Background: As the number of elderly people has increased in Japan, the occurrence of aspiration pneumonia has also increased. Guidelines for the treatment of pneumonia have been proposed, in which the use of antibiotics, such as [beta]-lactam plus [beta]-lactamase inhibitor, clindamycin, and carhapenem, has been recommended as effective against anaerobic bacteria in the treatment of aspiration pneumonia. However, to our knowledge, a prospective comparison of these antibiotics regarding their clinical efficacy in aspiration pneumonia has not been performed. Study objectives: We compared the effects of IV administration of a half dose of ampicillin/ sulbactam (SBT/ABPC), normal dose of SBT/ABPC, IV clindamycin, and IV panipenem/betamiprom (PAPM/BP) for treatment of mild-to-moderate aspiration pneumonia in elderly patients.
Design: Randomized prospective study.
Patients: One hundred adult patients with compatible signs and symptoms of aspiration pneumonia.
Assessments: Patients were assessed before, during, and after treatment regarding symptoms, as well as results of laboratory values, chest radiograph examinations, and sputum bacterial cultures.
Results: We found few differences between the groups regarding cure rate, duration of IV medication, and occurrence of adverse effects with the tested therapies. However, clindamycin therapy was less expensive and was associated with a lower rate of post-treatment occurrence of methicillin-resistant Staphylococcus aureus.
Conclusions: Clindamycin therapy for mild-to-moderate aspiration pneumonia is clinically effective, and provides economic advantages as compared to SBT/ABPC or PAPM/BP therapy.
Key words: ampicillin/sulbactam; aspiration pneumonia; clindamycin: medical cost; methicillin-resistant Staphylococcus aureus; panipenem/betamiprom; prospective clinical study
Abbreviations: CRP = C-reactive protein; IDSA = Infectious Diseases Society of America; MRSA = methicillin-resistant Staphylococcus aureus; PAPM/BP = panipenem/betamiprom; PBP = penicillin-binding protein; PORT = Patient Outcome Research Team; SBT/ABPC = ampicillin/sulbactam
**********
In Japan, pneumonia is the fourth-leading cause of death in elderly people. As the number of elderly people has increased, the occurrence of aspiration pneumonia has also been increasing. Kikuchi et al (1) reported that silent aspiration in the elderly with an acute episode of pneumonia occurred more frequently (70%) than in control subjects (10%).
Bartlett et al (2) prospectively studied 54 cases of pulmonary infection following aspiration and concluded that anaerobes that normally colonize the oral cavity play a key role in most cases of aspiration pneumonia. Furthermore, it is not uncommon for anaerobic bacteria to be resistant to a number of [beta]-lactam antibiotics because of the production of [beta]-lactamase. (3) Therefore, it has been recommended that antibiotics such as a [beta]-lactam plus [beta]-lactamase inhibitor, clindamycin, and carbapenem should be used, each of which are effective against anaerobic bacteria. (4-6) However, to our knowledge, the efficacy, bacteriologic effects, and adverse effects of these antibiotics have not been compared prospectively. We studied patients who received an administration of a [beta]-lactam plus [beta]-lactamase inhibitor (ampicillin/sulbactam [SBT/ABPC]), clindamycin, or carbapenem (panipenem/betamiprom [PAPM/BP]) who had mild-to-moderate aspiration pneumonia.
MATERIALS AND METHODS
Patients
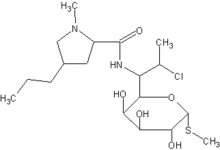
One hundred patients aged 71 to 94 years were studied between July 2000 and October 2003. These patients were hospitalized in Fukui or Ishikawa Prefecture in Japan and had mild or moderate aspiration pneumonia. The majority of the enrolled patients were nursing home residents. The diagnosis of aspiration pneumonia was made based on symptoms of fever, cough, and purulent sputum, as well as observed aspiration and a predisposition to aspirate due to dysphagia, and the results of blood analyses and radiographic examinations, such as chest radiograph and CT imaging, which revealed characteristic images compatible with aspiration pneumonia in the posterior segments of the lower lobes. (6-7) Clinical signs suggesting the presence of dysphagia were delayed swallowing, coughing or choking before, during, and after swallowing, and decreased oral/pharyngeal sensation. (8) Chemical aspiration pneumonitis that occurred after apparent vomiting was excluded. (7) The severity was graded by criteria for pneumonia established by the Japan Society of Chemotherapy, (9) which included body temperature, chest radiograph score (Table 1, Fig 1), WBC count, and C-reactive protein (CRP) [Table 2]. (9) Applying to the classification of community-acquired pneumonia by the American Thoracic Society (10) or that by the Infectious Disease Society of America (IDSA), (6) our patients were designated to group 3 and class IV, respectively.
