ABSTRACT. Background: Some patients who have short bowel syndrome (SBS) have high intestinal outputs, which increases the risk of dehydration and fluid-electrolyte abnormalities and impairs quality of life. Methods: We evaluated the use of clonidine, an [alpha]^sub 2^-adrenergic receptor agonist, in 2 patients with SBS and high intestinal outputs, who were refractory to conventional therapy with antidiarrheal and antisecretory agents (loperamide, belladonna, opiates, somatostatin, histamine^sub 2^ receptor antagonists and proton pump inhibitors). The first patient (case 1) was a 29-year-old woman who had 175 cm of small bowel anastamosed to 8 cm of descending colon, ending in a colostomy. The second patient (case 2) was a 22-year-old man who had 30 cm of jejunum anastomosed to 30 cm of sigmoid colon and rectum. Results: The addition of clonidine, 0.1 mg per os (PO) 2 times per day, to the treatment regimen of case 1 decreased her ostomy output from ~4 L/day to ~1 L/day, eliminating the need for parenteral nutrition and fluids and decreasing the need for opiate therapy. The addition of clonidine, 0.2 mg PO 2 times per day in case 2 resulted in decreased rectal outputs from ~4 L/day to ~1.5 L/day. Conclusions: These results demonstrate that clonidine can effectively reduce intestinal fluid and electrolyte losses and should be considered as an additional treatment option in patients with SBS and high intestinal outputs. (Journal of Parenteral and Enteral Nutrition 28:265-268, 2004)
Resection of the small intestine can affect the absorption of ingested nutrients; the severity of malabsorption depends on the length and functional status of the remaining intestine and the site of intestinal resection. Short-bowel syndrome (SBS) is used to describe patients who have had massive intestinal resection (
Patients who have SBS and a high intestinal output are at increased risk for complications associated with malabsorption and fluid-electrolyte losses. These patients often need long-term home parenteral nutrition (HPN) for normal function and survival. However, the use of HPN is associated with considerable medical complications, including catheter-related infections,1 liver disease and cholestasis,2'3 and metabolic bone disease.4 In addition, high ostomy outputs make it more difficult to provide ostomy care and adequate fluid-electrolyte replacement. Therefore, an important therapeutic goal for patients with SBS who have a high intestinal output is to minimize fluid and electrolyte losses by slowing intestinal transit and decreasing intestinal secretions. Treatment with modified diets, oral rehydration solutions, antimotility drugs, and antisecretory agents can decrease parenteral fluid and nutrient requirements and sometimes completely eliminate the need for HPN.5'6 Effective therapy with loperamide, belladonna, opiates, somatostatin, histamine2 receptor antagonists, and proton pump inhibitors has been reported.5'6 However, many patients still have excessive ostomy outputs despite such aggressive therapy.
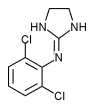
Clonidine is an a2-adrenergic receptor agonist that inhibits gastrointestinal motility by both central and peripheral action and increases intestinal sodium and water absorption and decreases bicarbonate secretion by direct activation of postsynaptic enterocyte a2-adrenoreceptors.7'8 These intestinal effects provide a rationale for the use of clonidine in treating specific forms of chronic diarrhea, including diabetic autonomie neuropathy,9 carcinoid syndrome,10 and diarrhea-predominant irritable bowel syndrome.11 Clonidine has also been reported to decrease gastrointestinal output in patients who had high intestinal output after smallbowel transplantation.12
We report 2 patients with SBS and high intestinal outputs who failed to adequately reduce fluid and electrolyte losses with conventional dietary, antidiarrheal, and antisecretory therapy. Both patients experienced rapid and marked decreases in intestinal output after treatment with clonidine, leading to clinically significant changes in their quality of life. These cases support the consideration of clonidine as a therapeutic agent in managing selected patients with SBS.
