ABSTRACT. Background: The inhibitory influence of exogenous dextrose on glucose production has been shown to be less pronounced during injury and sepsis. This protocol was designed to investigate the effect of IV hypocaloric dextrose on glucose metabolism during elective abdominal surgery. Methods: Fourteen patients with rectal cancer were studied under fasting conditions and toward the end of a 3-hour infusion of dextrose (2 mg-kg ^sup -1^ per minute) either in absence (control group, n = 7) or presence of colonic surgery (surgery group, n = 7). Endogenous glucose production was determined by using primed continuous infusions of [6,62H^sub 2^] glucose before and during dextrose administration. We also measured the plasma concentrations of glucose, lactate, cortisol, glucagon, and insulin. Results: The administration of dextrose decreased the endogenous glucose production in all patients (p
The major objective of IV dextrose administration in surgical patients is to attenuate the loss of functional and structural proteins, a typical feature of the catabolic response to abdominal surgery.1 The proteinsparing action of dextrose partly stems from the suppression of gluconeogenesis and, thus, a reduced need for amino acids, which become the quantitatively most important gluconeogenic precursors under perioperative conditions.2 The impact of dextrose infusions on endogenous glucose production has been assessed in healthy subjects,3 during the reconvalescence after abdominal operations,4 after injury,5 and during pancreatitis6 and sepsis.7 Although it is widely held that the inhibitory influence of exogenous dextrose on glucose production is less pronounced during periods of stress, its effect during the acute phase of elective surgical tissue trauma has not been studied so far. The present protocol was designed to investigate the effect of IV dextrose administered at a rate of 2 mg.kg^sup -1^.min^sup -1^ on glucose metabolism during abdominal surgery. Glucose production was assessed by the stable isotope tracer [6,6-2H^sub 2^]glucose.
MATERIALS AND METHODS
Patients
The study was approved by the local ethics committee and conducted in accordance with the guidelines of Helsinki. Informed consent was obtained from 14 patients scheduled for elective low anterior colonie resection for nonmetastasized rectal cancer. No patient was suffering from cardiac, hepatic, renal, or metabolic disorders or receiving any medication known to affect metabolism. None of the participants had developed >5% weight loss over the preceding 3 months, had a hemoglobin
Study Protocol
Consenting patients who were scheduled for surgery at 8:00 AM were assigned to the surgery group, whereas patients undergoing surgery after 11:00 AM formed the control group. Baseline measurements were performed on the day of surgery between 6:00 AM and 8:00 AM. Dextrose (beet dextroae 10% in 0.45% normal saline; Avebe, Foxhol, Holland) was administered over 3 hours (8:00 AM to 11:00 AM) either in absence (control group) or presence of surgery (surgery group). The dextrose solution was prepared by the local pharmacy and was tested for sterility, stability, and absence of pyrogens. Dextrose was infused at 2 mg-kg^sup -1^ per minute because intraoperative plasma glucose concentrations during the administration of glucose at a greater rate regularly exceed 10 mmol/L, the physiologic threshold for renal glucose excretion.^sup 8-10^
Anesthesia Care
In the surgery group, general anesthesia was induced with 5 mg/kg thiopentone and 5 µg/kg fentanyl. Endotracheal intubation was facilitated with 0.6 mg/kg rocuronium, and patients' lungs were ventilated with 30% oxygen in air to maintain normocapnia. General anesthesia was maintained using desflurane at end-tidal concentrations as required to keep heart rate within 20% of preoperative values. The pure [alpha]-agonist phenylephrine was used for hemodynamic support. Normal saline 0.9% was infused at a rate of 6 mL kg^sup -1^ per hour during the operation. Blood losses were replaced by normal saline in a ratio of 3:1. Patients in the control group received the same amount of normal saline during the infusion of dextrose. Supplemental doses of rocuronium were applied as needed for complete surgical muscle relaxation. All patients were covered with a warming blanket to maintain normothermia.