[FIGURE 1 OMITTED]
Exclusion Criteria
Patients with severe pneumonia, severe complications, and known allergies to the tested antibiotics, as well as those who had received other antibiotic therapy within 1 month prior to enrollment, were excluded. Informed consent was obtained from all patients prior to their participation.
Study Design
Following enrollment, the patients were randomly assigned to one of four IV treatment regimens. After beginning the study, two younger and three older patients were excluded because of age limitation, while one patient was admitted for a different disease (colon cancer). Patients in group 1 received a half dose of SBT/ABPC (1.5 g bid), those in group 2 received a normal dose of SBT/ABPC (3 g bid), those in group 3 received clindamycin (600 mg bid), and those in group 4 received PAPM/BP (0.5 g bid). Randomization was achieved by sealed envelopes, and the balance among groups was achieved by block randomization. When the number of patients reached 25 in each treated group, we preliminarily analyzed the results. Since we found methicillin-resistant Staphylococcus aureus (MRSA) in three of the treatment groups but not in the clindamycin group, we decided to discontinue the study early.
Assessments
We assessed the results by focusing on five parameters: healing effect, occurrence of adverse effects, duration of IV medication, new appearance of antibiotic-resistant bacteria, and antibiotic cost. The healing effect was determined by assessing body temperature, chest radiograph score, WBC count, and CRP (Table 3). (9) Those examinations were performed on day 1 (just prior to beginning therapy), day 3, day 7, and in stone cases day 14 of the hospitalization. As soon as the therapy was considered to be ineffective, the physician in charge of the patient changed the antibiotic to one believed more effective. To investigate the biological effects, sputum cultures for bacteria were also examined on days 1, :3, 7, and 14 of hospitalization.
Statistical Analysis
Statistical analysis was performed using software (StatView 5.0; SAS Institute; Cary, NC) on a personal computer. Categorical data were evaluated using [chi square] or Fisher Exact Test. To adjust for multiple comparisons, p values were adjusted using the method of Holm. Variable data were evaluated with one-way analysis of variance using the Fisher protected last-significant difference test. The probability of a type-1 error of 0.05 was used to determine statistical significance. When the p value was > 0.05 and the power analyses data (1-[beta]) were < 0.8, we described the differences in terms of "few differences" instead of "no significant difference."
RESULTS
Patient Characteristics
Table 4 lists the baseline clinical characteristics of the two groups. The details of underlying respiratory diseases were as follows: there were five patients with COPD and one patient with sequelae of pulmonary tuberculosis in the group receiving a half dose of SBT/ABPC, six COPD patients in the group receiving a normal dose of SBT/ABPC, nine COPD patients and one patient with sequelae of pulmonary tuberculosis in the group receiving a half dose of SBT/ABPC, six COPD patients in the clindamycin group, and eight COPD patients in the PAPM/BP group. All of those patients showed compatible images of COPD or changes consistent with previous pulmonary tuberculosis on chest CT images. In these patients, the underlying respiratory diseases were mild.
Clinical Efficacy
There were few differences regarding the clinical efficacy (p = 0.6249, 1-[beta] = 0.158), serial changes of CRP (data not shown), and duration of antibiotic therapy among the four groups (Table 5). The three different antibiotic regimens tested showed rather comparable results, with an efficacy of PAPM/BP of 88%, that of a normal dose of SBT/ABPC of 84%, that of a half dose of SBT/ABPC of 76%, and that of clindamycin of 76% (Table 5). These results were obtained following 8 to 10 days of treatment in each group (p = 0.3550, 1-[beta] = 0.278).
Adverse Events
There were few differences in adverse events between the four groups (p = 0.9717, 1-[beta] = 0.058) [Table 6]. The main side effects noted were digestive problems in group 2, and mild liver dysfunction in groups 1, 3, and 4. None of the patients experienced severe side effects that required any other additional supportive treatment, and each adverse event disappeared as soon as the antibiotic therapy was discontinued.
