We examined how a common therapy that includes clarithromycin affects normally colonizing Staphylococcus epidermidis. Samples from the nostrils of 5 patients receiving therapy were collected before, immediately after, 1 year after, and 4 years after treatment. From each patient and sample, S. epidermidis strains were isolated and analyzed for clarithromycin susceptibility and presence of the erm(C) gene. We show that macrolide-resistant strains of S. epidermidis were selected during therapy and that the same resistant strain may persist for 4 years, in the absence of further antimicrobial treatment.
**********
The emergence and spread of drug-resistant bacteria pose a serious threat to global public health (1,2), and the normal biota constitutes a potential reservoir of resistance genes that can spread to invading pathogens (3,4). A gene (aphA-3) that confers resistance to amikacin and kanamycin in Campylobacter spp. may have originated from the gram-positive Enterococcus, Streptococcus, or Staphylococcus spp. (4). Similarly, aadE and tet(O), which encode streptomycin and tetracycline resistance, respectively, have been found in Campylobacter spp. but are considered to have been transferred from gram-positive bacteria (4). Moreover, parts of the mosaic penicillin-binding protein genes of Streptococcus pneumoniae that confer penicillin resistance are likely to originate from viridans streptococci, which tend to be more resistant (5), and the mecA gene that renders Staphylococcus aureus resistant to all [beta]-lactams likely originated in coagulase-negative staphylococci (6).
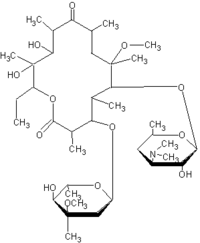
Staphylococcus epidermidis, a coagulase-negative staphylococcus, is a major component of the normal human biota (7). Large populations ([10.sup.3]-[10.sup.6] CFU/[cm.sup.2]) of S. epidermidis are commonly found in the anterior nares and the axillae (7). Coagulase-negative staphylococci have been increasingly recognized as important nosocomial pathogens (8), affecting immunocompromised patients or those with indwelling devices, such as joint prostheses, prosthetic heart valves, and central venous catheters (8,9). Since the infections associated with S. epidermidis are chiefly acquired during hospitalization, it is not surprising that they are increasingly resistant to antimicrobial drugs (10). Macrolide resistance in S. epidermidis is commonly caused by erm genes (10), whose products dimethylate a 23S rRNA adenine residue, preventing macrolide binding to the 50S ribosomal subunit (11,12). In S. epidermidis, erm(C), which induces high-level macrolide resistance, predominates (13,14).
In this study, we have assessed how a commonly used therapy that includes clarithromycin affects the normal microbiota of S. epidermidis. We show that a 1-week course of clarithromycin selects for macrolide-resistant S. epidermidis that may persist up to 4 years after treatment.
Methods
During a cohort study that examined eradication of Helicobacter pylori by a combination therapy that included clarithromycin, we chose 5 patients in order to study macrolide resistance in S. epidermidis. In the larger study, all patients were colonized with H. pylori and had either a duodenal or gastric ulcer, for which a 7-day course of clarithromycin 250 mg twice per day (b.i.d.), metronidazole 400 mg b.i.d., and omeprazole 20 mg b.i.d, was given. We excluded patients who had previously been treated for H. pylori or who had received any antimicrobial treatment within the prior 4 weeks. The control group included 5 patients with dyspeptic symptoms who had not received any antimicrobial treatment. During the 4-year course of this study, no other antimicrobial treatment was allowed. The study was approved by the human ethics committee at Uppsala University, Uppsala, Sweden.
Samples from the nares of each patient were collected 1 day before treatment, 3-7 days immediately after, 1 year later, and 4 years later. All samples were stored at -70[degrees]C until analyzed. From each study patient and each sample, 10 independent colonies of S. epidermidis were isolated on Columbia blood agar plates (Difco, Baltimore, MD, USA) and verified by Gram staining, positive catalase, negative DNase, negative mannitol, and negative trehalose testing. DNA was extracted from the bacterial strains with the DNeasy Tissue kit (Qiagen, Hilden, Germany). MIC of clarithromycin was measured with the Etest (AB Biodisk, Solna, Sweden), as recommended by the Swedish Reference Group for Antibiotics.
