The enzymes of the transsulfuration pathway also have the capacity to catalyze the desulfhydration of cysteine. Recent studies demonstrate a role of the transsulfuration enzymes, cystathionine [gamma]-lyase and cystathionine [beta]-synthase, in catalyzing the desulfhydration of cysteine in brain and smooth muscle. The H^sub 2^S produced from cysteine functions as a neuromodulator and smooth muscle relaxant. In glutamatergic neurons, the production of H^sub 2^S by cystathionine [beta]-synthase enhances N-methyl-D-aspartate (NMDA) receptor-mediated currents. In smooth muscle cells, H^sub 2^S produced by cystathionine [gamma]-lyase enhances the outward flux of potassium by opening potassium channels, leading to hyperpolarization of membrane potential and smooth muscle relaxation.
Key words: brain, calmodulin, cysteine, cystathionine [gamma]-lyase, cystathionine [beta]-synthase
© 2004 International Life Sciences Institute
doi: 10.1301/nr.2004.sept.348-353
Introduction
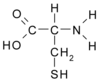
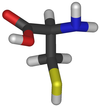
The nutritional essentiality of the sulfur amino acids is well established, and the current adult estimated average requirement (EAR) and recommended daily allowance (RDA) for methionine plus cysteine are approximately 15 mg kg^sup -1^ d^sup -1^ and 19 mg kg^sup -1^ d^sup -1^, respectively.1 The requirement for methionine is absolute, but cysteine can be synthesized via the unidirectional transsulfuration pathway that allows methionine to serve as the source of sulfur for cysteine synthesis. The enzymes that catalyze the transsulfuration pathway are cystathionine [beta]-synthase (CBS), which catalyzes the condensation of homocysteine with serine to form cystathionine, and cystathionine [gamma]-lyase (CGL), which catalyzes the [gamma]-cleavage of cystathionine to yield cysteine, [alpha]-ketobutyrate, and ammonia. While the roles of cysteine as a precursor for the synthesis of protein, glutathione, coenzyme A, taurine, and sulfate and the pathways for their production are well established, the role of cysteine as a precursor of reduced sulfur and the pathways for synthesis of reduced sulfur are only now being elucidated.
Since the 1950s, scientists have known that mammalian tissues contain enzymes capable of catalyzing the desulfhydration of cysteine. These enzymes include CBS, CGL, and possibly aminotransferases in conjunction with 3-mercaptopyruvate sulfurtransferase. Stipanuk and Beck2 attempted to assess the relative roles of these enzymes in cysteine desulfhydration in rat tissues, performing experiments both in vitro and in vivo, and concluded that both CBS and CGL catalyzed cysteine desulfhydration under physiologic conditions.
The enzymes involved in cysteine desulfhydration, CBS and CGL, are the same enzymes that catalyze the two steps in the methionine transsulfuration pathway. Both enzymes also accept cysteine as a substrate, but the reaction mechanisms for cysteine desulfhydration are somewhat unclear. CBS can catalyze a wide range of [alpha], [beta]-elimination/replacement reactions, which include the substitution of the thiol group of cysteine with a variety of thiol compounds to form H^sub 2^S and the corresponding thioether.3-5 It is thought that CGL catalyzes an [alpha],[beta]-disulfide elimination reaction that results in the production of pyruvate, ammonia, and thiocysteine. Thiocysteine may then react with cysteine or other thiols to form H^sub 2^S and cystine, or the corresponding disulfide. Thiocysteine may also decompose to elemental sulfur, which may then be reduced to H^sub 2^S, or more likely, the persulfide sulfur may be transferred to an acceptor such as sulfite.6-8 The affinity of these enzymes for cysteine is relatively low, and H^sub 2^S production increases with concentrations of up to >150 mM cysteine in assay systems.2 Thus, the amount of H^sub 2^S produced by these enzymes would be expected to increase with any increase in tissue cysteine concentration.
