted to the Calcutta Medical College & Hospital (CMCH), Kolkata in 1996. Other chloramphenicol sensitive plasmidless clinical strains of S. aureus were collected from CMCH, Nil Ratan Sarkar Medical College, Bangur Hospital, RG Kar Medical College and School of Tropical Medicine, Kolkata. The investigations using these strains were carried out in the section of Microbiology, Department of Physiology, University of Calcutta, during 1996-2002. S. aureus RN4220, a plasmidless, all antibiotic sensitive and restriction deficient strain and a derivative of S. aureus NCTC 8325 suitable as a transformation host13 was a gift from Dr Richard P. Novick, Skirball Institute, New York, USA.
Media & chemicals: The S. aureus strains were maintained on TSBYEG medium [3% Trypticase soya broth (TSB, Hi-media, India), 0.3% yeast extract (Oxoid Ltd, UK) and 0.5% glycine (Sigma, USA)].
For S. aureus protoplast transformation, Penassay (PA) broth [0.368 g K^sub 2^HPO^sub 4^ (Merck, India), 0.132 g KH^sub 2^PO^sub 4^ (Merck, India), 0. 15 g yeast extract, 0.5 g bactopeptone (Difco Lab, USA), 0.35 g sodium chloride (Qualigens Fine Chemicals, India), 0.1 g dextrose (Sarabhai M Chemicals, India), 0.15 g beef extract (SD Fine Chemicals Ltd, Bolsar), water 100ml, pH 7] was used. S. aureus transformants were selected on DM3 regeneration medium containing 135 g/l sodium succinate (Sisco Research Lab Pvt Ltd, India), 5 per cent w/v casamino acids (100 ml/l, Difco, USA), 20 per cent w/v glucose (25 ml/l, BDH Lab, India), 10 per cent w/v BSA (10 ml/l, Sigma, USA), agar (8 g/l, Merck, India), and the volume made to 1000 ml with water. Sodium succinate was used as an osmotic stabilizer. Antibiotics were adcted as required.
Antibiotic susceptibility pattern: Determination of susceptibility of the donor and the transformant strains to 8 different antibiotics, i.e., A, C, S, K, erythromycin (E), gentamycin (G), methicillin (M) and tetracyclin (T) was determined by the disc agar diffusion technique (DAD)14. Minimum inhibitory concentration (MIC) of different antibiotics was determined by the serial 2-fold broth dilution method15. Both DAD and MIC were determined in Muller Hinton Broth (MHB, Hi-media, India). A, C, S, K, E, G were products of Sigma, USA, M and T were gifts from Dr M.K. Mazumdar, ex-Director, Central Drug Laboratory, Kolkata.
Plasmid isolation: Plasmid DNA from S. aureus was isolated both by lysostaphm lysis16 and sucrose mediated detergent lysis methods17.
Restriction endonuclease (RE) digestion: The plasmids were digested with BamH I, EcoR I, Hind III and Pst I (Bangalore Genei), according to the instructions of the manufacturers.
Protoplast transformation: Transformation of S. aureus RN4220 (a restriction modification minus plasmidless strain suitable for transformation) was performed by the protoplast transformation method with slight modification18. The host S. aureus RN 4220 was grown in 2xPA broth to mid log phase (5x10^sup 8^ cells/ml) and protoplasts were prepared by incubating the mid log phase cells with lysostaphin (Sigma, USA) at 37[degrees]C for 20 min, stabilized with sucrose (Qualigens Fine Chemicals, India) and Mg^sup +2^. For transformation, 30-40 ng of plasmid DNA in a volume of 0.25 ml was mixed with an equal volume of SMM [sucrose 324 g/l, sodium maleate 4.6 g/l and MgCl^sub 2^ 8.1 g/l (Qualigens Fine Chemicals, India)], 0.5 ml of protoplast suspension was added and the mixture was shocked with polyethelene glycol (PEG, Sigma, USA). Protoplasts were plated onto DM3 regeneration medium containing the appropriate antibiotic and incubated at 37[degrees]C. Colonies began to appear after 48 h. In this study A, C. S or K containing DM3 medium was used.
