Abstract
In the treatment of mild to moderate acne vulgaris, the combination of an antibiotic and benzoyl peroxide provides enhanced efficacy over the individual agents, with the potential to decrease the emergence of resistant strains of P. acnes. To evaluate treatment regimens combining the daily use of a clindamycin/benzoyl peroxide gel, a tretinoin gel, and a clindamycin gel, the current randomized, evaluator-blind study was conducted. Results demonstrate that once-daily administration of clindamycin/benzoyl peroxide gel (combination formulation) was as effective as clindamycin/benzoyl peroxide gel + tretinoin gel + clindamycin gel. Both of these regimens provided greater efficacy than tretinoin + clindamycin. Treatment with clindamycin/benzoyl peroxide demonstrated a significant benefit over other treatments at Week 2, highlighting its rapid onset of action. All regimens were safe and generally well tolerated, with less severe peeling seen in patients who received clindamycin/benzoyl peroxide. In conclusion, the regimens that included clindamycin/benzoyl peroxide were more effective than tretinoin + clindamycin in the treatment of acne vulgaris, with no clinical advantage of adding tretinoin + clindamycin to once-daily clindamycin/benzoyl peroxide treatment.
Introduction
The development of acne vulgaris is caused by follicular hyperproliferation, excessive sebum production, and inflammation, resulting in the obstruction of sebaceous follicles. Propionibacterium acnes proliferates in this environment, producing chemotactic factors and proinflammatory mediators that may result in inflammation. (1) Current therapies include topical or systemic retinoids and antibiotics to control epidermal proliferation/differentiation and proliferation of P. acnes respectively. The majority of patients present with mild to moderate acne vulgaris, with topical therapies the treatment of choice for these patients. In patients with more severe disease, systemic therapies may be required.
Tretinoin was one of the first topical retinoids to be used for the treatment of acne vulgaris. (2) Topical tretinoin normalizes desquamation of the follicular epithelium, promotes drainage of preexisting comedones, and inhibits the formation of new comedones. (3) It has been suggested that tretinoin also increases the accessibility of the follicles to other agents such as antibiotics to control P. acnes proliferation. (3)
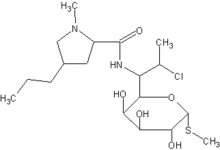
Topical antibiotics act predominantly antimicrobially, reducing follicular microbial colonization. They also demonstrate anti-inflammatory activity by suppressing chemotaxis. (4) Although P. acnes is sensitive to a range of antibiotics, the therapeutic value of individual antibiotics is dependent upon the degree to which these compounds are soluble in the lipid-rich environment within acne vulgaris lesions. Topical antibiotics of choice include erythromycin and clindamycin, which have activity against P. acnes and are relatively lipophilic. (5) Clindamycin is the more lipophilic of these antibiotics and may penetrate the acne vulgaris lesion more effectively. (1)
Lipophilic bactericidal agents such as benzoyl peroxide are also effective in reducing P. acnes in vivo and have been used in combination with antibiotics. Not only do such combinations enhance efficacy over the individual agents, they also minimize P. acnes resistance to antibacterials. For example, the combination of clindamycin and benzoyl peroxide has demonstrated significantly greater efficacy than either agent alone, (6-10) including a reduction in the emergence of resistant strains of P. acnes. (6)
Other combination therapies with clindamycin, benzoyl peroxide, and tretinoin may provide further advantages in the treatment of acne vulgaris. However, the use of tretinoin in combination with clindamycin/benzoyl peroxide has not been extensively evaluated. Therefore, a randomized, evaluator-blind, multicenter study was conducted to compare the efficacy and safety of treatment regimens combining the daily use of a clindamycin/benzoyl peroxide gel, a tretinoin gel, and a clindamycin gel in acne vulgaris.
Methods
Study Design
This was a multicenter (3 sites), randomized, evaluator-blind, parallel-group study. The efficacy and safety of the following treatment regimens were compared: once-daily treatment with the combination formulation of clindamycin 1%/benzoyl peroxide 5% gel applied in the morning (Group 1), once-daily treatment with tretinoin 0.025% gel and clindamycin 1% gel applied in the evening (Group 2), and clindamycin 1%/benzoyl peroxide 5% gel applied in the morning plus tretinoin 0.025% gel and clindamycin 1% gel applied in the evening (Group 3).