Although reduced sulfur may be used in the synthesis of molecules requiring a source of reduced sulfur, it has generally been assumed that the H^sub 2^S produced by these pathways would be readily oxidized to thiosulfate (inner sulfur), sulfite, and finally sulfate. The reactions involved in sulfide oxidation were elucidated by Koj et al.9 and Szczepkowski et al.10 in the 1960s.
This series of steps for sulfide oxidation to sulfate have been validated by subsequent studies demonstrating the GSH dependence of sulfate production, as well as thiosulfate accumulation by hepatocytes depleted of GSH with bromoheptane and/or buthionine sulfoximine and incubated with a high concentration of cysteine.11 About half of the cysteine catabolism in rat enterocytes or renal cortical tubules occurred via cysteinesulfinate-independent pathways, as evidenced by thiosulfate formation and inhibition by propargylglycine.12,13
Studies of cysteine desulfhydration in the 1970s and 1980s were followed by recognition that cysteine desulfhydration did not account for a quantitatively large proportion of cysteine catabolism in animals fed adequate levels of protein or sulfur amino acids.13-16 The major pathway for cysteine catabolism involves hepatic cysteine dioxygenase, which oxidizes the thiol group of cysteine to form cysteinesulfmate. Cysteinesulfinate is further oxidized, and cysteine sulfur is excreted as either taurine or sulfate. The K^sub m^ of cysteine dioxygenase is approximately 0.4 mM, which allows cysteine dioxygenase to respond to changes in cysteine concentrations within the physiologic range. Furthermore, cysteine dioxygenase concentration is robustly upregulated in response to increases in dietary protein or sulfur amino acid intake, effectively preventing accumulation of exess cysteine in the body but conserving it when intake is low.15,17 By ensuring that tissue cysteine concentrations remain below 1 µmol/g (usually below 0.1 µmol/g), cysteine dioxygenase limits the extent of H^sub 2^S production via cysteine desulfhydration.
Recently, another line of work has brought the focus back to cysteine desulfhydration pathways. Beginning in the mid-1990s, several studies demonstrated that H^sub 2^S has important physiologic functions and that its production is regulated. Furthermore, the role of CBS and CGL in regulated production of H^sub 2^S from cysteine in the nervous system and in smooth muscle tissues has been revealed.
Endogenous levels of H^sub 2^S are relatively high in brain, with 1.57 ± 0.04 µg/g (~0.3 nmol/mg protein) being measured in rat brain18 and 0.49 ± 0.07 nmol/mg protein in human frontal cortex.19 Several lines of evidence indicate that CBS is the enzyme responsible for H^sub 2^S production in brain. First, inhibitors or activators of CBS affected the production of H^sub 2^S from cysteine by whole brain preparations.20 Second, CBS activity, protein immunoreactivity, and mRNA levels were relatively high in various brain regions (hippocampus, cerebellum, cerebral cortex, and brain stem), whereas CGL activity and mRNA levels were low in cerebellum compared with other brain regions.21-23 Additionally, very low levels of H^sub 2^S in the brains of patients with Alzheimer's disease, compared with the brains of age-matched normal individuals, were accompanied by reduced CBS activity, an elevated level of Hcy, and a reduced level of S-adenosylmethionine (SAM), an activator of CBS.19
Physiologic concentrations of exogenously applied H^sub 2^S facilitate the induction of long-term potentiation (LTP) in rat hippocampal slices. Abe and Kimura20 showed that this enhancement of hippocampal LTP was the result of an enhancement of N-methyl-D-aspartate (NMDA) receptor-mediated currents in pyramidal cells of the CA1 layer. The mechanism underlying this phenomenon is poorly understood. The prevailing theory is that enhancement of NMDA currents arises as a secondary result of H^sub 2^S-induced alterations in intracellular cAMP metabolism (Figure 1). Indeed, Kimura24 demonstrated that sodium hydrosulfide (NaHS) increased cAMP concentrations in both primary neuronal cultures and some transformed neural cell lines.