case 1
A 29-year-old-woman with adenocarcinoma of the anal verge was treated with radiation therapy and chemotherapy, followed by local rectal resection and colostomy formation. Her postoperative course was complicated by radiation enteritis, intestinal ischemia, multiple intestinal microperforations, and peritonitis. Her weight decreased by 30%, from 68 kg (body mass index [BMI] of 24.2 kg/m^sup 2^) to 47 kg (BMI of 16.7 kg/m^sup 2^). These complications required extensive intestinal resection, and she was left with 175 cm of small bowel distal to the ligament of Treitz, anastomosed to 8 cm of descending colon, and ending in a colostomy. The patient's colostomy started functioning on the eighth day after surgery, and she began receiving oral feedings, which were advanced from clear liquids to a regular diet. Treatment with a proton pump inhibitor, antidiarrheal medications including diphenoxylate and loperamide, and finally octreotide were started because of high ostomy output. There was no evidence of partial bowel obstruction or intra-abdominal pathology by either clinical examination or computerized abdominal tomography. She was discharged 12 days after surgery, with instructions for use of codeine (15 mg per os (PO) q 6 hours) and octreotide (100 µg sc every day) therapy.
At home, the patient's ostomy output continued to increase to >4 L/day despite adding 4 drops deodorized tincture of opium 3 times per day to her therapeutic regimen. She was readmitted to the hospital 5 weeks after discharge because of fatigue, weight loss, dehydration, and electrolyte abnormalities. At that time, she weighed 41 kg (BMI 14.7 kg/m^sup 2^) and had hypokalemia (serum potassium 3.1 mg/dL) and hypomagnesemia (serum magnesium 0.6 mg/dL). An upper gastrointestinal series with small-bowel follow-through revealed approximately 175 cm of normal small bowel anastomosed to 8 cm of descending colon without evidence of strictures, fistulas, or mucosal abnormalities. She was treated with central parenteral nutrition (CPN), and her antidiarrheal and antisecretory therapies were changed to belladonna and opium capsules (30 mg powdered belladonna and 50 mg powdered opium 4 times per day) and omeprazole (20 mg 2 times per day). In addition, oral fluids were restricted to 500 mL/day of caffeine-free drinks and 2 L/day of oral rehydration solution, formulated at Washington University and containing 105 mEq sodium/L, 100 mEq chloride, 10 mEq citrate, and 20 g polycose.13 Although this therapeutic regimen decreased fluid losses, ostomy output remained high at 4 L/day. Increasing the dose of belladonna and opium (to 2 mL [0.6 mg] 4 times per day and 1.2 mL [0.12 mg] 4 times per day in liquid form, respectively) caused drug side effects of nausea, blurry vision, and dry mouth without improvement in ostomy output, and the dose of each medication was decreased to 1 mL (0.3 mg belladonna and 0.1 mg opium) 4 times per day. A trial of cholestyramine therapy, 2 g PO 4 times per day, was also ineffective. The patient required 4 L/day of CPN and 1 L/day of normal saline to maintain fluid and electrolyte balance, as determined by body weight, measured total fluid input and urine output, and serum electrolyte concentrations.
Clonidine therapy was started in an effort to reduce fluid and electrolyte losses. A low dose was given initially (0.025 mg PO 2 times per day) because of low blood pressure (80/50 mm Hg), and increased gradually over 2 months to 0.1 mg PO 2 times per day. The patient did not develop any symptoms of hypotension, and there was no evidence of a decrease in either systolic or diastolic blood pressure throughout treatment. In fact, the reduction in fluid losses was associated with an increase in blood pressure to 90/60 mm Hg.
Within 1 week of treatment, ostomy outputs decreased to 2.5 L/day and continued to decrease with increasing doses of clom'dine to 1 L/day by 16 weeks of therapy (Fig. 1). Belladonna and opium doses were reduced by more than half, and omeprazole therapy was stopped completely. By 6 months of therapy, intestinal output was
Case 2
A 22-year-old-man (BMI 23 kg/m^sup 2^) experienced severe abdominal trauma because of a motor vehicle crash. The injury caused intestinal ischemia and necrosis that required massive intestinal resection. After 2 operations, he was left with 30 cm of jejunum anastomosed to 30 cm of sigmoid colon and rectum. he consumed a diet containing approximately 3500 kilocalories (kcaiyday and 2 L/day of oral rehydration solution13 and required daily HPN containing 2.5 L of fluid a day and an additional liter of normal saline daily. he had 6 to 7 bowel movements a day and a rectal output of approximately 4 L/day, despite treatment with deodorized tincture of opium (1.2 mL 4 times per day) and belladonna (0.6 mL 4 times per day). The patient maintained a stable weight of 64.5 kg (BMI 19.6 kg/m^sup 2^) with this treatment regimen and was able to attend college, but the marked diarrhea and need for prolonged daily intravenous (IV) infusions interfered with his normal activities.