Inclusion and Exclusion Criteria
Male and female patients between 12 and 30 years of age with a definite clinical diagnosis of acne vulgaris and an Investigator's Global Acne Severity score of 1.5 to 3.0 were included in this study (Table 1). This severity scale was designed to incorporate descriptions based on the Pillsbury classification and includes specific photographs from the Leeds photographic acne scale as references. (11) Photographs were intended to provide an overall impression of acne severity at grades 1, 2, and 3, rather than encompass all criteria for each grade level.
Patients were required to have a minimum of 20 but not more than 60 combined facial papules/pustules at baseline, and a minimum of 20 facial comedones at baseline. Patients who used makeup were required to have used the same brand for a minimum of 2 weeks prior to baseline and to agree not to change brands during the study. Females of childbearing age were required to have a negative urine pregnancy test and to use appropriate birth control during the study.
Patients with more than 2 facial nodulo-cystic lesions, excluding the nose, were excluded from the study, as were those with facial bacterial folliculitis. Additionally, patients were excluded under the following conditions: they were treated with systemic antibiotics or systemic anti-acne drugs (except oral retinoids as described below) within 4 weeks prior to the study; they were treated with topical medications (either prescription or over the counter) for acne vulgaris within the past 2 weeks; they received oral retinoids within the past 6 months or topical retinoids to the face within 4 weeks; or they received laser therapy or electrodesiccation to the face within the past 6 weeks. Patients were also excluded if they had known sensitivity to any of the study medication ingredients or were pregnant or lactating.
Treatments
Patients were randomly assigned to 1 of 3 treatment regimens: clindamycin 1%/benzoyl peroxide 5% gel (BenzaClin[R] Topical Gel, Dermik Laboratories, Berwyn, PA); 0.025% tretinoin gel (Retin-A gel, Ortho Dermatological, Skillman, NJ) plus 1% clindamycin gel (Cleocin-T gel, Pharmacia & Upjohn Company, Kalamazoo, MI); or a combination of both regimens. The regimens in this study all differed from those listed in the package inserts for each product when prescribed as monotherapy. Treatment allocation was completed by PRACS Institute, Ltd., using a computer-generated randomization schedule. Study medication was dispensed by an independent third-party dispenser to nullify any differences in product packaging and was packaged as individual patient kits that included all necessary supplies for a specific visit period. Patients were instructed to apply a thin film of study medication to their faces after washing with a simple soap and warm water and patting dry. Patients randomized to clindamycin/benzoyl peroxide were instructed to apply the study medication once daily in the morning; those randomized to tretinoin + clindamycin were instructed to apply both products in the evening (tretinoin first, followed by clindamycin); and those randomized to clindamycin/benzoyl peroxide + tretinoin + clindamycin were instructed to apply each study drug as outlined above. Patients were not to bathe, shower, wash, or swim for 4 hours after study drug application.
Clinical Assessments
The primary efficacy assessments were mean percent change from baseline in number of inflammatory lesions, non-inflammatory lesions, and total lesions at the final visit (Week 10) and percent of treatment successes (defined as an Investigator's Global Acne Severity score of 0 [clear; no inflammatory lesions] to 0.5 [sparse comedones, with very few or no inflammatory lesions]) at Week 10. Secondary efficacy assessments were the above outcome measures evaluated at each visit.
Sites were instructed to have the same investigator assess the patient's facial acne at each study visit. Lesion count was assessed by counting the number of facial open and closed comedones, pustules, papules, and nodulo-cystic lesions above the jaw line to the hairline, excluding lesions involving the eyes, nose, and scalp. The Investigator's Global Evaluation is the investigator's comprehensive evaluation of the patient's overall acne condition. In addition to number of lesions, the overall condition of acne included (but was not limited to) size of lesions, overall degree of inflammation, general erythema of the face (both lesions and background), and skin condition.