An increase in cAMP levels in neurons could conceivably translate into alterations of NMDA channel conductance by means of protein kinase A (PKA) activation and the subsequent phosphorylation of conserved PKA consensus sites found on NMDA receptor subunits NMDARl, NMDAR2A, and NMDAR2B. Employing a Xenopus oocyte model that expresses NMDAR1 and NMDAR2A, Kimura24 showed that NaHS (10-30 µM) produced significant increases in intracellular cAMP and significant decreases in the onset of NMDA-induced membrane currents. The increase in cAMP and the reduction of activation latencies produced by NaHS could be prevented by an adenylyl cyclase-specific inhibitor.
Although these results suggest that changes in cAMP concentrations could be involved in the ability of H^sub 2^S to modulate NMDA activity, further examination of the hypothesis using neuronal cultures and a combination of adenylyl cyclase and PKA inhibitors needs to be conducted. Additional consideration should be given to the participation of astrocytes in the neuromodulatory properties of H^sub 2^S in situ. Accordingly, a recent study by Nagai et al.25 showed that NaHS alone induced robust, propagatable increases in the intracellular Ca^sup 2+^ levels of astrocytes from primary cultures and hippocampal slices. Co-cultured neurons, by contrast, showed no detectable change in intracellular Ca^sup 2+^ following exposure to NaHS. The exact mechanism by which NaHS altered intracellular Ca^sup 2+^ dynamics in astrocytes was not identified. It is worth noting, however, that NaHS was reported to increase the intracellular cAMP levels of transformed astroglia.25 Whether Ca^sup 2+^ channel phosphorylation by PKA is the cause of the dramatic changes in the Ca^sup 2+^ levels of astrocytes exposed to NaHS is not known.
The effects of physiologic levels of exogenously supplied H^sub 2^S on glutamatergic transmission through NMDA receptors in vitro have led to the suggestion that H^sub 2^S is an endogenous gaseous neuromodulator. However, definitive categorization of H^sub 2^S as an endogenous neuromodulator requires proof that control of its synthesis is coordinated with neuronal activity. Although there is no concrete evidence to indicate that this is the case, the localization of CBS expression within the soma and processes of many neurons hints at the possibility of neuronal activity-mediated regulation.23 Future studies remain to be conducted on the ability of glutamatergic-mediated changes in neuronal metabolic homeostasis, such as alterations in intracellular adenylate and calcium pools, to affect CBS activity.
Apart from its neuromodulatory properties, H^sub 2^S may also function as an endogenous smooth muscle relaxant in a wide array of vertebrates. Zhao and Wang26 reported that H^sub 2^S induced a concentration-dependent relaxation of rat aortic tissues. Teague et al.27 similarly demonstrated a dose-related relaxation of isolated rabbit ileum and rat vas deferens. Additionally, Sidhu et al.28 demonstrated that NaHS produced significant dose-dependent decreases in the spontaneous contractility of uterine strips from pregnant rats. Interestingly, the capacity for endogenous synthesis of H^sub 2^S in this tissue was hinted at by a reduction in spontaneous contractility following preincubation with 1 mM cysteine. Even in species of fresh and saltwater trout, H^sub 2^S was shown to elicit dose-dependent relaxation of isolated, pre-contracted branchial arteries.29 In vivo studies have supported the data gleaned from work done in vitro. Bolus intravenous injections of H^sub 2^S produced transient, 12.5 to 29.8 mm Hg drops in mean arterial blood pressure in rats with no corresponding change in heart rate-suggesting the exclusive involvement of arterial smooth muscle dilation.30 Given the blood levels of H^sub 2^S reported for different strains of rat (10-50 µM), H^sub 2^S may in fact be a tonic mediator of vasoactivity.30,31