Southern blotting and hybridization: Plasmid DNA was electrophoresed on 0.8 per cent w/v agrose gel (Sigma, USA) in Tns-Borate-EDTA (TBE) buffer (Sigma, USA), and then transferred to Hybond membrane (Amersham, USA)19. pMC524/MBM was radioactively labelled with [[alpha] ^sup 32^P] - dCTP (Bhaba Atomic Research Centre) by the random priming method using GIBCO BRL Random Primers Labelling System20. Prehybridization was carried out at 65[degrees]C. Subsequent washings and signal development were done following the method of Sambrook et al21.
Results
S. aureus MC524 was resistant to A, C, K and S by the disc agar diffusion technique. Its MIC value for chloramphemcol in MHB, was found to be 125 [mu]g/mi.
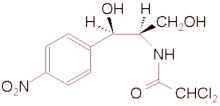
Plasmid analysis of S. aureus MC524 revealed that it harboured a small plasmid. designated as pMC524/MBM. This plasmid has a single cutting site for Hind III, but no cutting sites for EcoR I, BamH I or Pst I. Fig. 1 shows the RE digestion pattern of pMC524/MBM. Lane 2 in Fig.1 shows linearised form of pMC524/MBM due to single cut by Hind III.
Transformed S. aureus RN4220 clones with plasmid pMC524/MBM were selected on DM3 plates containing 30 [mu]g/ml C. Transformation frequency was 1.3x10^sup 4^ transformants per [mu]g of pMC524/MBM DNA. No transformants were found, on DM3 plates containing either A or K or S. It was thus concluded that pMC524/MBM codes for chloramphenicol resistance.
Ten, chloramphenicol sensitive, plasmidless clinical isolates of S. aureus different from each other as established by phage typing were procured from different Kolkata hospitals stocks, and attempts were made to transform these strains with pMC524/MBM following the protoplast transformation method. In seven of the 10 strains, chloramphenicol resistant transformants appeared. Plasmid preparations from these transformants revealed the presence of a small plasmid. Both the electrophoretic mobility (Fig. 2) and RE digestion pattern of these plasmids were identical to those of pMC524/MBM. As pMC524/MBM is a small plasmid the electrophoretic mobility of pMC524/MBM along with the plasmids obtained from two of the transformants, were compared to that of pBR 322 (Fig. 3). Antibiotic susceptibility testing by the disc agar diffusion technique showed that S. aureus MC524 (donor) was resistant to A, K, C and S, while the S. aureus RN4220/524 transformants and all the transformed clinical isolates were resistant to chloramphenicol only. Plasmids prepared from these transformants, were electrophoresed, blotted and hybridized with radioactively labelled pMC524/MBM. pMC524/MBM hybridized with each plasmid prepared from chloramphenicol resistance transformed clinical isolates indicating strong DNA homology of pMC524/MBM with the plasmid present in the transformed strains. The MIC for chloramphenicol for these transformants was determined and found to be 125 [mu]g/ml. The value was same as that of the original plasmid donor strain S. aureus MC524. pMC524/MBM was found to be stable in its original host S. aureus MC524 in the presence of chloramphenicol. The plasmid found in all the transformed clinical strains of S. aureus also need chloramphenicol for its stable maintenance.
Discussion
The most important means of the spread of antibiotic resistance in major bacterial species is by conjugation through the resistant genes residing on plasmids8,11. Plasmid mediated drug resistance was first demonstrated by Japanese workers in Shigella species2. Inactivation of chloramphenicol by Escherichia coli was reported first in 1967(22). Results obtained in this study suggest that pMC524/MBM, a native staphylococcal plasmid of size 2.889 kb23 bearing a chloramphenicol resistant gene, is capable of transferring and expressing itself, in some clinical strains of S. aureus without any alteration during the course of transfer. The MIC values of cholamphemcol, for S. aureus MC524 and different S. aureus transformants indicate that the plasmid is efficiently expressed in S. aureus transformants.