Sixteen months after his injury, clonidine therapy was started at 0.05 mg PO 2 times per day and was gradually increased over 6 months to 0.2 mg PO 2 times per day in addition to the tincture of opium and belladonna. Within 2 weeks of starting clonidine treatment, the patient's rectal output decreased by >2 L/day (Fig. 1), his weight increased by 2 kg, and his blood pressure was maintained at normal levels. At 6 months of clonidine therapy, his weight had increased by 10% to 70.9 kg (BMI 21.6 kg/m^sup 2^), and he was experiencing fewer bowel movements (3/day). After 15 months of clonidine therapy, he was still having only 3 bowel movements and 1.5 L of stool output per day, his weight was maintained at 75 kg (BMI 22.8 kg/m^sup 2^) with 3 L of a HPN solution infused 8 hours/day. The decrease in rectal output and time required for IV infusions has increased his ability to participate in normal daily activities.
DISCUSSION
Many patients with SBS have high ostomy or rectal outputs, which affects their daily function and quality of life and requires large volume parenteral fluid and electrolyte replacement. We report 2 patients with SBS who continued to have large-volume intestinal outputs despite aggressive therapy with standard antidiarrheal and antisecretory agents but who experienced a marked reduction in fluid output (2.5 L to 3 L/day) with clonidine treatment. In 1 patient, clonidine therapy permitted complete cessation of HPN and saline infusions and decreased the doses of opium and belladonna needed to control diarrhea. This patient is now able to maintain a normal nutritional status with an oral diet. In the second patient, home saline infusions were stopped, the volume of HPN was decreased, and electrolyte management was made easier by clonidine therapy. Our experience with these patients suggests that clonidine should be considered a therapeutic agent in the management of patients with SBS.
Clonidine is an a2-adrenergic receptor agonist that decreases diarrhea by increasing sodium and water absorption and decreasing bicarbonate secretion. Clonidine enhances sodium absorption in rabbit villus cells by increasing intercellular pH and stimulating sodium:hydrogen (Na:H) exchange and inhibits bicarbonate secretion from crypt cells by decreasing intercellular pH and inhibiting Na:H exchange.7 In 1 study, conducted in healthy human volunteers, clonidine caused a 48% reduction in the volume of diarrhea induced by ingesting an oral electrolyte solution.14 The decrease in diarrhea was caused by an enhanced rate of fluid absorption and by a marked decrease gastrointestinal motility.
Clonidine has central and peripheral inhibitory effects on gastrointestinal motility, which are mediated through its action on [alpha]^sub 2^-adrenergic receptors.8 In rats, clonidine has been shown to delay gastric emptying,15 slow down small-bowel transit,16 and decrease colonie motility.17 The gastric effect involves both central and peripheral receptors.18 However, the effect of clonidine on human intestinal motility is not clear, because of conflicting results from different studies. Two studies conducted in healthy male volunteers demonstrated that 0.3 mg of clonidine caused a marked prolongation of small-intestinal transit time, determined by using the hydrogen-breath test.19'20 However, 2 other studies conducted in healthy men and women found this dose of clonidine did not affect gastric emptying21 or small-bowel transit time,22'23 determined by using radiolabeled markers.
Clonidine is approved for use by the US Food and Drug Administration to treat hypertension.24'25 It is absorbed rapidly by the upper gastrointestinal tract, and decreases in blood pressure are seen within 30 to 60 minutes after an oral dose. About half of the absorbed dose is metabolized by the liver and half is excreted unchanged by the kidneys. The half-life of clonidine is 12 to 16 hours. The therapeutic effects of oral clonidine treatment observed in our patients suggest that clonidine absorption and action are not seriously affected by massive intestinal resection and impaired intestinal absorptive function.
