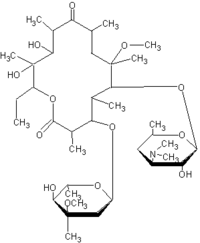
Clarithromycin
Clarithromycin is a macrolide antibiotic used to treat pharyngitis, tonsillitis, acute maxillary sinusitis, acute bacterial exacerbation of chronic bronchitis, pneumonia (especially atypical pneumonias associated with Chlamydia pneumoniae or TWAR), skin and skin structure infections, and, in HIV and AIDS patients to prevent, and to treat, disseminated Mycobacterium avium complex or MAC. more...
In addition, it is sometimes used to treat Legionellosis.
Clarithromycin is available under several brandnames, for example Biaxin and Klacid.
History
Abbott Laboratories brought out clarithromycin in 1991.
Available forms
Clarithromycin is commonly administered in tablets (Biaxin®), extended-release tablets (Biaxin XL®), or oral suspension.
Mechanism of action
Clarithromycin prevents bacteria from growing, by interfering with their protein synthesis. Clarithromycin binds to the subunit 50S of the bacterial ribosome, and thus inhibits the translocation of peptides. Clarithromycin has similar antimicrobial spectrum as erythromycin, but is more effective against certain gram-negative bacteria, particularly Legionella pneumophilae. Besides this bacteriostatic effect, clarithromycin also has bactericidal effect on certain strains such as Haemophilus influenzae, Streptococcus pneumoniae and Neisseria gonorrhoeae.
Pharmacokinetics
Unlike erythromycin, clarithromycin is acid-stable and can therefore be taken orally without being protected from gastric acids. It is readily absorbed, and diffused into most tissues and phagocytes. Due to the high concentration in phagocytes, clarithromycin is actively transported to the site of infection. During active phagocytosis, large concentrations of clarithromycin is released. The concentration of clarithromycin in the tissues can be over 10 times higher than in plasma. Highest concentrations were found in liver and lung tissue.
Metabolism
Clarithromycin has a fairly rapid first-pass hepatic metabolism, i.e it is metabolised by the liver. However, this metabolite, 14-hydroxy clarithromycin is almost twice as active as clarithromycin. The half-life of clarithromycin is about 5 hours and 14-hydroxy clarithromycin's about 7 hours. Clarithromycin's and its metabolites' main routes of elimination are urinary and biliary excretion.
Side effects
Most common side-effects are gastrointestinal; diarrhea, nausea, abdominal pain and vomiting. Less common side-effects include headaches, rashes, alteration in senses of smell and taste.
Special Precautions
Allergic reactions can occur with clarithromycin use. People with a history of allergy, asthma, hay fever or hives seem to be more susceptible to these reactions. The reaction can be immediate and severe.
Allergic symptoms include wheezing, hives, itching, swelling, spasms in the throat and breathing tubes, joint and muscle pain, difficulty breathing, fever and skin rashes. Nausea and vomiting are not symptoms of an allergic reaction.
Read more at Wikipedia.org