SKIN AND WOUND CARE
Incontinent patients present unique challenges to successful skin care management.
Abstract: Improve your understanding of the factors that contribute to perineal skin breakdown in incontinent patients and how to prevent or manage this condition. (Nurs Manage 2002:33(12):61-63]
Patients with urinary or fecal incontinence risk sustaining perineal skin damage, which, in turn, increases their susceptibility to urinary tract infection, pressure ulceration, and secondary den-nal infection.
Risk factors
Four risk factors contribute to skin breakdown related to incontinence:
* Moisture. Excessive moisture in an incontinent patient comes from several sources, including urine, perspiration, or liquid stool.1 The frequency and volume of the incontinence and the use of a containment device, such as a pad or brief, that traps moisture next to the perineal skin and promotes perspiration can affect the risk for skin damage.
* Skin pH. Normal skin maintains a slightly acidic pH; perineal skin exposed to urinary or fecal incontinence tends to be alkaline. Multiple factors contribute to this alkalinity Urine contains urea and ammonia that increase pH. Overgrowth of normal bacteria due to perspiration or urinary or fecal incontinence also leads to the production of more urea.
* Colonization with microorganisms. Prolonged exposure of the perineal skin to urine, stool, or perspiration leads to overgrowth of bacteria and local infection, particularly when combined with use of an incontinence brief, pad, or other containment device. Cutaneous infections irritate and inflame the skin, further reducing its efficiency as a barrier.
* Friction. When overhydrated skin interacts with incontinence containment devices, clothing, or the surface of a bed or chair, the friction produced may cause erosion of the stratum corneum of the skin's epidermis. In most cases, this erosion remains superficial, but it may involve large areas of perineal skin.
Skin care specifics
The goals of perineal skin care in an incontinent patient include:
* removing soil and irritants from the skin regularly
* preventing or minimizing additional exposure to damaging irritants and bacteria
* establishing a local environment conducive to healing.
Preventive perineal skin care essentially involves routine hygiene and judicious use of topical barrier products. Routine hygiene consists of cleansing when the skin becomes exposed to irritants interspersed with regular cleansing of the entire perineum. Traditionally thought of as the gold standard for skin hygiene, soap and water applied with a washcloth isn't the best procedure for preventing or managing problems in the incontinent patient 2 Although soap and water applied with a washcloth will cleanse the skin, regular use also tends to dry the skin and raise its pH. In addition, if applied with excessive fervor, soap and water can contribute to the erosion of the epidermis, which exacerbates, rather than alleviates, the risk of irritant dermatitis or secondary dermal infection.
Because of these risks, the cleanser selected should remove soil from the surface of the perineal skin and promote the integument's potential to heal and resist further damage. Base this selection on a careful evaluation of the patient's needs and the cleanser's ingredients rather than marketing claims or routine selection of products by the materials management department.3,4
Three broad categories of products used to manage perineal skin exist: cleansers, moisturizers, and moisture barriers.
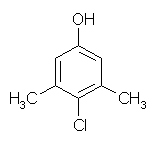
* Cleansers. Perineal skin cleansers typically contain water and a surfactant designed to remove irritants and related materials from the surface of the skin. Common surfactants found in skin cleansers include various lauryl sulfates (LS) such as sodium LS, triethanolamine LS, or sodium stearate. Skin cleansers may also contain antibacterial agents such as triclosan, para chloroxylenol, or chlorhexidine gluconate designed to limit bacterial growth and reduce odor.
In addition, consider the pH of the skin cleanser. The normal pH of the skin is 55. It's important to select a product that has a pH near this value because an alkaline environment irritates the skin and promotes bacterial overgrowth.
Cleansers may come packaged as a liquid, emulsion, or foam, or in a soft towelette, impregnated with the active ingredients.