The in situ generation of H^sub 2^S involved in peripheral smooth muscle relaxation appears to be catalyzed predominately by CGL. Inhibitors of CGL, but not of CBS, caused an increase in the contraction of guinea pig ileum in response to electrical stimulation.27 Hosoki et al.32 reported that CGL mRNA is expressed in the guinea pig ileum, portal vein, and thoracic aorta, and inhibitor studies suggested that the production of H^sub 2^S in portal vein and thoracic aorta was catalyzed by CGL, whereas in ileum it was catalyzed by both CGL and CBS-which was also shown to be transcribed in this tissue. In intact rats, expression of CGL and its corresponding enzyme activity in rat lung tissue were suppressed during hypoxic pulmonary hypertension, adding to evidence that H^sub 2^S production may be an important physiologic relaxor of smooth muscle.33
Within tissues that contain smooth muscle, it is not clear what cell types are contributing to the in situ synthesis of H^sub 2^S. To date, it has been shown that CGL is transcribed in vascular smooth muscle cells but not the endothelia of rat arteries.30 Pharmacologic investigations with CGL inhibitors and electrical field stimulation of guinea pig ileum, on the other hand, indirectly suggest that CGL may be expressed by intramural innervation within this tissue rather than smooth muscle cells.27 What bearing these differences in cell-specific expression may have on the larger physiologic function of H^sub 2^S-induced relaxation remains unclear. In fact, there is no clear picture of the extent to which H^sub 2^S contributes to smooth muscle tone under physiologic conditions. This deficit in understanding is due in part to how little is known about the regulatory mechanisms that govern H^sub 2^S generation in peripheral tissues.
The mechanism by which H^sub 2^S brings about smooth muscle relaxation is not fully understood. The most complete body of evidence comes from work based on vascular smooth muscle. According to the studies in this tissue, the effect of smooth muscle relaxation appears to be mediated in large part by the opening of potassium channels on the surface of smooth muscle cells (Figure 2). The first clear demonstration of the connection with potassium channels was reported by Zhao et al.30 through a series of in vivo and in vitro studies showing that H^sub 2^S induced relaxation of vascular smooth muscle via the opening of K+^sub ATP^ channels. Although K+^sub ATP^ channels appear to be the most important participant in H^sub 2^S-induced vasodilation, voltage-dependent Ca^sup 2+^ channels and Ca^sup 2+^-dependent K channels may also play a minor role in the development of this phenomenon. Support for the involvement of these channels stems from the attenuation of smooth muscle relaxation in aortic ring preparations when extracellular calcium is eliminated or when charybdotoxin/apamin is present.26
Additionally, H^sub 2^S-induced relaxation appears to be influenced by an ill-defined, endothelium-dependent component. Removal of the closely apposed endothelial lining from aortic rings decreased the sensitivity, but not the amplitude, of smooth muscle responsiveness to H^sub 2^S.26 Precisely how the endothelium modulates smooth muscle sensitivity to H^sub 2^S has yet to be elucidated. One possibility, however, is the release of a diffusible vasoactive factor such as NO. Although production of NO was not necessary for the action of H^sub 2^S, low concentrations of H^sub 2^S acted synergistically to greatly enhance NO-induced smooth muscle relaxation in the aorta.32 This synergistic interaction may be partially explained by the observation that H^sub 2^S production was enhanced by sodium nitroprusside, an NO donor. NO donors have been reported to increase CGL expression and activity in rat aorta and lung tissue.30
Although it is tempting to generalize the mechanisms delineated from vascular smooth muscle to other nonvascular tissues, one study suggests that not all smooth muscles rely upon changes in the conductance of potassium/calcium channels to effect relaxation in the presence of H^sub 2^S. In particular, the smooth muscle found in guinea pig ileum proved to be insensitive to the K+^sub ATP^ channel inhibitor glibenclamide and, moreover, was not affected by manipulations of extracellular K+ concentration.26 The potential diversity of novel mechanisms underlying H^sub 2^S-induced relaxation in smooth muscles outside the cardiovascular system is thus an area ripe for investigation.