The erm(C) gene was detected as described (13), by using primers ermC1/C2 5'-GCTAATATTGTTTAAATCGTCAATTCC-3' and 5'-GGATCAGGAAAAGGACATTT-3' but with the following modifications: each polymerase chain reaction (PCR) contained 25 gL master mix (PeR Master, Roche, Penzberg, Germany), 30 pmol of each primer, 14 [micro]L distilled water, and 5 [micro]L DNA sample. The amplified 572-bp product was separated by electrophoresis on a 1.5% agarose gel.
For pulsed-field gel electrophoresis (PFGE), bacterial cells were harvested by centrifugation from 3 mL overnight cultures in brain-heart infusion broth and resuspended in 3 mL Tris-HCl buffer (pH 7.6). The bacterial suspension (150 [micro]L) was mixed with 150 [micro]L 2% agarose (Sigma, St. Louis, MO, USA) in Tris-HCl buffer and used for making the gel plugs. The plugs were incubated at 35[degrees]C overnight in 4 mL Lysis 1 buffer (6 mmol/L Tris-HCl [pH 7.6], 1 mol/L NaCl, 100 mmol/L EDTA [pH 7.5], 0.5% Brij 58, 0.2% deoxycholate, 0.5% sodium lauryl sarcosine [Sarcosyl, Kodak International Biotechno-logies, New Haven, CT, USA], 1 mg/mL lysozyme [Life Technology, Sigma-Aldrich, Steinheim, Germany], and 7 [micro]g/mL lysostaphin [Sigma]), then incubated overnight at 55[degrees]C in 4 mL Lysis 2 buffer (1% sodium lauryl sarcosine [Sarcosyl], 0.5 mol/L EDTA [pH 9.5], and 50 [micro]g/mL Proteinase K [Roche Diagnostics Corporation, Indianapolis, IN, USA]). The plugs were washed 3 times for [greater than or equal to] 30 min at 35[degrees]C in 4 mL of Tris-EDTA buffer. A 3-mm slice of each gel plug was incubated overnight at 25[degrees]C with SmaI (Life Technology, Invitrogen, Carlsbad, CA, USA) and buffer, then placed in the wells of a 1.0% agarose gel (Ultra pure agarose, Life Technology, Invitrogen), sealed with 1.0 % agarose, and put in 0.5x Tris-borate-EDTA buffer. Electrophoresis (Gene Path Electrophoresis System, Bio-Rad Laboratories, Inc., Hercules, CA, USA) was performed with the following conditions: 5-60 s switch interval with a voltage gradient of 6 V/h at an angle of 120[degrees] for 23 h. After electrophoresis, the gel was stained with ethidium bromide for 30 min, destained in distilled water for 1 h, and DNA was visualized under UV light (Gel doc 1000, Bio-Rad Laboratories, Inc.). The restriction fragment profiles were interpreted by comparison with each other, with a reference S. aureus strain NCTC 8325, and with a [lambda] phage DNA standard (New England Biolabs, Beverly, MA, USA).
Results
At 1 day before treatment, all 5 patients in the treatment group harbored clarithromycin-susceptible (MIC <0.5 [micro]g/mL) S. epidermidis among the 10 independent colonies examined. In 4 patients, all 10 isolates were susceptible, but in the fifth patient 2 isolates were highly resistant (MIC >256 [micro]g/mL) because erm(C) was present. Immediately after completing treatment, 4 of 5 patients displayed high-level clarithromycin-resistant (MIC >256 gg/mL) isolates (Table 1). The other isolates from this time point were either resistant with lower MIC values (16-96 [micro]g/mL) or susceptible. Highly resistant isolates could be detected 1 year after treatment in 4 patients and 4 years after treatment in 3 patients. All highly resistant isolates harbored erm(C), as determined by PCR. In the controls, who did not receive any antimicrobial treatment, no selection of resistant staphylococci was detected. However, in control 4, 1 highly resistant isolate was detected at the first time point. In the same control, 2 of 10 isolates were highly resistant at the second time point, but no resistance was detected at the 1- and 4-year follow-ups. In control patient 5, all isolates were susceptible, except 5 resistant isolates detected at the 4-year follow up (Table 2).