The most commonly reported side effects of clonidine treatment are dry mouth, drowsiness, dizziness, sedation, and constipation. Hypotension can also occur and is a particular concern when clonidine is used to treat patients with high intestinal output because of the possibility of preexisting low intravascular volume and blood pressure caused by fluid losses. For this reason, we cautiously initiated clonidine treatment at a very low dose (0.05 mg PO 2 times per day) in our patients and increased the dose every week by 0.05 mg/day, if tolerated, until a satisfactory therapeutic effect was achieved or we reached a dose of 0.2 mg PO 2 times per day. Neither of our patients experienced side effects or hypotension with this approach. In fact, blood pressure increased in both patients after starting clonidine treatment, presumably because of a reduction in fluid losses. Nonetheless, we recommend slow titration of clonidine and careful blood pressure monitoring in patients with SBS, particularly in children, elderly adults, and those with hepatic or renal impairment because of the increased risk of toxicity.
In summary, we found that clonidine therapy reduced fluid losses and simplified the nutrition management of 2 patients with SBS who had high intestinal outputs. Clonidine treatment was initiated after our patients failed to demonstrate an adequate therapeutic response to conventional antidiarrheal and antisecretory therapy.
Our experience suggests that clonidine should be considered early in the treatment course of patients with SBS because it might reduce or eliminate the need for opiate therapy. Narcotic antidiarrheal agents are expensive and addicting and can cause sedation, sleepiness, and mental status changes. However, additional studies in patients with SBS are needed to confirm our results and to determine whether clonidine is more effective than other antidiarrheals agents in patients with SBS.
REFERENCES
1. Klein S, Rubin D. Enterai and parenteral nutrition. In: Feldman M, Freidman L, Sleisenger M, eds. Sleisenger & Fordtran's Gastrointestinal and Liver Disease. 7th ed. Philadelphia, PA: W. B. Saunders Co; 2002:287-309.
2. Klein S. Total parenteral nutrition and the liver. In: Schiff L, Schiff ER, eds. Disease of the Liver. 7th ed. Philadelphia, PA: J. B. Lippincott Co; 1993:1505-1516.
3. Messing B, Bories C, Kunstlinger F, Bernier JJ. Does total parenteral nutrition induce gallbladder sludge formation and lithiasis? Gastroenterology. 1983;84:1012-1019.
4. Klein GL, Coburn JW. Parenteral nutrition: effect on bone and mineral homeostasis. Annu Rev Nutr. 1991;11:93-119.
5. Nightingale JMD. Management of patients with a short bowel. Nutrition. 1999;15:633-637.
6. Klein S, Jeejeebhoy KN. The malnourished patient: nutritional assessment and management. In: Feldman M, Freidman L, Sleisenger M, eds. Sleisenger & Fordtrans Gastrointestinal and Liver Disease. 7th ed. Philadelphia, PA: W. B. Saunders Co; 2002:265-285.
7. Sundaram U. Mechanism of intestinal absorption: effect of clonidine on rabbit ileal villus and crypt cells. J Clin Invest. 1995;95:2187-2194.
8. De Ponti F, Giaroni C, Cosentino M, Lecchini S, Frigo G. Adrenergic mechanisms in the control of gastrointestinal motility: from basic science to clinical applications. Pharmacol Ther. 1996;69: 59-78.
9. Fedorak RN, Field M, Chang EB. Treatment of diabetic diarrhea with clonidine. Ann Intern Med. 1985;102:197-199.
10. Schworer H, Munke H, Stockmann F, Ramadori G. Treatment of diarrhea in carcinoid syndrome with ondansetron, tropisetron, and clonidine. Am J Gastroenterol. 1995;94:645-648.
11. Camilleri M, Kim D-Y, McKinzie S, et al. A randomized, controlled exploratory study of clonidine in diarrhea-predominant irritable bowel syndrome. Clin Gastroenterol Hepatol. 2003;1: 111-121.
