This report describes a case of acute myeloid leukemia (subtype M1) with biphasic morphology. The bone marrow biopsy showed 2 distinct regions of blasts, one containing large cells and the other small cells. Morphometric and DNA ploidy analysis showed that the mean nuclear area and mean DNA index for the large cell region were 2-fold higher than those for the small cell region. Cytogenetic analysis showed an abnormal near-tetraploid clone. The tumor relapsed following aggressive therapy. The cells from the relapse specimen were similar to the original small cell region with respect to nuclear area and DNA index; however, there was immunophenotypic transformation with gain of CD7 and gain of CD56. Cytogenetically, the relapse specimen showed no evidence of the near-tetraploid clone, but instead had a previously unidentified abnormal clone containing 46 chromosomes and structural abnormalities of 2q and 7q. Biphasic morphology in acute myeloid leukemia may be predictive of a near-tetraploid subclone and immunophenotypic transformation.
(Arch Pathol Lab Med. 2004;128:448-451)
Acute myeloid leukemia (AML) is usually characterized by a monomorphic infiltrate of blasts on histologic sections.1 To our knowledge, a biphasic growth pattern with 2 distinct cell populations of different sizes has not been reported in AML.
We report a case of AML with biphasic morphology characterized by the presence of 2 separate regions of blasts, one comprised of large cells and the other of small cells. The neoplasm was refractory to aggressive therapy, and the relapsed tumor resembled the original small blast component histologically. This report describes the morphologic, morphometric, DNA ploidy, immunophenotypic, and cytogenetic analyses of the tumor at presentation and relapse.
REPORT OF A CASE
A 44-year-old man presented with a several-week history of worsening sore throat, low-grade fever, and dyspnea at rest. Physical examination showed plethora and left cervical lymphadenopathy. Laboratory studies showed pancytopenia, with a hemoglobin level of 4.7 g/dL (2.9 mmol/L); white blood cell count, 1200/µL (1.2 × 10^sup 9^L); and platelets, 39 × 10^sup 3^/µL (39 × 10^sup 9^/L). The blood smear showed 43% blasts. Bone marrow aspiration and biopsy were performed. This patient was diagnosed with AML subtype Ml based on World Health Organization classification criteria.1
The patient was treated with standard induction chemotherapy (3 + 7; daunorubicin + cytarabine) followed by consolidation chemotherapy. The bone marrow went into morphologic remission. He was treated 10 months later with autologous peripheral blood stem cell transplantation. The patient had a bone marrow relapse 2 months later, which was treated with allogeneic peripheral blood stem cell transplantation (sibling donor) and resulted in marrow remission. He developed a second marrow relapse 6 months later and did not receive further therapy. The patient eventually died of pneumonia 18 months after initial presentation.
PATHOLOGIC FINDINGS
Neoplasm at Presentation
Morphologic Analysis.-The Wright-stained bone marrow aspirate smears showed 90% blasts, characterized by a polymorphous mixture of small to large cells with regular nuclear contour, finely dispersed cnromatin, 1 to 2 prominent nucleoli, and moderate amounts of pale blue cytoplasm without vacuolation. Cytochemical stains showed the blasts were moderately positive for Sudan black B, weakly positive for chloroacetate esterase, negative for a-naphthyl acetate esterase, and negative for periodic acid-Schiff.
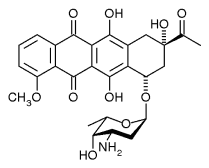
The hematoxylin-eosin-stained bone marrow biopsy showed a hypercellular marrow (90%) with 2 distinct regions of blasts (Figure). The first region was composed of a diffuse infiltrate of large cells. The second region was adjacent to the first region and was composed of a diffuse infiltrate of small cells.