* Moisturizers. Moisturizers contain humectants, such as glycerin, methyl glucose esters, lanolin, or mineral oil that replace oils in the skin and promote its effectiveness as a moisture barrier. Although overhydrated from exposure to urine or stool, perineal skin in an incontinent patient may paradoxically seem dry because of a deficiency of the oils seen in normal skin.
Some moisturizers get applied as a separate step in perineal skin care, but many are combined with perineal skin cleansers, saving the time and expense of applying a separate product. Skin cleansing products also may incorporate cetyl or stearyl alcohol in proper concentrations as emollients to soften the skin and soothe irritation.
* Moisture barriers. Moisture barriers, sometimes called skin protectants, shield the skin from exposure to irritants or moisture. Active ingredients in moisture barriers include petrolatum, dimethicone, lanolin, or zinc oxide. A moisture barrier may be incorporated into skin cleansers or applied separately as a cream or ointment. Creams are water-based preparations, whereas ointments are oilbased preparations and have a longerlasting effect than creams because of their more occlusive nature. Typically, manufacturers use petrolatum as the oil component of ointments; creams tend to contain lanolin.
Choosing Coro Plans
Although an assessment of the perineal skin and response to specific products should govern the skin care plan for an incontinent patient, also consider the following general guidelines:
Intact skin and mild to severe urinary incontinence. Cleanse the entire perineum daily, whenever a moist urinary containment device gets changed, or following an episode of significant urinary leakage. Apply a moisturizer cream or ointment if the perineal skin becomes chapped or dry after cleansing.
* Fecal incontinence. Cleanse the perineum daily and with each major incontinent episode. Routinely apply a moisture barrier cream or ointment. Avoid liquid barriers because of the potential for irritation, particularly when exposed to liquid stool.
* Double urinary and fecal incontinence. Cleanse the perineum daily and with each major incontinent episode. Routinely apply a moisture barrier cream or ointment. If the drainage contains irritants, a paste may help to protect the skin.
* Perineal skin infection. Initiate localized or systemic treatment for infected perineal skin. Treat candidiasis with an ointment or cream that also prevents exposure to moisture. Use systemic antibiotics to treat secondary bacterial infections.5
Maximize healing
Keep in mind that caring for the incontinent patient with perineal skin problems begins with a thorough assessment. This assessment allows you to identify existing perineal skin problems and create a care plan that minimizes exposure to irritants and maximizes healing.
References
1. Fiers, S., and Thayer, D.: "Management of Intractable Incontinence," in Doughty, D. (Ed): Urinary and Fecal Incontinence: Nursing Management, 2nd ed. Mosby, St. Louis, Mo., 2000.
2. Byers, P., Ryan, P., Regan, M., Shields, A., and Carta, S.: "Effects of Incontinence Care Cleansing Regimens on Skin Integrity,' Journal of Wound, Ostomy, and Continence Nursing. 22(4): 187-92, 1996.
3. Fiers, S., and Thayer, D.: loc cit.
4. Nix, D.: "Factors to Consider When Selecting Skin Cleansing Products,' Journal of Wound, Ostomy, and Continence Nursing. 27(5): 260-8, 2000.
5. Fiers, S., and Thayer, D.: loc cit.
Adapted from "Tender Mercies: Providing Skin Care for an Incontinent Patient," Nursing2002. 32(7): 51-54, 2002.
By Mike) Gray, CUNP, CCCN, FAAN, PhD; Catherine Ratliff, RN, CWOCN, PhD; and Ann Donovan, RN, MSN, CWOCN
About the authors
Mel Gray is a Professor and Nurse Practitioner, Department of Urology and School of Nursing, Catherine Ratliff is an Assistant Professor and Clinician Five, Department of Nursing and Department of Plastic and Reconstructive Surgery, and An Dwu is a WOC Nurse Specialist, Department of Nursing, University of Virginia, Charlottesville, Va.
Copyright Springhouse Corporation Dec 2002
Provided by ProQuest Information and Learning Company. All rights Reserved