These physiologic studies have provided a clear role of CBS and CGL in generating H^sub 2^S to act as a neuroamodulator and smooth muscle relaxant. That cysteine is the substrate for H^sub 2^S production by cysteinesulfinate-independent pathways may be one reason the body needs a robustly regulated non-desulfhydration pathway (i.e.,the cysteinesulfinate-dependent or cysteine dioxygenase pathway) for rapid removal of excess cysteine. If cysteine levels were elevated, H^sub 2^S production might occur at toxic, rather than physiologic levels.
1. Institute of Medicine, National Academies. Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids. Washington, DC: National Academies Press; 2002.
2. Stipanuk MH, Beck PW. Characterization of the enzymic capacity for cysteine desulphhydration in liver and kidney of the rat. Biochem J. 1982;206: 267-277.
3. Lac ND, Gorgachenkova EV, Braunstein AE. Investigation of substrate specificity of serine sulfhydrase from the hen liver and its relation to some inhibitors. Biokhimiya. 1970;35:270-277.
4. Braunstein AE, Goryachenkova EV, Lac ND. Reactions catalysed by serine sulfhydrase from chicken liver. Biochim Biophys Acta. 1971;171: 366-368.
5. Porter PN, Grishaver MS, Jones OW. Characterization of human cystathionine [beta]-synthase. Evidence for the identity of human L-serine dehydratase and cystathionine [beta]-syntahse. Biochim Biphys Acta. 1974;364:129-139.
6. Cavallini D, Mondovi B, DeMarco C, Scioscia-Santoro A. Inhibitory effect of mercaptoethanol and hypotaurine on the desulfhydration of cysteine by cystathionase. Arch Biochem Biophys. 1962;96: 456-457.
7. Cavallini D, Mondovi, B, DeMarco C, Scioscia-Santoro A. The mechanism of desulphydration of cysteine. Enzymologia. 1962;24:253-266.
8. Szczepkowski TW, Wood JL. The cystathionase-rhodanese system. Biochim Biphys Acta. 1967;139: 469-478.
9. Koj A, Frendo J, Janik Z. [^sup 35^S]Thiosulphate oxidation by rat liver mitochondria in the presence of glutathione. Biochem J. 1967; 103:791-795.
10. Szczepkowski TW, Skarzynski B, Weber M. The metabolic state of thiosulphate. Naturwissenschaften. 1961 ;189:1007-1008.
11. Huang J, Khan S, O'Brien PJ. The glutathione dependence of inorganic sulfate formation from L- or D-cysteine in isolated rat hepatocytes. Chem Biol Interact. 1998;110:189-202.
12. Coloso RM, Stipanuk MH. Metabolism of cyst(e)ine in rat enterocytes. J Nutr. 1989;119:1914-1924.
13. Stipanuk MH, De la Rosa J, Hirschberger LL. Catabolism of cyst(e)ine by rat renal cortical tubules. J Nutr. 1990;120:450-458.
14. Bella DL, Hahn C, Stipanuk MH. Effects of non-sulfur and sulfur amino acids on the regulation of hepatic enzymes of cysteine metabolism. Am J Physiol. 1999;277:E144-E153.
15. Stipanuk MH, Londono M, Lee JI, Hu M, Yu AF. Enzymes and metabolites of cysteine metabolism in nonhepatic tissues of rats show little response to changes in dietary protein or sulfur amino acid levels. J Nutr. 2002;132:3369-3378.
16. Stipanuk MH, Coloso RM, Garcia RA, Banks MF. Cysteine concentration regulates cysteine metabolism to glutathione, sulfate and taurine in rat hepatocytes. J Nutr. 1992;122:420-427.
17. Stipanuk MH, Hirschberger LL, Londono MP, Cresenzi CL, Yu AF. The ubiquitin-proteasome system is responsible for cysteine-responsive regulation of cysteine dioxygenase concentration in liver. Am J Physiol Endocrinol Metab. 2004;286: E439-E448.