Morphometric and DNA Ploidy Analysis.-Morphometric analysis of nuclear area and DNA ploidy analysis were performed on Feulgen-stained bone marrow biopsy sections using a CAS 200D Image Analysis System equipped with version 3.0 of the Quantitative DNA Analysis software program (originally Cell Analysis Systems, Inc, a Division of Becton Dickinson, Inc, Elmhurst, Ill; service support now supplied by Bacus Laboratories, Inc, Lombard, Ill). The outer nuclear contour of each cell selected for analysis was delineated using a mouse-controlled pointer. The instrument automatically calculated the nuclear area and DNA index for each cell. One hundred random cells were evaluated in the large cell region and small cell region.
The results are summarized in the Table. The mean nuclear area of the large cell region was 2-fold higher than that of the small cell region. The DNA ploidy analysis showed a mean DNA index that was also approximately 2-fold higher in the large cell region, consistent with the morphometric analysis. The large cell region was dominated by tetraploid cells (DNA index = 1.81-2.20) and aneuploid cells (DNA index > 2.20), whereas the small cell region was dominated by diploid cells (DNA index = 0.90-1.10) and S-phase cells (DNA index = 1.11-1.80).
Immunophenotypic Analysis.-Two-color flow cytometry was performed on the marrow aspirate using a Cytoron Absolute analyzer (Ortho Diagnostics Systems, Raritan, NJ). Antibodies to CD2, CD3, CD4, CD7, CD8, CD10, CD11b, CD13, CD14 (Mo2), CD14 (My4), CD20, CD33, CD34, CD45, CD56, and HLA-DR were obtained from Coulter Corporation (Miami, Fla). Antibodies to CDS and CD19 were obtained from Caltage Laboratories (Burlingame, Calif). Antibody to CD41 was obtained from GenTrak, Inc (Plymouth Meeting, Pa). Antibody to CD235a was obtained from Dako Corporation (Carpinteria, Calif). Blasts were gated based on light-scattering characteristics (forward vs side scatter). The blasts were positive for dim CD45, CD13, CD33, CD34, and HLA-DR. The blasts were negative for CD2, CD3, CD4, CD5, CD7, CD8, CD10, CD11b, CD14 (Mo2), CD14 (My4), CD19, CD20, CD41, CD56, and CD235a (glycophorin A).
Cytogenetic Analysis.-Cytogenetic analysis was performed on the marrow aspirate using standard G-banding technique. Eight of 20 metaphases were near-tetraploid (92-94 chromosomes) with multiple numerical and structural chromosome abnormalities, including del(6)(q23) and several unidentifiable marker chromosomes. The remaining 12 metaphases were 46,XY.
Fluorescence in situ hybridization on the bone marrow aspirate using a DNA probe against 7q31 showed an interstitial deletion of the long arm of chromosome 7 in 17% of the interphase nuclei.
Neoplasm at Relapse
Morphologic Analysis.-The bone marrow was reevaluated at the second relapse by morphology, morphometry, DNA ploidy, flow cytometry, and cytogenetics. The marrow aspirate showed 26% blasts. The hematoxylin-eosinstained bone marrow biopsy showed a hypocellular marrow (10%-20%) with focal areas of monomorphic blasts infiltrating in an interstitial pattern. The blasts appeared similar in size to the small cell component noted on the original neoplasm.
Morphometric and DNA Ploidy Analysis.-One hundred blasts were randomly selected for analysis on a Feulgen-stained biopsy section. The results are summarized in the Table. The mean nuclear area and mean DNA index were more similar to the small cell region than the large cell region of the original neoplasm. The relapsed tumor did show some differences from the small cell region, however, including increased diploid cells, decreased S-phase cells, and slightly increased aneuploid cells.
Immunophenotypic Analysis.-Flow cytometric studies were performed using the same panel of antibodies used on the neoplasm at first presentation. The blasts were positive for the same markers as noted on the original neoplasm; however, there was gain of CD7 and CD56. Coexpression of CD7 and CD56 on the CD34-positive blasts was confirmed by 2-color analysis.