Isolates obtained from patients 1 and 2, chosen to investigate the clonality of resistance, were genotyped by pulsed-field gel electrophoresis (PFGE). Before treatment, each patient carried 5 different S. epidermidis strains among the 10 colonies tested. In patient 1, no highly resistant isolates were detected before treatment. However, immediately after treatment, 2 of 10 isolates were highly resistant, both defined as strain H. Based on PFGE patterns, strain H was detected in 8 of 10 isolates 1 year after treatment and in 4 of 10 isolates 4 years after treatment (Table 1). Strain G, which was susceptible to clarithromycin, was present immediately after treatment and 4 years later. Two of the pretreatment strains (B and C) were detected 4 years after treatment.
For patient 2, from whom 2 highly resistant isolates with the same profile (N) were detected before treatment, PFGE showed 2 distinct resistant strains (N and S) to be present immediately after treatment. Clone N was detected in 8 of 10 isolates 1 year after treatment and in 3 of 10 isolates 4 years after treatment. Susceptible strains P and Q, which were present pretreatment, were isolated again 4 years after treatment. Thus, after treatment in both cases, PFGE analysis showed that highly resistant strains persisted for 4 years, in the absence of further selection pressure, and that both resistant and susceptible strains were present 4 years after treatment (Table 1).
In a similar manner, the isolates from 2 controls were genotyped (Table 2). In control 1, at least 5 different strains were present at the start of the study. After 1 year, the composition had changed, and after 4 years, a new strain predominated in the flora. In control 2, we initially detected 3 different strains. These strains were also represented at each time point and predominated at 4 years. Thus, 1 control showed stable populations, whereas the other showed a dynamic state in the absence of treatment.
Discusien
Since antimicrobial drugs do not distinguish between pathogenic and colonizing bacteria, our indigenous biota is affected every time a drug is given (3,15). Resistance development in staphylococci that normally colonize the skin has previously been observed after antimicrobial prophylaxis or treatment (16-18). Depending on mechanism, resistance can be selected de novo, exist in the pretreatment biota, or be acquired, especially in hospital environments.
In this study of the effect of a 1-week course of clarithromycin on indigenous S. epidermidis populations, we show that macrolide-resistant S. epidermidis strains are selected during therapy and that, without further selection, resistant clones can persist for up to 4 years. This finding is important for several reasons. First, although S. epidermidis belongs to the normal cutaneous microbiota, it may be a pathogen, especially in hospitalized patients (8); stably resistant populations increase the risk for treatment failure. Second, resistance in the normal microbiota might contribute to increased resistance in higher-grade pathogens by interspecies genetic transfer. Since the population size of the normal microbiota is large, multiple and different resistant variants can develop, which increases the risk for spread to populations of pathogens. Persisting populations of resistant microbiota further enhance transfer risk, especially if the selecting agent is used for treatment. Third, antimicrobial drugs may affect the stability of residential populations.
Whether a resistant population persists is mostly determined by the fitness and transmission costs of resistance (19,20). Most resistance involves a cost (21-24), but resistance may occur without detectable cost (25). If most resistance is costly for bacteria, resistant populations should decline once the selective antimicrobial pressure is removed. However, mutations may arise that compensate for the fitness cost, restoring the bacteria's fitness without reversion of the resistant phenotype. This phenomenon, compensatory evolution, is considered to be relevant to stabilizing resistant populations (26). Other important mechanisms that could stabilize resistant populations are no-cost resistance mutations (25) and genetic linkage with adjacent genes. Despite substantially decreased sulfonamide use in the United Kingdom from 1991 to 1999,
Escherichia coli resistance to sulfonamides remained high (39.7% in 1991, 46.0% in 1999) because sulfonamide resistance was linked to other resistance genes that continued to be under selective pressure (27). In poultry, since vanA can be co-selected with erm(B) in Enterococcus hirae isolates (28), vancomycin resistance can be maintained by using macrolides, despite excluding avoparcin from animal feed. Thus, the stability and maintenance of antimicrobial drug resistance depends on the magnitude of selective pressure, compensatory evolution, no-cost associated resistance, and genetic linkage with co-selected resistance genes.