Economic Analysis
The cost for a single vial or ampule was calculated as follows, with US dollar amounts based on a current exchange rate of 109.83 yen to the dollar: PAPM/BP, 2,021 yen ($18.40) for 0.5 g; SBT/ABPC, 1,385 yen ($12.60) for 1.5 g; and clindamycin, 759 yen ($6.90) for 600 mg (Table 7). Considering the duration of IV medication, the cost was significantly lower in the clindamycin group (13,982 yen, $12.70) as compared to the SBT/ABPC 3 g/d group (22,889 yen, $208.10), SBT/ABPC 6 g/d group (48,805 yen, $443.70), and PAPM/BP group (40,420 yen, $367.50) [p < 0.0001, 1-[beta] = 1.000]. Furthermore, the cost for the SBT/ABPC 3 g/d group was significantly lower than that for the SBT/ABPC 6 g/d and PAPM/BP groups.
Bacteriologic Response
Sputum samples for culture were obtained in 99 of the 100 cases, of which 42 results (42.4%) were negative (Table 8), The detected organisms were Gram-negative bacilli (48.1%), including Klebsiella pneumoniae (24%), Escherichia coli (4.9%), Enterobacter cloacae (4.9%), Pseudomonas aeruginosa (4.9%), and Haemophilus influenzae (3.7%), and Gram-positive cocci (40.7%), including MRSA (12.3%), methicillin-sensitive S aureus (9.8%), and Streptococcus pneumoniae (4.9%). A number of the improved patients showed no disappearance of the detected pathogens following treatment, namely 5 of 18 cases in the half-dose SBT/ABPC group, 5 of 16 cases in the normal-dose SBT/ABPC group, 4 of 17 cases in the clindamycin group, and 4 of 21 cases in the PAPM/BP group.
New Appearance of MRSA
The rate of postantibiotic treatment appearance of MRSA was significantly lower in the clindamycin group (no cases, 0%) as compared with the SBT/ ABPC 3 g/d group (five cases, 22.7%), SBT/ABPC 6 g/d group (five cases, 25%), and PAPM/BP group (eight cases, 34.8%) [p = 0.0228, 1-[beta] = 0.882].
DISCUSSION
In the present study, we obtained three new findings that suggest that clindamycin is advantageous for treating mild-to-moderate aspiration pneumonia in elderly patients. First, clindamycin therapy did not induce the new appearance of MRSA, whereas SBT/ABPC and PAPM/BP therapy induced MRSA at a high rate. Second, the cost of clindamycin therapy was significantly lower than that of the other antibiotic therapies. Finally, clindamycin therapy showed satisfactory clinical efficacy as compared with the other tested [beta]-lactams, and the occurrence of adverse side effects was not as high as that with the other therapies.
Our bacterial examination showed that 57.6% of the detected pathogens were the same kind of bacteria as listed in the report of patients with pneumonia acquired in nursing homes. (11) But, interestingly, 19.0 to 31.3% of the successfully treated patients still had the same pathogen regardless of the treatment. In some reports of nonsevere pneumonia, the microbiological studies were noncontributory. Theerthakarai et al (12) reported that sputum cultures in nonsevere community-acquired pneumonia patients identified pathogens in only 5%. However, as the IDSA guidelines have noted for elderly patients, microbiological studies are valuable for preventing nosocomial infection such as MRS& or when considering changing antibiotics. (6)
MRSA is an increasingly common cause of nosocomial infections, and its prevalence has become a serious problem in clinical medicine. Once MRSA appears, even if it does not affect the patient, greater medical costs are generated, as clinicians are required to observe special precautions to prevent the spread of MRSA. (13) It has been reported that the use of broad-spectrum antibiotics is a critical risk factor for colonization or infection with antibiotic-resistant bacteria. (14) Malin et al (15) recommended the use of drugs with a narrow antimicrobial spectrum or "older" antibiotics to curtail the development of antimicrobial resistance. In our study, the rate of postantibiotic appearance of MRSA was significantly higher in the groups that received SBT/ABPC or PAPM/BP therapy, as compared with those who received clindamycin.
As for why clindamycin therapy did not induce a comparable appearance of MRS& we considered the fact that [beta]-lactams (such as SBT/ABPC, PAPM/ BP) combine with penicillin-binding proteins (PBPs), and then inactivate their transpeptidase and carboxypeptidase activities, which are responsible for catalyzing the final transpeptidation step of bacterial cell wall biosynthesis. (16-17) Although all strains of S aureus have four PBPs (PBP-1 to PBP-4), only MRSA expresses a specific PBP (PBP0-2' or PBP-2a) from the mecA gene. PBP-2' takes over the biosynthetic functions of normal PBPs in the presence of inhibitory concentrations of [beta]-lactams because it has a decreased binding affinity for them. Clindamycin inhibits the formation of 50S subunits in bacterial cells as well as protein synthesis; thus, clindamycin therapy may not induce MRSA. In support of this hypothesis, it has been reported that 39% of cases of community-acquired MRSA were susceptible to clindamycin, (18) as compared to the lack of bactericidal effects shown by the two other tested antibiotics.