12. Rovera G, Furukawa H, Reyes J, Todo S, Houston W. The use of clonidine for the treatment of high intestinal output following small bowel transplantation. Transplant Proc. 1997;29:1853-1854.
13. Klein S. Nutritional therapy. In: Ahya S, Flood K, Paranjothi S, eds. The Washington Manual of Medical Therapeutics. 30th ed. Philadelphia, PA: Lippincott Williams & Wilkens; 2000:27-42.
14. Schiller LR, Santa Ana CA, Morawski SG, Fordtran JS. Studies of the antidiarrheal action of clonidine: effects on motility and intestinal absorption. Gastroenterology. 1985;89:982-988.
15. Asai T, Vickers MD, Power I. Clonidine inhibits gastric motility in the rat. Eur J Anaesthesiol. 1997;14:316-319.
16. Tadano T, Kisara K, Stewart JJ. A comparison of peripheral and central effects of clonidine on rat intestinal transit. Res Commun Chem Pathol Pharmacol. 1992;78:161-179.
17. Yamamoto O, Niida H, Tajima K, et al. Inhibition of stressstimulated colonie propulsion by a-2 adrenoceptor antagonists in rats. Neurogastroenterol Motil. 1998;10:523-532.
18. Nagata M, Osumi Y. Central alpha-2 adrenoceptor-mediated inhibition of gastric motility in rats. Jpn J Pharmacol. 1993;62: 329-330.
19. Baumer P, Danays T, Lion L, Cosnes J, Gendre JP, Le Quintrec Y. Effect of clonidine on oro-cecal transit time in normal man. Ann Gastroenterol Hepatol (Paris). 1989;25:5-9.
20. Rubinoff MJ, Piccione PR, Holt PR. Clonidine prolongs human small intestine transit time: use of the lactulose-breath hydrogen test. Am J Gastroenterol. 1989;84:372-374.
21. Baxter AJ, Edwards CA, Holden S, Cunningham KM, Welch IM, Read NW. The effect of two alpha-2 adrenoreceptor agonists and an antagonist on gastric emptying and mouth to cecum transit time in humans. Aliment Pharmacol Ther. 1987;l:649-655.
22. Viramontes BE, Malcolm A, Camilleri M, et al. Effects of an [alpha]-2 adrenergic agonist on gastrointestinal transit, colonie motility, and sensation in humans. Am J Physiol Gastrointest Liver Physiol. 2001;281:G1468-G1476.
23. Gregersen H, Kraglund K, Rittig S, Tottrup A. The effect of a new selective a-2 adrenoreceptor antagonist, idazoxan, and the agonist, clonidine, on fasting antroduodenal motility in healthy volunteers. Aliment Pharmacol Ther. 1989;3:435-443.
24. Lowenthal DT, Metzek KM, MacGregor TR. Clinical pharmacokinetics of clonidine. Clin Pharmacokinet. 1988;14:287-310.
25. Davies DS, Wing AM, Reid JL, Neill DM, Tippett P, Dollery CT. Pharmacokinetics and concentration-effect relationships of intravenous and oral clonidine. Clin Pharmacol Ther. 1977;21: 593-601.
Karen McDoniel, MS*; Beth Taylor, MS*; Way Huey, PhD*; Kelly Eiden, MS*; Sharon Everett, BSN*; James Fleshman, MD[dagger]; Timothy G. Buchman, MD, PhD[dagger]; David Alpers, MD*[double dagger]; and Samuel Klein, MD*[double dagger]
From the *Nutrition Support Service, Barnes-Jewish Hospital; and the [dagger]Department of Surgery and [double dagger]Center for Human Nutrition, Washington University School of Medicine, St. Louis, Missouri
Received for publication September 23, 2003.
Accepted for publication April 6, 2004.
Correspondence: Samuel Klein, MD, Washington University School of Medicine, 660 S. Euclid Ave., Box 8031, St. Louis, MO 63110. Electronic mail may be sent to sklein@im.wustl.edu.
Copyright American Society for Parenteral and Enteral Nutrition Jul/Aug 2004
Provided by ProQuest Information and Learning Company. All rights Reserved