Clinical assessments were conducted at baseline at Days 14 (Week 2), 28 (Week 4), 49 (Week 7), and 70 (Week 10) [+ or -] 4 days. All study visits included evaluation of lesion count, acne severity, and local irritation (Signs/Symptoms of Irritation assessment, with scores ranging from 0 [none] to 3 [severe, marked/intense]). The baseline visit also included a medical history, pregnancy test for females, and instruction on medication application and completion of patient diaries. Adverse events and treatment compliance were evaluated at all study visits (excluding baseline). The clinical course of each adverse event was followed until resolution.
Analysis of Data
The intent-to-treat (ITT) population was defined as all patients who received at least 1 dose of study drug. Baseline treatment group differences for continuous variables were analyzed by a 2-way analysis of variance (ANOVA) when normality and homogeneity assumptions could be supported, or by the Friedman's test when they could not. Baseline treatment group differences for categorical variables were evaluated by Cochran-Mantel-Haenszel procedures for pooling results across multiple clinical sites. Analyses of clinical efficacy parameters were performed on the efficacy analysis population, defined as those patients who completed the study with a dosing compliance rate of 80% to 120%, did not have significant protocol violations, and returned for the final study visit (Week 10) within the specified 4-day window. Treatment group differences in mean percent reduction in lesion counts were evaluated using ANOVA (with factors of treatment and center) when normality and homogeneity assumptions could be supported or by the Friedman's test when they could not. Treatment group differences in proportion of patients who were treatment successes (ie, Investigator's Global Acne Severity score of 0-0.5) were analyzed using a 2-sided z-test adjusted for center using Yates' continuity correction. Significance was determined at the 0.05 level using 2-sided tests. Safety analyses were performed on the ITT population with summary statistics generated for all adverse events.
Results
Patient Characteristics
Of 132 enrolled patients who received at least 1 dose of study drug (ITT population), 109 patients completed the study. Reasons for discontinuation included lost to follow-up (n = 14), consent withdrawn (n = 3), noncompliance or protocol violation (n = 2), adverse event (n = 2), use of prohibited concomitant medication (n = 1), and other (n = 1). A total of 26 patients who completed the study were excluded from the efficacy population due to a failure to appear for the final assessment within the 4-day assessment window (n = 16), use of prohibited medication (n = 6 [with 1 patient also outside of the 4-day assessment window]), and incomplete compliance (n = 5).
Demographic and baseline characteristics of the ITT population are presented in Table 2. At baseline, patients in the 3 groups had similar numbers of papules, although patients in Group 2 (tretinoin + clindamycin) had significantly higher numbers of comedones compared with Groups 1 and 3 and patients in Group 1 (clindamycin/benzoyl peroxide) had significantly lower numbers of pustules compared with Groups 2 and 3. The mean Investigator's Global Acne Severity score was 2.1 to 2.2 in all groups.
Lesion Counts
The overall number of inflammatory lesions was considerably reduced during the 10-week study period. The mean percent reduction from baseline in inflammatory lesions was 65.7% for Group 1 (clindamycin/benzoyl peroxide), 52.5% for Group 2 (tretinoin + clindamycin), and 69.3% for Group 3 (clindamycin/benzoyl peroxide + tretinoin + clindamycin) (Figure 1). At Week 10, the mean percent reduction was significantly greater for Group 1 compared with Group 2 (P = .05) and for Group 3 compared with Group 2 (P = .02). There was no significant difference between Group 1 and Group 3 (P = .69). At Week 2, the percent reduction for Group 1 was significantly greater than both Group 2 (P = .01) and Group 3 (P = .02), highlighting the rapid onset of action of clindamycin/benzoyl peroxide.
The number of non-inflammatory lesions was also reduced during the study. At Week 10, numerically greater mean percent reductions were seen in the 2 groups that included clindamycin/benzoyl peroxide compared with the tretinoin + clindamycin group (Group 1 = 57.2%, Group 3 = 61.0% vs. Group 2 = 46.2%) (Figure 2). Reductions in total lesion counts at Week 10 followed the same pattern (Group 1 = 61.4%, Group 3 = 62.6% vs. Group 2 = 49.6%) (Figure 3).
