hospitalnursing
* Nutrition for acutely ill patients
* Dehydration on the job
Learn who's at risk and how to prevent these painful infections.
For bacteria, an indwelling urethral catheter is like a red carpet to the urinary tract. Any invasive device placed in the bladder gives urinary pathogens (uropathogens) a direct route in, making the patient highly susceptible to urinary tract infections (UTIs).
Catheterized and other susceptible patients develop UTIs when uropathogens ascend and inflame the urethra or bladder in the lower urinary tract or the ureters or kidneys in the upper urinary tract. Besides causing painful symptoms, UTIs can lead to serious complications, such as renal scarring and bacteremia, and extend the patient's length of stay.
In this article, I'll describe types of UTIs, patients who are particularly susceptible, and ways to prevent or treat UTIs in your patients.
Identifying susceptible patients
Patients with indwelling urethral catheters aren't the only ones susceptible to UTIs. Because women have a shorter urethra and more bacteria near their urethral opening, they're more susceptible than men. Sexual activity, diaphragm use, and menopause each creates conditions conducive to UTI development in women.
Men under age 60 are less likely to get UTIs, but the risk increases after age 60 as the incidence of prostatitis increases.
Patients with chronic prostatitis, chronic pyelonephritis, or infected bladder stones are also susceptible to developing UTIs because these conditions constantly supply uropathogens to the urinary tract. Patients who are immunocompromised or have diabetes are susceptible too because their bodies may lack the ability to fight off ascending uropathogens.
Free-flowing and uncomplicated
A UTI is considered either uncomplicated or complicated, depending on its cause, signs, and symptoms. Uncomplicated UTIs, common in women of reproductive age who are sexually active, usually involve the lower urinary tract and occur in patients with normal urinary tract structure. Generally, bacteria from the perineum, periurethral area, vagina, or lower gastrointestinal tract infect the urethra (urethritis), the bladder (cystitis), or the upper urinary tract.
A patient with an uncomplicated lower UTI typically complains of dysuria and urinary frequency and urgency; however, she likely won't have a fever or systemic symptoms. About 20% of women with an uncomplicated UTI have suprapubic tenderness and pain. Signs and symptoms such as fever, nausea and vomiting, abdominal pain, and costovertebral-angle tenderness are more likely to occur in a patient with pyelonephritis. If your patient is symptomatic, the health care provider will order a routine urinalysis and possibly a urine culture to support a diagnosis of UTI.
* Routine urinalysis requires a clean-catch urine specimen. If the results are positive for nitrites (which indicates bacteriuria), leukocyte esterase (associated with pyuria), or protein (associated with presence of protein-containing substances such as white blood cells, mucus, and bacteria), a urine culture is necessary.
* A urine culture can identify causative pathogens, which commonly include Escherichia coli or Staphylococcus saprophyticus in uncomplicated UTI. Instructing your patient on the proper way to collect the specimen is essential to prevent contamination (see Collecting a Urine Culture Specimen and Interpreting Test Results).
Complicated, recurrent and resistant
Difficult to resolve and likely to recur, a complicated UTI usually involves the upper urinary tract and may involve the bloodstream. Complicated UTIs commonly occur in patients with urinary tract abnormalities such as bladder stones, prostatitis, strictures, tumors, neurogenic disorders, bladder diverticula, and vesicoureteral reflux. These abnormalities contribute to urinary retention and stagnation, increasing the risk of a complicated UTI.
Usually affecting middle-aged and older men and women, a complicated UTI is more likely than uncomplicated UTI to involve antibiotic-resistant microorganisms. The usual suspects include Enterococcus faecalis, Staphylococcus aureus, and species of Klebsiella, Proteus, Enterobacter, Pseudomonas, and Serratia.
A patient with an upper UTI may have pyuria, fever, chills, suprapubic pain, and costovertebral tendemess. He may also have an increased white blood cell count and proteinuria.
A complicated UTI may be a recurrence or a reinfection. Recurrent lower or upper infection caused by the original pathogen occurs within 2 weeks of completing antibiotic therapy. Reinfection caused by the original or a different pathogen occurs 2 weeks or more after completing antibiotic therapy The health care provider should further evaluate a patient with a reinfection or a recurrent infection, paying particular attention to underlying causes.
Coming from the catheter
Uropathogens can easily make their way up a urethral catheter and into the urinary tract system. Although most patients with a catheter-related UTI are asymptomatic, fever and signs of sepsis may signal infection.
Complications of UTI due to short-term catheterization include fever, acute pyelonephritis, bacteremia, and rarely, death. In older adults, confusion or
changes in alertness may be the first sign of a UTI. Complications from long-term catheterization include catheter obstruction, bladder stones, local periurethral infection, chronic renal inflammation, chronic pyelonephritis, bladder cancer, renal failure, and the same complications as from short-term catheterization.
To reduce the incidence of UTIs and their complications in catheterized patients, wash your hands with water and a conventional antiseptic-containing soap or use an alcohol-based gel or foam before and after donning gloves to care for your patients catheter. Keep the catheter drainage system closed and remove the catheter as soon as possible.
Treating a UTI in a catheterized patient includes removing or replacing the catheter and administering an antibiotic based on urine culture results.