Measurements
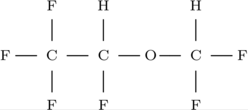
Plasma kinetics of glucose were determined by a stable isotope tracer technique using primed continuous infusions of [6,6-2H^sub 2^glucose (Cambridge Isotope Laboratories, Cambridge, MA). Sterile solutions of the isotope were prepared by the local pharmacy and kept at 4°C until administration. A catheter was placed in a superficial vein in the dorsum of the hand and kept patent with a slow saline 0.9% infusion. A superficial vein of the contralateral arm was cannulated to provide access for the infusion of [6,6-2H^sub 2^]glucose. Blood samples were taken to determine baseline enrichments. At 6:00 AM, a priming dose of [6,6-2H^sub 2^]glucose 22 µ/kg was administered, followed immediately by the infusion of [6,6-2H^sub 2^]glucose at 0.22 µmol-kg^sup -1^ per minute over 5 hours. Isotope infusions were uninterrupted throughout the entire study period. Blood samples for the determination of isotopic plasma enrichments were taken at 150 minutes, 160 minutes, 170 minutes, and 180 minutes of [6,6-2H^sub 2^]glucose infusion. A second set of samples was taken during dextrose administration at 270 minutes, 280 minutes, 290 minutes, and 300 minutes of the isotope infusion. In the surgery group, this was equivalent to 90 minutes, 100 minutes, 110 minutes, and 120 minutes into the operation. Blood samples were drawn for the measurement of metabolic substrates (glucose, lactate) and hormones (insulin, glucagon, cortisol) after 180 minutes, 270 minutes, and 300 minutes of [6,6-2H^sub 2^]glucose infusion. Each blood sample was immediately transferred to a heparinized tube and centrifuged at 4°C (3000 X g, 15 minutes). The plasma obtained was stored at -70°C until analysis.
Analytical Methods
Plasma [6,6-2H^sub 2^]glucose enrichment was analyzed by electron-impact selected-ion monitoring gas chromatography-mass spectrometry.11 Plasma glucose concentrations were measured with a glucose analyzer 2 (Beckman Instruments, Fullerton, CA) using the glucose oxidase method. The plasma lactate assay was based on lactate oxidase using the synchron CX 7 system (Beckman Instruments). Cortisol, insulin, and glucagon plasma concentrations were measured by a double antibody radioimmunoassay (Amersham International, Amersham, Bucks, UK).
Calculations
Under steady-state conditions, the rate of appearance (R^sub a^ of unlabeled substrate in plasma can be derived from the plasma enrichment (atom percent excess = APE) calculated by R^sub a^ = I X (APE^sub inf^/APE^sub pl ^ 1), where APE^sub inf^ is the tracer enrichment in the infusate, APE^sub pl^ is the tracer enrichment in plasma at steady state, and I is the infusion rate of the labeled tracer. The APE values used in this calculation represent the mean of the four APE values determined during each isotopic plateau. Steady-state conditions were assumed when the coefficient of variation of the APE values at isotopic plateau was
The plasma clearance of glucose, an indirect measure of whole-body glucose uptake, was calculated as the R^sub a^ glucose divided by the actual plasma glucose concentration.
For metabolic substrates and hormones, the average of the 2 measurements at 270 and 300 minutes of isotope infusion was calculated.
Statistics
Differences between the groups were analyzed using the Mann-Whitney U test. Within-group comparison of variables was made by the t test. A probability of p
RESULTS
There were no differences between the 2 groups regarding age, height, weight, and gender (Table I). Patients in the surgery group received a total of 1902 ± 215 mL normal saline, whereas patients in the control group received 1650 ± 80 mL. Isotopic plateau of [6,62H^sub 2^] glucose was achieved before and during the dextrose infusion, allowing steady-state calculations (Fig. 1). The administration of dextrose decreased the endogenous glucose production in all patients (Table II; p
DISCUSSION
The results of the present study indicate that the inhibitory effect of dextrose on endogenous glucose production is attenuated in patients undergoing colorectal surgery for cancer. Dextrose infusion at 2 mg-kg^sup -1^ per minute was associated with a 60% suppression of the R^sub a^ glucose during surgery, whereas it diminished the R^sub a^ glucose by 90% in a control group of patients studied under similar metabolic circumstances in the absence of surgery. Our findings are in line with the results of previous studies suggesting that during periods of physical stress, glucose production is to some extent resistant to the inhibitory action of exogenous dextrose. Administration of 4 mg-kg^sup -1^ per minute dextrose over 2 hours in patients with trauma,5 sepsis,7 or pancreatitis6 reduced glucose production by 50% only. In contrast, dextrose infused over 3 days at a rate of 4 mg-kg^sup -1^ per minute (together with amino acids) completely suppressed endogenous glucose production 6 days after different types of surgery.3
Much of the catabolic responses to surgery have been ascribed to alterations in the endocrine milieu, in particular to the elevated plasma concentrations of the counterregulatory hormones cortisol, glucagon, epinephrine, and norepinephrine, all of which promote hyperglycemia by stimulating glucose production and decreasing peripheral glucose use.12 Although plasma catecholamines were not determined in this protocol and glucagon plasma levels remained unchanged, cortisol plasma concentrations significantly increased during surgery. With respect to the well-known catabolic influence of cortisol on glucose metabolism and its counteracting effect on insulin,13 this may partly be responsible for the limited effectiveness of dextrose to inhibit glucose production intraoperatively.
