OBJECTIVE: Ambient-temperature storage of urine samples would increase the variety of life sciences studies that could be performed during spaceflight. The purpose of this study was to evaluate a preservative that would reduce the effects of oxidation and bacterial contamination on sample integrity and would be safe for personnel.
DESIGN: Chlorhexidine, a topical antiseptic, and n-propyl gallate, an antioxidant used in food production, were used in combination to produce a preservative (CPG) that meets these criteria. Urine pools were prepared and divided into three aliquots that were stored unpreserved at either -70 °C or room temperature (21 °C to 25 °C), or stored preserved with CPG at ambient temperature. Analyte measurements were conducted on days 1, 14, and 28, and monthly thereafter for one year. Stability was defined as the ability of a test condition to result in analyte values within the acceptable range established with the reference condition (-70 °C).
RESULTS: CPG effectively maintained stability of ammonia for 14 days, total nitrogen and 3-methylhistidine for three months, chloride for four months, sodium for five months, potassium for seven months, and urea for 12 months. Creatinine and osmolality were not preserved by CPG.
CONCLUSION: These data indicate that CPG offers prolonged room-temperature storage for multiple urine analytes, reducing the requirements for frozen urine storage on future spaceflights. In medical applications on Earth, this technology can allow urine samples to be collected in remote settings and eliminate the need to ship frozen samples.
ABBREVIATIONS: chlorhexidine/n-propyl gallate; CPG; first morning void; FMV.
INDEX TERMS: ambient temperature; urine preservative; urine storage.
Volume, mass, and power constraints severely limit frozen storage for biological samples collected during spaceflight. Identifying a means of preserving urine analytes stored at ambient temperature would lessen the impact of these limitations on biomedical research and crew health monitoring. Several urine preservatives, e.g., boric acid, hydrochloric acid, or thimerosal, are used clinically to preserve one or more analytes. Ideally, preservatives must provide stability for multiple analytes while minimizing hazard exposure for personnel. This is especially critical during spaceflight. Strong acids, such as hydrochloric or acetic acid, are not available for use during flight due to the safety hazard they pose to the crew. Additionally, strong acids tend to alter pH, with a resultant negative effect on other analytes.1,2 Dilute solutions of boric acid pose little risk to crewmembers, but preserve very few analytes for extended periods.3 Both thymol and thimerosal have been used to preserve urine samples on Space Shuttle missions, but require special handling to protect ground personnel when stock reagents are used to fill sample tubes.4
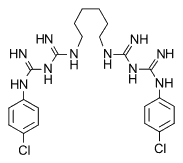
Two potential causes of analyte destruction in urine are bacterial contamination and oxidation.1,5 Consequently, we designed a urine preservative that would be relatively safe for personnel and would eliminate or reduce bacterial contamination and oxidation without altering sample pH. The urine preservative we formulated, designated CPG, is a chemical compound composed of equal parts of chlorhexidine gluconate and n-propyl gallate. Chlorhexidine gluconate is a water-soluble bacteriostatic agent that is used as both a urine preservative and a topical anti-infectant.6 The commercial food additive n-propyl gallate was chosen for its antioxidant properties. The FDA has deemed both chemicals safe for human use at the concentrations we report here.7,8 A 12month storage study was conducted to evaluate the ability of CPG to preserve multiple analytes in urine samples.
METHODS
Materials
CPG (U.S. patent #6,261,844) was prepared in two stages. First, a 20% solution of n-propyl gallate (Sigma Chemical Co, St Louis MO) was prepared by dissolving one gram of n-propyl gallate in five mL of absolute methanol. Equal volumes of chlorhexidine gluconate (20%, Sigma Chemical Co, St Louis, MO) and n-propyl gallate were combined to form the working preservative solution (CPG). Appropriate amounts of this solution were added to samples to yield a final concentration of 0.4 mg CPG/mL urine.
Sample collection and preparation
Pools representing first morning voids (FMV) and 24-hour (24-h) collections were obtained to verify analyte stability for the two most common time periods of urine collection. Male and female volunteers (n = 32) collected their first urine void of the morning. These samples were pooled and stored at 2 °C to 8 °C while awaiting further processing (
All samples were processed within two hours after collection was completed. Lithium chloride, a urine volume marker used during space missions, was added to the 24-h collection pool. Each pool was divided into three aliquots and a sufficient quantity of CPG was added to one aliquot to yield a final concentration of 0.4 mg CPG/mL of urine. All aliquots were further divided into 14 replicates, one for each day of testing (days 1, 14, and 28, and monthly through one year), and were designated -70 °C (reference storage temperature), RT (room temperature, 21 °C to 25 °C), or CPG (room temperature with CPG). Analyte, e.g., sodium, potassium, and ammonia, aliquots were prepared for each of the 14 replicates, and for each of the three storage conditions. On measurement days, frozen samples were thawed and all samples were mixed well prior to analysis.