In our study, resistant isolates persisted long after drug treatment was completed. However, a variation in length of persistence between the patients was observed. Whether this variation is related to different costs associated with erm(C) carriage or different extents of genetic compensation for an initial cost cannot be concluded from current data. The observed variation in persistence of resistance could further be affected by the degree of recolonization and transient colonization of new strains during the 4-year study period. Although recolonization with S. epidermidis is presumably low, it can be enhanced by, for example, nosocomial spread during hospital stays (29). That indigenous S. epidermidis populations may naturally change in composition over time was reflected in the control group. According to the PFGE profiles from controls 1 and 2, populations of S. epidermidis can either remain stable for 4 years or show a more dynamic state, with new strains appearing over time. A change in the composition of the flora was also observed in control 5, in whom 5 resistant isolates appeared in the susceptible flora after 4 years. Since this patient did not receive any antimicrobial drugs during the study period, this finding is likely due to recolonization or transient colonization of a strain from the environment. However, most importantly, although a few resistant isolates were detected among the controls, no selection of resistant S. epidermidis occurred over the 4year study period, as was observed in the treated patients.
In conclusion, antimicrobial drug treatment affects our indigenous microbiota and can give rise to long-term colonization with resistant populations. Our results show that as part of a combination therapy, a 7-day course of clarithromycin resulted in macrolide-resistant S. epidermidis that persisted up to 4 years without any further selection. In total, these observations suggest that selection of resistance in our microbiota after short antimicrobial drug courses may not be a rare phenomenon. However, the extent, to which other antimicrobial treatment regimens select for resistant S. epidermidis remains to be investigated.
This work was supported in part by the AFA Health Research Foundation, Stockholm, Sweden; the Swedish Research Council; the Capio Research Fund, Stockholm, Sweden; the Scandinavian Society of Antimicrobial Chemotherapy, Sweden; RO1GM63270 by the National Institute of Health, USA; and the Filomena D'Agostino Foundation.
Dr Sjolund is a microbiologist at the Department of Bacteriology, Swedish Institute for Infectious Disease Control, Stockholm, Sweden. Her research interests include the characterization of drug-resistant bacteria, mechanisms of resistance, and studies of the biological cost of drug resistance.
References
(1.) Levy SB. The 2000 Garrod lecture. Factors impacting on the problem of antibiotic resistance. J Antimicrob Chemother. 2002;49:25-30.
(2.) Finch RG. Antibiotic resistance. J Antimicrob Chemother. 1998;42:125-8.
(3.) Sullivan A, Edlund C, Nord CE. Effect of antimicrobial agents on the ecological balance of human microflora. Lancet Infect Dis. 2001;1:101-14.
(4.) Courvalin P. Transfer of antibiotic resistance genes between gram-positive and gram-negative bacteria. Antimicrob Agents Chemother. 1994;38:1447-51.
(5.) Dowson CG, Coffey TJ, Kell C, Whiley RA. Evolution of penicillin resistance in Streptococcus pneumoniae; the role of Streptococcus mitis in the formation of a low affinity PBP2B in S. pneumoniae. Mol Microbiol. 1993;9:635-43.
(6.) Wu SW, de Lencastre H, Tomasz A. Recruitment of the mecA gene homologue of Staphylococcus sciuri into a resistance determinant and expression of the resistant phenotype in Staphylococcus aureus. J Bacteriol. 2001;183:2417-24.
(7.) Kloos WE, Bannerman TL. Update on clinical significance of coagulase-negative staphylococci. Clin Microbiol Rev. 1994;7:117-40.
(8.) von Eiff C, Peters G, Heilmann C. Pathogenesis of infections due to coagulase-negative staphylococci. Lancet Infect Dis. 2002;2:677-85.
(9.) O'Gara JP, Humphreys H. Staphylococcus epidermidis biofilms: importance and implications. J Med Microbiol. 2001;50:582-7.
(10.) Archer GL, Climo MW. Antimicrobial susceptibility of coagulase-negative staphylococci. Antimicrob Agents Chemother. 1994;38:2231-7.
(11.) Weisblum B. Erythromycin resistance by ribosome modification. Antimicrob Agents Chemother. 1995;39:577-85.
(12.) Pechere JC. Macrolide resistance mechanisms in gram-positive cocci. Int J Antimicrob Agents. 2001;18(Suppl 1):S25-8.
(13.) Lina G, Quaglia A, Reverdy ME, Leclercq R, Vandenesch F, Etienne J. Distribution of genes encoding resistance to macrolides, lincosamides, and streptogramins among staphylococci. Antimicrob Agents Chemother. 1999;43:1062-6.