Cytogenetic Analysis.-All 20 metaphases analyzed had 46 chromosomes. Six of the 20 metaphases had del(7)(q22) and add(2)(q32). The near-tetraploid clone noted on the original neoplasm was not detected.
COMMENT
To our knowledge, this is the first reported case of AML with biphasic morphology on bone marrow biopsy. The biphasic growth pattern was characterized morphologically by a distinct large cell region whose cells had twice the nuclear area of the small cell region, as determined by morphometric analysis. DNA ploidy analysis on Feulgenstained sections indicated that the large cell region was composed of predominantly tetraploid and aneuploid cells. The cytogenetic finding of a near-tetraploid clone further supported these results.
Near-tetraploidy is a rare cytogenetic abnormality in AML and is reported in 0.7% of cases.2 This abnormality is more frequent in males, occurs in a variety of AML subtypes (M0, M1, M2, M4, M5, and M6), and is of uncertain prognostic significance. The most consistent morphologic association with near-tetraploidy is the presence of both large blasts and smaller blasts on bone marrow aspirate smears and biopsy sections.2,3 Previous reports do not describe in detail the histopathology of the biopsy infiltrate. For example, it is unclear whether the large blasts are intermingled with the small blasts, or whether the large blast component is distinctly separate from the small blast component, as reported here. A systematic study of the biopsy material from tetraploid and near-tetraploid AML will be required to determine the range of specific growth patterns.
Tetraploid and near-tetraploid AML has been associated with t(8;21) and double 8;21 translocations involving rearrangement of the AML1 and ETO genes.4-6 This observation suggests that the tetraploid clone could arise by secondary evolution from a diploid t(8;21) clone. Although the present case did not contain a t(8;21) clone by routine cytogenetic analysis, we cannot exclude the possibility of a molecular rearrangement, since dual-color fluorescence in situ hybridization analysis for the AML1 and ETO genes was not performed owing to an insufficient amount of sample.
It is interesting to speculate on the role of the neartetraploid AML clone in the carcinogenic mechanism of this neoplasm. One possibility is that it could represent an unstable secondary clone that was part of the evolution to a more stable neoplastic phenotype. In Barrett esophagus, for example, tetraploid clones appear to be transient intermediates in the pathway leading to esophageal carcinoma.7 These intermediate clones contain a large set of up-regulated genes, many of which function in the G^sub 2^-M phase of the cell cycle to mediate processes such as chromosome condensation and segregation.
This neoplasm demonstrated immunophenotypic transformation at relapse, with gain of CD7 and CD56 on the diploid small cell component. This is the first reported case of AML subtype Ml with gain of these 2 cell surface proteins at relapse. The CD7 gene is located at 17q25 and is normally expressed on T cells, natural killer cells, precursor B cells, and precursor myeloid cells.8,9 The CD56 gene is located at 11q23 and is normally expressed on natural killer cells and a subset of activated T cells.10,11 The mechanism of dysregulated expression of CD7 and CD56 in this case is uncertain. We found no conventional cytogenetic evidence to suggest gross mutations involving their genes at chromosomes 17 and 11. De novo AML with CD7 and CD56 expression is thought to represent a distinct clinicopathologic entity that is associated with poor prognosis.12 Consequently, gain of these 2 markers at relapse may have been a poor prognostic feature in this case.
At presentation, the tumor showed a complex karyotype (>3 abnormalities) plus an interstitial deletion of 7q, putting this patient in an unfavorable prognostic group.11 In addition, the relapsed tumor acquired a cytogenetically abnormal clone containing both del(7)(q22) and add(2)(q32). The failure of aggressive postremission therapy consisting of autologous and allogeneic peripheral blood stem cell transplantation is consistent with these complex and unfavorable cytogenetic features.
In summary, this report demonstrates that AML can exhibit biphasic morphology. Further study will be required to define the frequency and clinical significance of this histopathologic feature in AML with near-tetraploidy or tetraploidy.