For asymptomatic bacteriuria (colonization of bacteria in the urine), antibiotics are indicated only if your patient is pregnant, has had a kidney transplant, or is about to have urinary tract surgery.
Hampering hospital patients
Outbreaks of nosocomial infection in hospitals often involve patients with UTIs. Some 40% of nosocomial infections are UTIs, and up to 80% of these are from urinary catheterization.
Factors that increase a hospital patients risk of developing a UTI include being female or older than age 60 or having severe underlying disease, fecal incontinence, or an indwelling urethral catheter. Manipulating the catheter during diagnostic or therapeutic procedures also encourages UTI development. You can help prevent UTIs in the hospital by consistently following hand hygiene recommendations and avoiding the use of urinary catheters.
Links to long-term care
Because of increased use of catheterization, decreased fluid intake, incontinence, and changes in personal hygiene, long-term-care residents are especially susceptible to UTIs. In this population, UTIs are the most common cause of infection. In elderly long-term-care residents, UTIs are the most common cause of bacteremia. You can help protect residents from UTIs with appropriate nursing interventions (see Preventing UTIs in Long-Term Care).
Catheter-related UTIs are the most common acquired infection in long-term-care residents. If a resident becomes confused, agitated, lethargic, incontinent, or has more falls, he may have a UTI; however, these nonspecific signs can indicate other conditions too, such as dehydration.
Antibiotic therapy should be initiated in a resident who doesn't have an indwelling catheter but has acute dysuria or a temperature greater than 100 deg F (37.9 deg C) and at least one of the following criteria:
* new or worsening urinary frequency or urgency, suprapubic pain, or incontinence
* new costovertebral-angle tenderness
* gross hematuria.
Antibiotic therapy should be initiated in a resident who has an indwelling catheter and at least one of the following criteria:
* temperature greater than 1000 F
* chills
* new costovertebral-angle tenderness
* new onset of delirium.
Antibiotics shouldn't be initiated in a resident simply because his urine is cloudy or smells foul. Someone with asymptomatic bacteriuria shouldn't receive antibiotics.
A urinalysis to measure bacteria levels, nitrites, white blood cells, and leukocyte esterase aren't reliable indicators of UTI in asymptomatic residents. One study found that 50% of women and 40% of men in long-term care had significant amounts of bacteria in their urine (colonization), but didn't have a UTI.
Choosing the right treatment
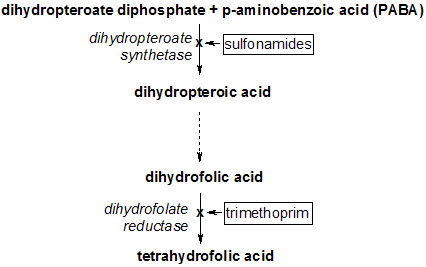
To treat a UTI, the health care provider will prescribe an antibiotic specific for the uropathogen identified by the urine culture. Until culture results are available, however, an antibiotic is chosen based on local susceptibility patterns. Common antibiotic choices for treating UTIs include trimethoprim/ sulfamethoxazole (Bactrim, Septra, Cotrim), nitrofurantoin (Macrodantin, Furadantin), amoxicillin, ampicillin, and fluoroquinolones. Nitrofurantoin shouldn't be used in patients with renal insufficiency, and ciprofloxacin should be used when resistant microorganisms are present. Duration of treatment depends on the microorganism, the patient's age and sex, and whether the infection is uncomplicated or complicated.
Teach your patient to take an active role in prevention by informing her of everyday choices that can help her and her family avoid these painful infections in the future (see Teaching Your Patients to Prevent UTIs).
The power of prevention
By following hand hygiene recommendations, knowing which patients are susceptible, and recognizing signs and symptoms, you can help patients avoid UTIs, regardless of your practice setting.
SELECTED REFERENCES
Dwyer, P: "Recurrent Urinary Tract Infection in the Female," Current Opinion in Obstetrics & Gynecology. 14(5):537-543, October 2002. Kaufman, J.: "Clinical Diagnosis of Urinary Tract Infection," JAMA. 288(10):1229-1230, September 2002.
Larcombe, J.: "Urinary Tract Infection," Clinical Evidence. 12(8):406-420, December 2002.
Nicolle, L.: "Urinary Tract Infections in Long-Term-Care Facilities," Infection Control and Hospital Epidemiology. 22(3):167-175, March 2001.
Ronald, A.: "The Etiology of Urinary Tract Infection: Traditional and Emerging Pathogens," Disease-A-Month. 49(2):71-82, February 2003.
Schaeffer, A.: "Short Compared with Standard Duration of Antibiotic Treatment for Urinary Tract Infection: A Systematic Review of Randomised Controlled Trials," The Journal of Urology. 169(4):1614-1615, April 2003.
BY JUDY C. ARBIQUE, ART(CSMLS), CLS(NCA)
Judy C. Arbique is a laboratory technologist in the division of microbiology, Queen Elizabeth II Health Sciences Centre, Halifax, Nova Scotia, Canada, and a partner in Arbique-Rendell Onsite Training and Consulting.
Copyright Springhouse Corporation Jun 2003
Provided by ProQuest Information and Learning Company. All rights Reserved