Because of preoperative bowel preparation, the fasting time before abdominal procedures is usually long enough to substantially deplete hepatic glycogen stores.14 Hence, we assume that gluconeogenesis accounted for >90% of total glucose production as assessed by [6,6-^sup 2^H^sub 2^]glucose kinetics in our patients.15 Because muscle protein is broken down to supply amino acids as precursors for de novo glucose synthesis, it has been hypothesized that any suppression of gluconeogenesis may lead to a decrease in whole body protein breakdown.2 This assumption is supported by recent studies demonstrating a positive correlation between glucose production and protein breakdown in surgical patients.16,17 Our demonstration that dextrose at 2 mg.kg^sup -1^ per minute fails to substantially decrease glucose production during surgery may explain the fact that administration of hypocaloric dextrose fails to prevent the protein losses after major surgery.18-20
It has long been recognized that the type of anesthesia and analgesia significantly affects glucose homeostasis during surgery.21 For example, the attenuation of the hyperglycemic response to surgery by epidural blockade of efferent and afferent fibers at the spinal level was mediated through its inhibitory action on endogenous glucose production.22,23 A remifentanil-based IV anesthetic also decreased the R^sub a^ glucose during abdominal procedures.17 Although the present study design did not allow to separate the effects of surgery and anesthesia from the effects of dextrose infusion, we are confident that the type of anesthesia as used in the present protocol did not have a specific effect on glucose metabolism. This assumption is based on the results of a recent study conducted in a similar patient population and using the same anesthetic regimen, which show no significant change in glucose production during colorectal surgery.22
In summary, we have shown that surgical stress blunts the inhibitory effect of IV dextrose on endogenous glucose production. Despite the fact that only hypocaloric amounts of dextrose were used in our patients, intraoperative plasma glucose concentrations increased to a mean value of almost 10 mmol/L. Considering the clinical consequences of acute hyperglycemia, including immunosuppression,24,25 electrolyte imbalances,26 increased CO2 production,27 stimulated sympathoadrenergic activity,28 and increased mortality,29,30 it remains questionable if surgical patients benefit from intraoperative dextrose administration.
ACKNOWLEDGMENTS
The study was supported by a grant from the Research Institute of the Royal Victoria Hospital (to Dr Schricker).
REFERENCES
1. Wilmore D. Postoperative protein sparing. World J Surg. 1999; 23:545-552.
2. Wolfe RR. Carbohydrate metabolism and requirements. In: Rombeau JL, Caldwell MD, eds. Clinical Nutrition: Parenteral Nutrition. Philadelphia, Pa: Saunders; 1993:113-132.
3. Wolfe RR, Allsop JR, Burke JF. Glucose metabolism in man: Responses to intravenous glucose infusion. Metabolism. 1979;28: 210-220.
4. Wolfe RR, O'Donnell TF, Stone MD, Richmand DA, Burke JF. Investigation of factors determining the optimal glucose infusion rate in total parenteral nutrition. Metabolism. 1980;29:892-900.
5. Shaw JH, Wolfe RR. An integrated analysis of glucose, fat, and protein metabolism in severely traumatized patients. Ann Surg. 1989;209:63-72.
6. Shaw JH, Wolfe RR. Glucose, fatty acid, and urea kinetics in patients with severe pancreatitis: The response to substrate infusion and total parenteral nutrition. Ann Surg. 1986;204:665-672.
7. Shaw JH, Wolfe RR. Determinations of glucose turnover and oxidation in normal volunteers and septic patients using stable and radio-isotopes: The response to glucose infusion and total parenteral feeding. Aust N Z J Surg. 1986;56:785-791.
8. Sieber FE, Smith DS, Kupferberg J, et al. The effects of intraoperative glucose on protein catabolism and plasma glucose levels in patients with supratentorial tumors. Anesthesiology. 1986; 64:453-459.
9. Obata K, Ogata M, Matsumoto T, Takenaka I, Sata T, Shigematsu A. The effects of glucose on plasma amino acids and pyruvate during upper abdominal surgery. Anesth Analg. 1993; 76:357-361.
10. Sieber F, Smith D, Kupferberg J, et al. The effects of intraoperative glucose on protein catabolism and plasma glucose levels in patients with supratentorial tumors. Anesthesiology. 1989;64: 453-459.