The guidelines of the Society for Healthcare Epidemiology of America and IDSA for prevention of the spread of antimicrobial resistance in hospitals recommend appropriate use of antimicrobials, including not only limited use of inappropriate agents, but also appropriate selection, dosing, and duration of antimicrobial therapy to achieve optimal efficacy in managing infections.19 Based on the present results, we recommend clindamycin as an appropriate selection to treat mild-to-moderate aspiration pneumonia in elderly patients.
The cost of clindamycin therapy was found to be very low, which may become more important in the future. Currently, the Japanese society is faced with a serious economic problem of rapidly increasing health-care costs. It is estimated that in 2001, the total medical cost was 3.04 x [10.sup.13] yen, or approximately $3.22 x [10.sup.15], and that 38.5% of the total medical cost, 1.18 x [10.sup.13] yen or approximately $1.25 x [10.sup.15], was spent for patients who were > 70 years old. The drug cost of clindamycin was the lowest, while the duration of treatment was the same as with the other [beta]-lactams tested. In addition, clindamycin therapy did not induce new appearance of MRSA; therefore, the medical cost related to standard precaution for MRSA would also be reduced.
Panipenem is a carbapenem antibiotic that is used extensively in Japan, Korea, and China. Its range of antibacterial activities is broad, including most Gram-negative and Gram-positive aerobic and anaerobic organisms. (20) The antibiotic is administered with an organic anion transport inhibitor, betamiprom, to reduce its renal toxicity, which prevents the uptake of panipenem by the renal cortex. (21) Shibuya et al (22) evaluated the use of PAPM/BP for pneumonia in elderly patients and reported that it was safe and effective.
We also directly compared two different doses of SBT/ABPC. Since the patients were at an advanced age and considered to have lower levels of pharmacometabolism, we anticipated that the half-close SBT/ABPC therapy might induce fewer adverse effects than the normal dose. Although the incidence of adverse effects in these two groups was equal, diarrhea or bloody bowel discharge preferably occurred in those who received the normal dose.
We know that several guidelines for treating patients with mild-to-moderate pneumonia often recommend macrolide oral therapy rather than IV therapy. (23) However, because our medical insurance system could cover the hospital fee, we pursued follow-up care in these patients, attempting to prevent the repeated aspiration pneumonia. Patients were rehabilitated and taught how to swallow food or drink with dietary modification and received aggressive oral care. (8) Thereafter, patients were permitted to have oral intake. Such care in postaspiration pneumonia is usually provided in Japan.
In this study, all the patients improved. According to the Patient Outcome Research Team (PORT) validation cohort, (24) the mortality of patients of class IV who corresponded to our patients' severity was 8.2%. In Japan, Nishimura et al (25) examined the utility of the pneumonia PORT prediction rule for evaluating the severity of community-acquired pneumonia. According to this report, the risk-class-specific mortality rate was 3.2% in class IV.
CONCLUSION
We conclude that for the treatment of mild-to-moderate aspiration pneumonia in elderly patients, clindamycin is preferable as an initial therapy, as we have shown it to be cost-effective and to prevent the emergence of antibiotic-resistant bacteria.
ACKNOWLEDGMENT: The authors thank Professor N. F. Volkel (University of Colorado Health Sciences Center) for his advice and assistance with the preparation of this article.