Investigator's Global Acne Severity Score
At Week 10, significantly more patients in Group 3 achieved an Investigator's Global Acne Severity score of 0 to 0.5 compared with patients in Group 2 (50% vs. 14%, P = .01). There was no statistical difference between the numbers of patients achieving an Investigator's Global Acne Severity score of 0 to 0.5 between Group 1 and Group 3. Patients in Group 1 had a success rate of 29%, approximately twice as high as Group 2, but this difference did not reach statistical significance.
[FIGURE 1 OMITTED]
[FIGURE 2 OMITTED]
[FIGURE 3 OMITTED]
Tolerability
All treatment regimens were safe and generally well tolerated. Substantially more adverse events were reported for the combination regimen of clindamycin/benzoyl peroxide + tretinoin + clindamycin than for either regimen alone. Overall, more application site reactions occurred with tretinoin + clindamycin than with clindamycin/benzoyl peroxide. The most common adverse events were application site irritation and application site dryness (Table 3). Adverse events were primarily mild to moderate in severity. During the study, the 4 severe adverse events which were reported included application site dryness (1 patient each in Groups 1 and 2), application site irritation (1 patient in Group 2), and facial peeling (1 patient in Group 2). All patients recovered without sequelae. Two patients (in Group 3) discontinued due to facial burning of moderate severity, with discontinuations occurring within the first week of study drug administration. There were no serious adverse events reported during the trial.
Evaluation of the signs and symptoms of irritation demonstrated that at study end patients treated with clindamycin/benzoyl peroxide experienced less severe peeling than those treated with tretinoin + clindamycin or clindamycin/benzoyl peroxide + tretinoin + clindamycin (mean [SD] Signs/Symptoms peeling scores of 0.14 [0.42], 0.26 [0.44], and 0.20 [0.46], respectively). Severity of dryness, erythema, and oiliness (additional signs and symptoms of irritation) were similar among the treatment groups. Generally, signs and symptoms of irritation decreased by approximately 50% over the time course of the study in each of the treatment groups.
Discussion
In this 10-week randomized, evaluator-blind, comparator study, the effectiveness of 3 treatment regimens was compared. Overall, there was no apparent benefit of the multiple-agent regimens over the combination formulation regimen alone in the reduction in lesions, with clindamycin/benzoyl peroxide gel as effective as the most complicated regimen of clindamycin/benzoyl peroxide gel + tretinoin gel + clindamycin gel. Although numerically greater effects were seen for clindamycin/benzoyl peroxide + tretinoin + clindamycin compared with clindamycin/benzoyl peroxide for each primary efficacy variable, differences were not statistically significant. A significant benefit of clindamycin/benzoyl peroxide over tretinoin + clindamycin was observed in the reduction of inflammatory lesions. Differences among treatment groups reached significance at Week 2, highlighting the rapid onset of action of clindamycin/benzoyl peroxide. Treatment group differences in inflammatory lesions are especially noteworthy, as inflammatory lesions are often the impetus for seeking treatment, suggesting that these lesions are of greatest concern to patients. Results of this study indicate that there is no significant clinical benefit of additional therapies over the once-daily application of clindamycin/benzoyl peroxide gel.
The approval of clindamycin 1%/benzoyl peroxide 5% gel (BenzaClin[R]) was based on twice-daily dosing. (12) Therefore, it is notable that once-daily administration was as effective in the improvement of lesions as the 2 other treatment regimens, indicating that once-daily dosing provides substantial clinical benefit. All treatments were safe and generally well tolerated with no major safety concerns with any of the regimens. None of the treatments resulted in major irritation issues, although clindamycin/benzoyl peroxide + tretinoin + clindamycin resulted in a greater proportion of patients experiencing local reactions. Not surprisingly, the treatment that included clindamycin/benzoyl peroxide and tretinoin + clindamycin resulted in more adverse events than either of the treatment regimens alone. As expected, fewer application site reactions occurred with clindamycin/benzoyl peroxide than with tretinoin + clindamycin. Evaluation of the signs and symptoms of irritation revealed that peeling was less severe in patients treated with clindamycin/benzoyl peroxide compared with the other 2 treatment regimens. Assessments of dryness, erythema, and oiliness were similar among the treatment groups.