11. Schricker T, Wykes L, Eberhart L, Lattermann R, Mazza L, Carli F. The anabolic effect of epidural blockade requires energy and substrate supply. Anesthesiology. 2002;97:943-951.
12. Weissman C. The metabolic response to stress: An overview and update. Anesthesiology. 1990;73:308-327.
13. Baron AD, Wallace P, Brechtel G. In-vivo regulation of noninsulin mediated and insulin mediated glucose uptake by cortisol. Diabetes. 1987;36:1230-1237.
14. Chandramouli V, Ekberg K, Schumann W, Kalhan SC, Wahren J, Landau BR. Quantifying gluconeogenesis during fasting. Am J Physiol. 1997;273:E1209-E1215.
15. Gump FE, Long CL, Geiger JW, Kinney JM. The significance of altered gluconeogenesis in surgical catabolism. J Trauma. 1975; 15:704-713.
16. Schricker T, Wykes L, Carli F. Epidural blockade improves substrate utilization after surgery. Am J Physiol. 2000;279:E646-E653.
17. Schricker T, Lattermann R, Fiset P, Wykes L, Carli F. Integrated analysis of protein and glucose metabolism during surgery: Effects of anesthesia. J Appl Physiol. 2001;91:2523-2530.
18. Greenberg G, Marliss E, Anderson H, et al. Protein sparing therapy in postoperative patients: Effects of added hypocaloric glucose or lipids. N Engl J Med. 1976;294:1411-1416.
19. Askanazi J, Carpentier Y, Jeevanandam M, Michelsen C, Elwyn D, Kinney J. Energy expenditure, nitrogen balance, and norepinephrine excretion after injury. Surgery. 1981;89:478-484.
20. Nordenstrom J, Askanazi J, Elwyn D, et al. Nitrogen balance during total parenteral nutrition. Ann Surg. 1983;197:27-33.
21. Schricker T, Lattermann R, Schreiber M, Geisser W, Georgieff M, Radermacher P. The hyperglycaemic response to surgery: Pathophysiology, clinical implications and modification by the anaesthetic technique. Clin Intensive Care. 1998;9:118-128.
22. Lattermann R, Wykes L, Carli F, Schricker T. Epidural blockade modifies perioperative glucose production without affecting protein catabolism. Anesthesiology. 2002;97:374-381.
23. Lattermann R, Schricker T, Wachter U, Georgieff M, Goertz A. Understanding the mechanisms by which isoflurane modifies the hyperglycemic response to surgery. Anesth Analg. 2001;93:121-127.
24. Kwoun MO, Ling PR, Lydon E, et al. Immunologic effects of acute hyperglycemia in nondiabetic rats. JPEN. 1997;21:91-95.
25. Pomposelli J, Baxter J, Babineau T, et al. Early postoperative glucose control predicts nosocomial infection rate in diabetic patients. JPEN. 1998;22:77-81.
26. Brenner W, Lansky Z, Engelman R, Stahl W. Hyperosmolar coma in surgical patients. Ann Surg. 1973;178:651-654.
27. Askanazi J, Rosenbaum S, Hyman A, Silverberg P, Milic-Emili J, Kinney J. Respiratory changes induced by the large glucose loads to total parenteral nutrition. JAMA. 1980;243:1444-1447.
28. Nordenstrom J, Jeevanandam M, Elwyn DH, Carpentier YA. Increasing glucose intake during total parenteral nutrition increases norepinephrine excretion in trauma and sepsis. Clin Physiol. 1981;1:525-534.
29. Rady MY, Ryan T, Starr NJ. Perioperative determinants of morbidity and mortality in elderly patients undergoing cardiac surgery. Crit Care Med. 1998;26:225-235.
30. Van den Berghe G, Wouters P, Weekers F, et al. Intensive insulin therapy in critically ill patients. N Engl J Med. 2001;345: 1359-1367.
Thomas Schricker, MD, PhD*; Ralph Lattermann, MD, MSc[dagger]; Linda Wykes, PhD*; and Franco Carli, MD, MPhil*
From the *Department of Anesthesia, McGill University Health Center, Montreal, Canada; and the [dagger]Department of Anesthesia, University Regensburg, Regensburg, Germany
Received for publication October 13, 2003.
Accepted for publication January 16, 2004.
Correspondence: Thomas Schricker, Department of Anesthesia, Royal Victoria Hospital, 687 Pine Avenue West, Room S5.05, Montreal, Quebec, Canada H3A 1A1. Electronic mail may be sent to thomas.schricker@mcgill.ca.
Copyright American Society for Parenteral and Enteral Nutrition May/Jun 2004
Provided by ProQuest Information and Learning Company. All rights Reserved