Analytical methods
Standard clinical laboratory methods were employed to analyze samples. Urinary sodium and potassium were measured by ion-specific electrode techniques, chloride by silver chloride electrode, and creatinine by the Jaffe reaction on the Astra4 analyzer (Beckman Instruments, Anaheim CA). Urinary urea nitrogen and ammonia were analyzed enzymatically on the CX5 analyzer (Beckman Instruments, Anaheim CA). Osmolality was analyzed by freezing-point depression technology (Fiske Associates, Norwood MA) and 3-methylhistidine was analyzed by ion-exchange chromatography using the Beckman 6300 amino acid analyzer (Beckman Instruments, Anaheim CA). Total nitrogen was measured by pyrochemiluminescence (Antek Instruments, Houston TX). The accuracy and precision of each method were verified on days of analysis by measuring samples of known concentration.
Statistical analysis
Performance of the -70 °C stored sample was used as the reference condition to evaluate stability. The mean and standard deviation (SD) were calculated for each analyte on data obtained from samples stored under the reference condition. Outliers, defined here as values outside of ±3 SD of the mean, were removed and the acceptable range (mean ±2 SD) was determined for the reference condition. Precision was determined by calculating the percent coefficient of variation (CV) for each analyte.
Stability was defined as the ability of the test condition to maintain analyte values within the acceptable range. Two criteria were used to determine the length of analyte stability. First, if values fell outside the ±2 SD range for two consecutive test periods, the length of stability was assigned to the time period when the last acceptable test result was obtained. second, when stability data varied between first morning void and 24-hour pools for a particular analyte, the shorter of the two time periods was considered the cut-off point.
Regression analyses were performed to evaluate each storage condition for degradation trends. Correlation coefficients with p values less than 0.05 were considered to demonstrate statistically significant degradation trends. Statistical analyses were performed using Excel (Microsoft Corp, Cambridge MA), SAS (SAS Institute, Cary NC), and Sigma Stat (Jandel Scientific Inc, San Rafael CA) software.
RESULTS
Outliers in the reference condition data set were identified for the following analytes: urea 24-h day 28 (-7.1 SD), creatinine FMV day 28 (+3.3 SD), sodium FMV day 28 (+3.4 SD), chloride FMV day 28 (+3.3 SD), and osmolality FMV day 28 (+3.2 SD). These values were eliminated before the acceptable ranges were calculated. Resultant acceptable ranges and CVs for the reference condition are shown in Table 1.
Deviations from the reference mean for each stable analyte are depicted in Figure 1. In general, analyte values obtained from the first morning void pool were the limiting factors when determining stability. Lengths of stability for the CPG-preserved urine analytes are listed in Table 2. Urine pH remained stable in the CPG-preserved samples (FMV: 6.42 ± 0.18; 24-hr: 6.50 ± 0.24), but increased within 24 hours in the unpreserved samples (FMV: 9.04 ± 1.6; 24-hr: 8.70 ± 2.0). Unpreserved urine stored at ambient temperature remained within acceptable limits through month seven for urea nitrogen and month two for total nitrogen and 3-methylhistidine. Standard deviations were within acceptable limits for sodium and potassium in unpreserved urine stored at ambient temperature for three and five months, respectively, while chloride remained stable for only 28 days. Specimens stored unpreserved at ambient temperature yielded unacceptable standard deviations for pH, ammonia, creatinine, and osmolality.
Regression analyses to assess degradation trends were performed on the portion of each analyte curve that met acceptability requirements. The results are listed in Table 2. Statistically significant degradation over time was noted for both potassium and chloride in the CPG-preserved specimens; however, this degradation never reached the level of clinical significance.9
DISCUSSION
Data from this study indicate that CPG effectively provides a safe method for ambient-temperature storage of urine without altering pH. The length of ambient storage examined in this study is suitable for spaceflight, although stability for one to two weeks would suffice for ground-based analyses.
While ammonia levels remained stable for 14 days in CPG-preserved urine, the levels increased rapidly in unpreserved samples stored at ambient temperatures. It is interesting to note that the urea concentration in unpreserved urine decreased only slightly prior to month eight. Previous studies have indicated that decreases in urea levels, with concurrent increases in ammonia concentration, would be expected to occur in the absence of a bacteriostatic agent if urea-splitting bacteria were present in the samples.10-12 The concentration of 3-methylhistidine decreased more rapidly in the unpreserved samples, while remaining stable for three months in urine samples containing CPG. These findings suggest that the breakdown of amino acids in the urine as well as some urea degradation contributed to the rapid increases in ammonia concentration in unpreserved urine.13 Historically, urine samples for ammonia analysis have been analyzed immediately, or acidified and either refrigerated or frozen to preserve sample integrity. This study indicates that CPG is the preservative of choice for ambient-temperature storage of urinary ammonia, urea, and 3-methylhistidine.