The spread of resistance via conjugative (intraspecies, interspecies and mtergeneric) plasmids of 17 to 20 megadaltons that code for chloramphenicol and other antibiotics was found in Streptococci24. Interspecies plasmid transfer between Bacillus subtilis and other Bacillus species was reported from Amherst, Massachusetts in 1987(25). A 3.2 kb plasmid (WBG1022), encoding chloramphenicol resistance was isolated from S. aureus in Perth, Australia, which could be transferred in mixed culture26. Report of co-transfer of a non-conjugative 3.5 kb chloramphenicol resistance plasmid along with a conjugative plasmid pXU10 is found11. Spread of methicillin resistance via plasmid, from one strain of S. aureus to another in mixed culture was noticed in 1999 in Poland27. In our study, the plasmid isolated was of much smaller size (2.889 kb) than reported by other workers in this field.
Under different conditions with antibiotic selection pressure, the resistant determinants are picked up by different bacteria, specially in the hospital environment, as survival measures and thus becomes an important factor in the dissemination of antibiotic resistance. Our results provide evidence that pMC524/MBM, a native staphylococcal chloramphenicol resistant plasmid, is capable of expressing itself in different S. aureus clinical isolates, without undergoing any modification or alteration during this process of mtraspecies transfer through transformation. The sequencing of the plasmid revealed that it has a size of 2.889 kb23. In most instances reported so far the transfer of plasmid mediated antibiotic resistance is conjugational transfer8,11,28,29, but our study reports nonconjugalional transfer of chloramphenicol resistance.
With the strong antibiotic selection pressure in hospital environments, this type of small plasmid probably causes rapid emergence and spread of antibiotic resistance in other hospital pathogens.
Acknowledgment
The authors are grateful to Dr R.P. Novick, Skirball Institute, New York, USA, for gift of S. aureus strain RN 4220. Authors thank the Staphylococcal Phage Typing Centre, Maulana Azad Medical College, New Delhi for phage typing of S. aureus strains. Thanks are due to Prof. Uma Dasgupta, Department of Molecular Biology and Biophysics, University of Calcutta, Kolkata for radioactive hybridization studies. The partial financial assistance from the University Grants Commission (UGC) and Council of Scientific and Industrial Research (CSIR), New Delhi, is acknowledged.
References
1. Cohen ML. Epidemiology of drug resistance: implications for a post-antimicrobial era. Science 1992; 257 : 1050-5.
2. Davies J. Inactivation of antibiotics and the dissemination of resistance genes. Science 1994; 264 : 375-82.
3. Walsh C. Molecular mechanisms that confer antibacterial drug resistance. Nature 2000; 406 : 775-81.
4. Ruben FL, Norden CW. Staphylococcal infections. In: Evans AS, Feldman HA, editors. Bacterial infections of humans: epidemiology and control. New York : Plenum Medical Book Company; 1982 p. 511-24.
5. Bradley SF. Staphylococcus aureus infections and antibiotic resistance in older adults. Clin Infect Dix 2002; 34: 211-6.
6. Ray B, Bal M. Studies on the antibiotic sensitivity pattern and [beta]-lactamases of clinical isolates of Staphylococcus aureus. In: Chakravarty AN, Dastidar SG, editors. Proceeding Sixth National Congress. Indian Association of Medical Microbiology. Calcutta: Image India; 1984 p. 154-8.
7. Lacey RW. Antibiotic resistance plasmids of Staphylococcus aureus and their clinical importance. Bacterial Rev 1975; 39 : 1-32.
8. McDonnell RW, Sweeney HM, Cohen S. Conjugational transfer of gentamicin resistance plasmids intra- and interspecifically in Staphylococcus aureus and Staphylococcus epidermidis. Antimicrob Agents Chemother 1983; 23 : 151-60.
9. Mitra M, Chakrabarty AN, Mitra A, Dastidar SG. Transformation for antibiotic resistance and haemolysin production markers in Staphylococci. Indian J Exp Biol 1985; 23 : 585-7.
10. Archer GL, Coughter JP, Johnston JL. Plasmid-encoded trimethoprim resistance in Staphylococci. Antimicrob Agents Chemother 1986; 29 : 733-40.
11. Udo EE, Jacob LE, Mokadas RM. Conjugative transfer of high-level mupirocin resistance from Staphylococcus haemolyticus to other Staphylococci. Antimicrob Agents Chemother 1997; 41 : 693-5.
12. Bal M. Antibiotic resistant factors of Staphylococcus aureus. In : Roychoudhury A, editor. Proceedings of the twelfth annual conference of physiological society of India. Calcutta: Physiological Society of India; 2000 IL2, A6-A7.