References
1. Brunning RD, Matutes E, Flandrin G, et al. Acute myeloid leukaemia not otherwise categorised. In: Jaffe ES, Harris NL, Stein H, Vardiman JW, eds. Pathology and Genetics of Tumours of Haematopoietic and Lymphoid Tissues. Lyon, France: IARC Press; 2001:91-105. World Health Organization Classification of Tumours; vol 3.
2. Clarke MR, Lynch EF, Contis LC, et al. Near-tetraploidy in adult acute myelogenous leukemia. Cancer Cenet Cytogenet. 1996;86:107-115.
3. Espinet B, Sole F, Woessner S, et al. Two new cases of near-tetraploidy in adult acute myeloid leukemia. Cancer Genet Cytogenet. 1998;102:131-134.
4. Xue Y, Pan Y, Liu Z, et al. Tetraploid or near-tetraploid clones characterized by two 8;21 translocations and other chromosomal abnormalities in two patients with acute myeloblastic leukemia. Cancer Genet Cytogenet. 1996;92:18-23.
5. Xue Y, He J, Wang Y, et al. Secondary near-pentaploidy and/or near-tetraploidy characterized by the duplication of 8;21 translocation in the M2 subtype of acute myeloid leukemia, Int J Hematol. 2000;71:359-365.
6. Yamamoto K, Nagata K, Kida A, et al. CD7 + near-tetraploid acute myeloblastic leukemia M2 with double t(8;21)(q22;q22) translocations and AML1/ETO rearrangements detected by fluorescence in situ hybridization analysis, Int J Hematol. 2001;74:316-321.
7. Barrett MT, Pritchard D, Palanca-Wessels C, et al. Molecular phenotype of spontaneously arising 4N (G2-tetraploid) intermediates of neoplastic progression in Barren's esophagus. Cancer Res. 2003;63:4211-4217.
8. Baker E, Sandrin MS, Garson OM, et al. Localization of the cell surface antigen CD7 by chromosomal in situ hybridization, Immunogenetics. 1990;31: 412-413.
9. Sempowski GD, Lee DM, Kaufman RE, et al. Structure and function of the CD7 molecule. Crit Rev Immunol. 1999;19:331-348.
10. Nguyen C, Mattei MG, Goridis JF, et al. Localization of the human N-CAM gene to band q23 of chromosome 11: the third gene coding for a cell interaction molecule mapped to the distal portion of the long arm of chromosome 11. J Cell Biol. 1986;102:711-715.
11. Lanier LL, Le AM, Civin Cl, et al. The relationship of CD16 (Leu-11) and Leu-19 (NKH-1) antigen expression of human peripheral blood NK cells and cytotoxic T lymphocytes. J Immunol. 1986;136:4480-4486.
12. Suzuki R, Yamamoto K, Seto M, et al. CD7+ and CD56+ myeloid/natural killer cell precursor acute leukemia: a distinct hematolymphoid entity. Blood. 1997;90:2417-2428.
13. Slovak ML, Kopecky KJ, Cassileth PA, et al. Karyotypic analysis predicts outcome of preremission and postremission therapy in adult acute myeloid leukemia: a Southwest Oncology Group/Eastern Cooperative Oncology Group study. Blood. 2000;96:4075-4083.
Marwa Imkie, MD; Marilyn K. Davis; Diane L. Persons, MD; Mark T. Cunningham, MD
Accepted for publication November 17, 2003.
From the Department of Pathology, University of Kansas Medical Center, Kansas City, Kan.
The authors have no relevant financial interest in the products or companies described in this article.
Reprints: Mark T. Cunningham, MD, Department of Pathology, University of Kansas Medical Center, Mail Stop 3045, 3901 Rainbow Blvd, Kansas City, KS 66223 (e-mail: mcunningham@kumc.edu).
Copyright College of American Pathologists Apr 2004
Provided by ProQuest Information and Learning Company. All rights Reserved