In conclusion, results of this randomized, evaluator-blind, multicenter trial indicate that once-daily treatment with clindamycin 1%/benzoyl peroxide 5% gel provides efficacy similar to that of the more complicated regimen of clindamycin 1%/benzoyl peroxide 5% gel + tretinoin 0.025% gel + clindamycin 1% gel, with better tolerability.
Conflict of Interest/Financial Disclosures: Dr. Gold has received honoraria for speaking on behalf of Dermik Laboratories. Dr. Bowman and Dr. Nasir have nothing to disclose. Mr. Vamvakias is an employee of Dermik Laboratories. This study was supported by Dermik Laboratories.
References
1. Leyden JJ. Therapy for acne vulgaris. N Engl J Med. 1997;336:1156-1162.
2. Swinyer LJ, Swinyer TA, Britt MR. Topical agents alone in acne. A blind assessment study. JAMA. 1980;243:1640-1643.
3. Berson DS, Shalita AR. The treatment of acne: The role of combination therapies. J Am Acad Dermatol. 1995;32:S31-S41.
4. Krautheim A, Gollnick HPM. Acne: topical treatment. Clin Dermatol. 2004;22:398-407.
5. Gollnick H, Schramm M. Topical drug treatment in acne. Dermatology. 1998;196:119-125.
6. Cunliffe WJ, Holland KT, Bojar R, Levy SF. A randomized, double-blind comparison of a clindamycin phosphate/benzoyl peroxide gel formulation and a matching clindamycin gel with respect to microbiologic activity and clinical efficacy in the topical treatment of acne vulgaris. Clin Ther. 2002;24:1117-1133.
7. Leyden JJ, Berger RS, Dunlap FE, Ellis CN, Connolly MA, Levy SF. Comparison of the efficacy and safety of a combination topical gel formulation of benzoyl peroxide and clindamycin with benzoyl peroxide, clindamycin and vehicle gel in the treatment of acne vulgaris. Am J Clin Dermatol. 2001;2:33-39.
8. Leyden JJ, Kaidbey K, Levy SF. The combination formulation of clindamycin 1% plus benzoyl peroxide 5% versus 3 different formulations of topical clindamycin alone in the reduction of Propionibacterium acnes. An in vivo comparative study. Am J Clin Dermatol. 2001;2:263-266.
9. Leyden JJ. Effect of topical benzoyl peroxide/clindamycin versus topical clindamycin and vehicle in the reduction of Propionibacterium acnes. Cutis. 2002;69:475-480.
10. Tschen EH, Katz HI, Jones TM, et al. A combination benzoyl peroxide and clindamycin topical gel compared with benzoyl peroxide, clindamycin phosphate, and vehicle in the treatment of acne vulgaris. Cutis. 2001;67:165-169.
11. Burke BM, Cunliffe WJ. The assessment of acne vulgaris--the Leeds technique. Br J Dermatol. 1984;111:83-92.
12. BenzaClin (clindamycin 1%/benzoyl peroxide 5% gel) prescribing information. Berwyn, PA: Dermik Laboratories;2005.
Address for Correspondence
Steven Bowman, MD
Tampa Bay Medical Research, Inc.
3251 McMullen Booth Rd, #301
Clearwater, FL 33761
Phone: 727-724-3316
Fax: 727-725-5562
e-mail: sbowman11@aol.com
Steven Bowman MD, (a) Michael Gold MD, (b) Adnan Nasir MD PhD, (c) George Vamvakias (d)
a. Tampa Bay Medical Research, Inc., Clearwater, FL
b. Tennessee Clinical Research Center, Nashville, TN
c. Department of Dermatology, University of North Carolina Chapel Hill, Chapel Hill, NC
d. Dermik Laboratories, Berwyn, PA
COPYRIGHT 2005 Journal of Drugs in Dermatology, Inc.
COPYRIGHT 2005 Gale Group