18. Warenycia MW, Goodwin LR, Benishin CG, et al. Acute hydrogen suifide poisoning. Demonstration of selective uptake of suifide by the brainstem by measurement of brain suifide levels. Biochem Pharmacol. 1989;38:973-981.
19. Eto K, Asada T, Arima K, Makifuchi T, Kimura H. Brain hydrogen suifide is severely decreased in Alzheimer's disease. Biochem Biophys Res Commun. 2002;293:1485-1488.
20. Abe K, Kimura H. The possible role of hydrogen suifide as an endogenous neuromodulator. J Neurosci. 1996:16:1066-1071.
21. Awata S, Nakayama K, Suzuki I, Sugahara K, Kodama H. Changes in cystathionine [gamma]-lyase in various regions of rat brain during development. Biochem Mol Biol Int. 1995;35:1331-1338.
22. Kodama H, Ikeda H, Awata S, Nakayama K. Cystathionine accumulation in various regions of brain of DL-propargylglycine-treated rats. J Neurochem. 1985;44:1207-1209.
23. Robert K, Vialard F, Thiery E, et al. Expression of the cystathionine [beta] synthase (CBS) gene during mouse development and immunolocalization in adult brain. J Histochem Cytochem. 2003;51:363-371.
24. Kimura H. Hydrogen sulfide induces cyclic AMP and modulates the NMDA receptor. Biochem Biophys Res Commun. 2000;267:129-133.
25. Nagai Y, Tsugane M, Oka J, Kimura H. Hydrogen suifide induces calcium waves in astrocytes. FASEB J. 2004:18:557-559.
26. Zhao W, Wang R. H^sub 2^S-induced vasorelaxation and underlying cellular and molecular mechanisms. Am J Physiol Heart Circ Physiol. 2002;283:H474-H480.
27. Teague B, Asiedu S, Moore PK. The smooth muscle relaxant effect of hydrogen sulphide in vitro: evidence for a physiological role to control intestinal contactility. Br J Pharmacol. 2002;137:139-145.
28. Sidhu R, Singh M, Samir G, Carson RJ. L-Cysteine and sodium hydrosulphide inhibit spontaneous contractility in isolated pregnant rat uterine strips in vitro. Pharmacol Toxicol. 2001;88:198-203.
29. Dombkowski RA, Russell MJ, Olson KR. Hydrogen suifide as an endogenous regulator of vascular smooth muscle tone in trout. Am J Physiol Regul Comp Physiol. 2004;286:R678-R685.
30. Zhao W, Zhang J, Lu Y, Wang R. The vasorelaxant effect of H^sub 2^S as a novel endogenous gaseous K^sub ATP^ channel opener. EMBO J. 2001;20:6008-6016.
31. Mason J, Cardin CJ, Dennehy A. The role of sulphide and sulphide oxidation in the copper molybdenum antagonism in rats and guinea pigs. Res Vet Sci. 1978;24:104-108.
32. Hosoki R, Matsuki N, Kimura H. The possible role of hydrogen sulfide as an endogenous muscle relaxant in synergy with nitric oxide. Biochem Biophys Res Commun. 1997;237:528-531.
33. Chunyu Z, Janbao D, Dingfang B, Hui Y, Xiuying T, Chaoshu T. The regulatory effect of hydrogen sulfide on hypoxic pulmonary hypertension in rats. Biochem Biophys Res Commun. 2003;302: 810-816.
John E. Dominy, B.S., and Martha H. Stipanuk, Ph.D.
Dominy and Stipanuk are with Division of Nutritional Sciences, Cornell University, Ithaca, NY, 14853, USA.
Copyright International Life Sciences Institute and Nutrition Foundation Sep 2004
Provided by ProQuest Information and Learning Company. All rights Reserved