Urinary sodium, potassium, and chloride tended to increase over time in both the unpreserved and CPG-preserved samples, while total nitrogen concentrations were erratic. It remains unclear why urinary electrolytes were less stable in the unpreserved urine samples than in CPG-preserved samples. One possible explanation is that previously bound electrolytes became free over time, increasing more rapidly with the elevated pH levels found in the unpreserved samples. Differences in the matrix effects of unpreserved and CPG-preserved samples may also have contributed to the loss of stability for these analytes. Nonetheless, urine specimens for total nitrogen and electrolyte measurements can be safely stored at ambient temperature for three and four months, respectively, with CPG as a preservative.
The National Committee for Clinical Laboratory Standards has established guidelines for the development and credentialing of clinical laboratory methods.14 However, voluntary consensus standards are not available for determining analyte stability in biological samples. The evaluation criterion used in this study assures accuracy within clinically significant ranges.9
CPG combines both bacteriostatic and antioxidant properties to provide a safe and reliable method for long-term ambient-temperature storage of urine. During past space shuttle and space station missions, restrictions in freezer space and power requirements have limited the scientific data obtained during spaceflight. Furthermore, failures of the flight freezer system have, on occasion, compromised scientific data. CPG offers the advantage of prolonged room-temperature storage for multiple urine analytes and, therefore, may reduce the requirements for frozen urine storage on future spaceflights. This technology can be carried over into the medical community by allowing patients the convenience of collecting urine samples in their homes and mailing aliquots to the physician's office or laboratory for testing. In addition, this preservative will allow urine samples to be collected in remote settings throughout the world, where dry ice, the traditional method for transporting frozen samples, is unavailable.
ACKNOWLEDGMENTS
This work was funded by NASA. CPG is covered under U.S. Patent No 6,261,844. The authors wish to thank the Johnson Space Center Nutritional Biochemistry Laboratory and Clinical Laboratories for their support in completing the analytical measurements reported here.
REFERENCES
1. Griffith DP, Dunn D. Collection and preservation of urine for biochemical analyses. Invest Urol 1978;15:459-61.
2. Nicar MJ, Hsu MC, Johnson T, Pak C. The preservation of urine samples for determination of renal stone risk factors. Lab Med 1987;18(6):382-4.
3. Henry JB, Kurec AS. The clinical laboratory: organization, purposes, and practice. In: Henry JB, editor. Clinical diagnosis and management by laboratory methods 19th ed. Philadelphia: WB Saunders Co; 1996. p 22-4.
4. Whitson PA, Pietrzyk RA, Pak CYC. Renal stone risk assessment during space shuttle flights. J Urol 1997;158:2305-10.
5. Chalmers AH, Cowley DM, McWhinney BC. Stability of ascorbate in urine: relevance to analyses for ascorbate and oxalate. Clin Chem 1985;31(10):1703-5.
6. Hodgkinson A. Sampling errors in the determination of urine calcium and oxalate: solubility of calcium oxalate in HCl-urine mixtures. Clin Chim Acta 1981;109:239-44.
7. United States Food & Drug Administration. Electronic orange book approved drug products with therapeutic equivalence evaluations. http:/ /www.fda.gov/cder/orange/default.htm. Accessed January 2003.
8. Code of Federal Regulations, Title 21, Volume 3, Parts 170-99. 21CFR184.1660. U.S. Government Printing Office, 1998:509-10.
9. Copeland BE. Quality control. In: Kaplan LA, Pesce AJ, editors. Clinical chemistry theory, analysis, and correlation. 2nd ed. St Louis: CV Mosby; 1989. p 310-37.
10. Ramadan MA, Tawfik AF, El-Kersh TA, Shibl AM. In vitro activity of subinhibitory concentrations of quinolones on urea-splitting bacteria: effects on urease activity and on cell surface hydrophobicity. Infect Dis 1995;171:483-6.
11. Rodman JS. Struvite stones. Nephron 1999;81(suppl 1):50-9.
12. Flournoy DJ. Incidence of bacteria from clean-catch and catheterized urine of nursing home residents. J Okla State Med Assoc 1993;86:550-2.
13. Slocum RH, Cummings JG. Amino acid analysis of physiological samples. In: Hommes FA, editor. Techniques in diagnostic human biochemical genetics. New York: Wiley-Liss; 1990. p 87-126.
14. NCCLS. The reference system for the clinical laboratory: criteria for development and credentialing of methods and materials for harmonization of results; proposed guideline. NCCLS document NRSCL13-P. Wayne: NCCLS, 1995.
Clin Lab Sci 2004;17(3):149
Jeannie L Nillen is in the Human Adaptation and Countermeasures Office, Wyle Laboratories.
Scott M Smith PhD is in the Human Adaptation and Countermeasures Office, NASA Johnson Space Center.
Address for correspondence: Scott M Smith PhD, Nutritional Biochemistry Laboratory, Human Adaptation and Countermeasures Office, Mail Code SK3, NASA Johnson Space Center, Houston TX 77058. (281) 483-7204, (281) 483-2888 (fax). scott.m.smith@nasa.gov
Copyright American Society for Clinical Laboratory Science Summer 2004
Provided by ProQuest Information and Learning Company. All rights Reserved