13. Kreisworth BN, Lofdahl S, Betley MJ, O'Reilly M, Schlievert PM, Bergdoll MS, el al. The toxic shock syndrome exotoxin structural gene is not delectably transmitted by a prophage. Nature 1983; 305 : 709-12.
14. National Committee for Clinical Laboratory Standards. Performance standards for antimicrobial susceptibility testing. NCCLS approved standards. M100-S9. National Committee for Clinical Laboratory Standards, Wayne, Pennsylvania. 1999.
15. Ericsson UM, Sherris JC. Antibiotic sensitivity testing: report of an international collaborative study. Acta Pathol Microbiol Scand Section B. 1971; 217 (suppl) : 65-7.
16. Novick RP. Genetic systems in Staphylococci. Methods Enzymol 1991; 204 : 587-636.
17. Saha B, Saha D, Niyogi S, Bal M. A new method of plasmid DNA preparation by sucrose-mediated detergent lysis from Escherichia coli (Gram-negative) and Staphylococcus aureus (Gram-positive). Anal Biochem 1989; 176 : 344-9.
18. Chang S, Cohen SN. High frequency transformation of Bacillus subtilis protoplasts by plasmid DNA. Mol Gen Genet 1979; 168 : 111-5.
19. Southern EM. Detection of specific sequences among DNA fragments separated by gel electrophoresis. J Mol Biol 1975; 98 : 503-17.
20. Feinberg AP, Vogelstein B. A technique for radiolabeling DNA restriction endonuclease fragments to high specific activity. Anal Biochem 1983; 132 : 6-13.
21. Sambrook J, Fritsch EF, Maniatis T. Hybridization of radiolabelled probes to nucleic acids immobilized on nitrocellulose filters or nylon membranes. In : Molecular cloning, A laboratory manual, 2nd ed. Cold Spring Harbor, New York : Cold Spring Harbor Laboratory Press; 1989 p. 9.52-9.58.
22. Shaw WV. The enzymatic acetylation of chloramphenicol by extracts of R factor-resistant Escherichia coli. J Biol Chem 1967; 242 : 687-93.
23. Bal M. Staphylococcus aureus plasmid pMC524/MBM including cat gene for choramphenicol acetyl transferase and rep gene for replication protein. EMBL-EBI 2002; EMBL Accession No. AJ3 12056 SAU3 12056.
24. Horaud T, Le Bouguenec C, Pepper K. Molecular genetics of resistance to macrolides, lincosamides and streptogramin B (MLS) in Streptococci. J Antimicrob Chemother 1985; 16(Suppl A) : 111-35.
25. Koehler TM, Thorne CB. Bacillus subtilis (Natto) plasmid pLS20 mediates interspecies plasmid transfer. J Bacteriol 1987; 169 : 5271-8.
26. Udo EE, Grubb WB. Transfer of plasmid-borne resistance from a multiply-resistant Staphylococcus aureus isolate, WBG 1022. Curr Microbiol 1995; 31 : 71-6.
27. Mlynarczyk A, Mlynarczyk G, Jeljaszewicz J. Genetic transfer of methycilline resistance in Staphylococcus epidermidis and Staphylococcus aureus strains in mixed cultures. Med Dosw Mikrobiol 1999; 51 : 199-205.
28. Lyon BR, Skurray R. Antimicrobial resistance of Staphylococcus aureus : genetic basis. Microbiol Rev 1987; 51 : 88-134.
29. Projan SJ, Novick RP. Incompatibility between plasmids with independent copy control. Mol Gen Genet 1986; 204 : 341-8.
Mausumi Bhakta*, Suranjana Arora & Manjusri Bal
Section of Microbiology, Department of Physiology, University College of Science & Technology University of Calcutta, Kolkata, India
Received November 6, 2002
* Present address: Hooghly Mohsin College, Hooghly, West Bengal
Reprint requests : Dr Manjusri Bal, Section of Microbiology, Department of Physiology, University College of Science & Technology, University of Calcutta, 92 APC Road, Kolkata 700009, India
Copyright Indian Council of Medical Research Apr 2003
Provided by ProQuest Information and Learning Company. All rights Reserved