(14.) Lim JA, Kwon AR, Kim SK, Chong Y, Lee K, Choi EC. Prevalence of resistance to macrolide, lincosamide and streptogramin antibiotics in gram-positive cocci isolated in a Korean hospital. J Antimicrob Chemother. 2002;49:489-95.
(15.) Sjolund M, Wreiber K, Andersson DI, Blaser MJ, Engstrand L. Long-term persistence of resistant Enterococcus species after antibiotics to eradicate Helicobacter pylori. Ann Intern Med. 2003;139:483-7.
(16.) Terpstra S, Noordhoek GT, Voesten HG, Hendriks B, Degener JE. Rapid emergence of resistant coagulase-negative staphylococci on the skin after antibiotic prophylaxis. J Hosp Infect. 1999;43:195-202.
(17.) Kotilainen P, Nikoskelainen J, Huovinen P. Emergence of ciprofloxacin-resistant coagulase-negative staphylococcal skin flora in immunocompromised patients receiving ciprofloxacin. J Infect Dis. 1990;161:41-4.
(18.) Archer GL. Alteration of cutaneous staphylococcal flora as a consequence of antimicrobial prophylaxis. Rev Infect Dis. 1991;13(Suppl 10):S805-9.
(19.) Andersson DI, Levin BR. The biological cost of antibiotic resistance. Curr Opin Microbiol. 1999;2:489-93.
(20.) Bjorkman J, Andersson DI. The cost of antibiotic resistance from a bacterial perspective. Drug Resist Updat. 2000;3:237-45.
(21.) Schrag SJ, Perrot V, Levin BR. Adaptation to the fitness costs of antibiotic resistance in Escherichia coli. Proc Biol Sci. 1997;264:1287-91.
(22.) Reynolds MG. Compensatory evolution in rifampin-resistant Escherichia coli. Genetics. 2000;156:1471-81.
(23.) Bjorkman J, Samuelsson P, Andersson DI, Hughes D. Novel ribosomal mutations affecting translational accuracy, antibiotic resistance and virulence of Salmonella typhimurium. Mol Microbiol. 1999;31:53-8.
(24.) Bjorkholm B, Sjolund M, Falk PG, Berg OG, Engstrand L, Andersson DI. Mutation frequency and biological cost of antibiotic resistance in Helicobacter pylori. Proc Natl Acad Sci U S A. 2001;98:14607-12.
(25.) Sander P, Springer B, Prammananan T, Sturmfels A, Kappler M, Pletschette M, et al. Fitness cost of chromosomal drug resistance-conferring mutations. Antimicrob Agents Chemother. 2002;46: 1204-11.
(26.) Levin BR, Perrot V, Walker N. Compensatory mutations, antibiotic resistance and the population genetics of adaptive evolution in bacteria. Genetics. 2000;154:985-97.
(27.) Enne VI, Livermore DM, Stephens P, Hall LM. Persistence of sulphonamide resistance in Escherichia coli in the UK despite national prescribing restriction. Lancet. 2001;357:1325-8.
(28.) Borgen K, Sorum M, Wasteson Y, Kruse H, Oppegaard H. Genetic linkage between erm(B) and vanA in Enterococcus hirae of poultry origin. Microb Drug Resist. 2002;8:363-8.
(29.) Kotilainen P, Huovinen S, Jarvinen H, Aro H, Huovinen P. Epidemiology of the colonization of inpatients and outpatients with ciprofloxacin-resistant coagulase-negative staphylococci. Clin Infect Dis. 1995;21:685-7.
Maria Sjolund, * ([dagger]) Eva Tano, * Martin J. Blaser, ([double dagger]) Dan I. Andersson, ([dagger]) and Lars Engstrand * [dagger]
* University Hospital, Uppsala, Sweden; ([dagger]) The Swedish Institute for Infectious Disease Control, Solna, Sweden; and ([double dagger]) New York University School of Medicine, New York, New York, USA
Address for correspondence: Lars Engstrand, Department of Bacteriology, Swedish Institute for Infectious Disease Control, SE-171 82 Solna, Sweden; fax: 46-8-301-797; email: lars.engstrand@smi.ki.se
COPYRIGHT 2005 U.S. National Center for Infectious Diseases
COPYRIGHT 2005 Gale Group