REFERENCES
(1) Kikuchi R, Watanabe N, Konno T, et al. High incidence of silent aspiration in elderly patients with community-acquired pneumonia. Am J Respir Crit Care Med 1994; 150:251-253
(2) Bartlett JG, Gorbach SL, Finegold SM. The bacteriology of aspiration pneumonia. Am J Med 1974; 56:202-207
(3) Sydney MF. Aspiration pneumonia. Rev Infect Dis 1991; 13(suppl):S737-S742
(4) The Committee of the Japanese Respiratory Society. Guidelines for management of hospital-acquired pneumonia: the basic concept of management for hospital-acquired pneumonia in adults [in Japanese]. Tokyo, Japan: Kyorinsya, 2002; 27-34
(5) American Thoracic Society. Hospital-acquired pneumonia in adults: diagnosis, assessment of severity, initial antimicrobial therapy, and preventative strategies. Am J Respir Crit Care Med 1995; 153:1711-1725
(6) The Infectious Diseases of America. Practice guidelines of the management of community-acquired pneumonia in adults. Clin Infect Dis 2000; 31:347-382
(7) Marik P. Aspiration pneumonitis and aspiration pneumonia. N Engl J Med 2001; 344:665-671
(8) Marik P, Kaplan D. Aspiration pneumonia and dysphagia in the elderly. Chest 2003; 124:328-336
(9) Saito A, Miki F, Oizumi K, et al. Clinical evaluation methods for new antimicrobial agents to treat respiratory infections: report of the Committee for the Respiratory System, Japan Society of Chemotherapy. J Infect Chemother 1999; 5:110-123
(10) American Thoracic Society. Guidelines for the initial management of adults with community-acquired pneumonia: diagnosis, assessment of severity, and initial antimicrobial therapy. Am J Respir Crit Care Med 1993; 148:1418-1426
(11) Janssens J-P, Krause K-H. Pneumonia in the very old. Lancet Infect Dis 2004; 4:112-124
(12) Theerthakarai R, El-Halees W, Ismail M, et al. Nonvalue of the initial microbiological studies in the management of nonsevere community-acquired pneumonia. Chest 2001; 119: 181-184
(13) Garner JS. Guidelines for isolation precautions in hospitals. Infect Control Hosp Epidemiol 1996; 17:53-80
(14) Joseph P, Lynch III. Hospital-acquired pneumonia: risk factors, microbiology, and treatment. Chest 2001; 119:373S-384S
(15) Malin HK, Victoria JF. Antibiotic resistance in the intensive care unit. Ann Intern Med 2001; 134:298-314
(16) de Lencastre H, de Jonge BL, Matthews PR, et al. Molecular aspects of methicillin resistance in Staphylococcus aureus. J Antimicrob Chemother 1994; 33:7-24
(17) Ghuysen JM. 1991. Serine [beta]-lactamases and penicillin binding proteins. Annu Rev Microbiol 1991; 45:37-67
(18) Laurel SA, Virginia DS, Angela MN, et al. Antimicrobial susceptibility and molecular characterization of community-acquired methicillin-resistant Staphylococcus aureus. Diag Microbiol Infect Dis 2002; 43:225-232
(19) David MS, Dale NG, Joseph FJ, et al. Society for Healthcare Epidemiology, of America and Infectious Diseases Society of America Joint Committee on the Prevention of Antimicrobial Resistance: guidelines for the prevention of antimicrobial resistance in hospitals. Clin Infect Dis 1997; 25:584-599
(20) Shimada J, Kawahara Y. Overview of a new carbapenem, panipenem/betamipron. Drugs Exp Clin Res 1994; 20:241-245
(21) Goa KL, Noble S. Panipenem/betamipron. Drugs 2003; 63:913-925
(22) Shibuya T, Kitamura S, Tani G, et al. Evaluation of panipenem/betamipron (PAPM/BP) in pneumonia in elderly patients. J Infect Chemother 2002; 8:151-154
(23) Read RC. Evidence-based medicine: empiric antibiotic therapy in community-acquired pneumonia. J Infect 1999; 39: 171-178
(24) Fine MJ, Able TE, Yealy DM, et al. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med 1997; 336:243-250
(25) Nishimura O, Taniguchi H, Kondoh T, et al. The utility of the pneumonia PORT prediction rule for evaluating the severity of community-acquired pneumonia in Japan: the relationship between disease severity and drug-resistant Streptococcus pneumoniae. Kansenshogaku Zasshi 2002; 76:1003-1009
* From the Third Department of Internal Medicine (Drs. Kadowaki, Demura, Mizuno, Uesaka, Ameshilna, and Mivamori) and Nursing Science (Dr. Ishizaki), Medical Faculty, University, of Fukui, Fukui Prefecture, Japan.
Manuscript received April 13, 2004; revision accepted November 16, 2004.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (e-mail: permissions@chestnet.org).
Correspondence to: Maiko Kadowaki, MD, Third Department of Internal Medicine, Medical Faculty, University of Fukni, 23 Shimoaiduki Matsuoka-cho, Fukui Prefecture, 910-119.3, Japan; e-mail address: maik@fmsra.fukui-med.ac.jp
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group