Abstract
We undertook a prospective study to determine the safety and effectiveness of the direct administration of a steroid to the eustachian tube via the Silverstein Micro Wick in 11 patients with chronic eustachian tube dysfunction, including two who had Samter's triad. All patients had previously been treated with medical therapy and surgical middle ear ventilation without resolution. The MicroWick was placed directly in the eustachian tube orifice through a pressure-equalization tube. Patients received 3 drops of dexamethasone 4 mg/ml three times a day. The drops were discontinued after 4 weeks, and the MicroWick and ventilation tube were removed after 3 months. At study's end, eight patients (72.7%) reported subjective improvement in terms of a reduction in aural pressure and fullness. Audiometric testing demonstrated a 55% reduction in the mean air-bone gap and a 3% increase in the mean speech discrimination score. Bone pure-tone averages remained stable. Tympanometry showed that five patients (45.5%) converte d from type B or C tympanograms to type A. Four patients (36.4%) had persistent perforations. Both patients with Samter's triad improved with therapy. These preliminary results suggest that direct dexamethasone administration to the eustachian tube is safe and effective for the treatment of chronic eustachian tube dysfunction. Long-term studies to confirm these findings are under way.
Introduction
Chronic eustachian tube dysfunction is frequently encountered by primary care physicians and otolaryngologists. This condition can be difficult to treat, particularly in adults who have a lifelong history of eustachian tube dysfunction. Bluestone and Doyle attribute three major functions to the eustachian tube: ventilation, clearance, and protection of the middle ear. (1) The middle ear tends to lose gas by diffusion into the surrounding mucosal circulation. The normal eustachian tube serves to admit gas in order to equalize middle ear pressure with that of the surrounding environment. Eustachian tube dysfunction can result in negative middle ear pressure and precipitate associated signs and symptoms. These signs and symptoms include conductive hearing loss, tinnitus, otalgia, vertigo, tympanic membrane atelectasis, cholesteatoma formation, and recurrent otitis media. (2-4) Many authors have concluded that eustachian tube dysfunction is the most important precipitating pathology in the development of otitis m edia. (2-6)
Historically, the single most effective treatment for negative middle ear pressure and serous otitis media has been the insertion of a ventilation tube into the tympanic membrane. (2) More recently, laser-assisted tympanostomy has been used to create an opening in the tympanic membrane for 3 to 4 weeks. (7,8) This procedure obviates the need for placing a ventilation tube in half of all affected children and approximately 80% of affected adults. However, no method has been proven effective that involves directly treating eustachian tube pathology when conventional therapy has failed. Several techniques have been proposed over the years. For example, in 1985, Jansen described a posterior tuboplasty procedure in which the osseous portion of the eustachian tube is enlarged. (9) Within a few years, variations of this technique were reported by Charachon et al (10) and Zini. (11) Poe and Kujawski recently described an endoscopic laser-assisted technique that was designed to improve the proximal opening of the nas opharyngeal eustachian tube orifice. (12)
Much of eustachian tube pathology relates to mucosal disease and associated hypertrophy, which can be precipitated by allergic and reactive disease. We have developed a technique for treating chronic eustachian tube dysfunction that involves a transtympanic approach to the eustachian tube. In our method, a patient self-instills a topical steroid via the Micro Wick device (ET MicroWick) over an extended period of time. We propose that direct steroid application via the ET Micro Wick might serve to reduce mucosal hypertrophy and improve eustachian tube function.
Patients and methods
All patients at our tertiary otologic referral center who had chronic eustachian tube dysfunction were offered treatment with the ET Micro Wick provided that they met three selection criteria: (1) their symptoms were consistent with eustachian tube dysfunction (e.g., hearing loss and aural fullness), (2) they had previously undergone both medical therapy and at least one middle ear ventilation procedure, and (3) findings on tympanometry or clinical examination suggested that their middle ear pressure was abnormal. Eleven patients, aged 34 to 90 years (mean: 63), qualified for the study. Two of these patients had eustachian tube dysfunction associated with Samter's triad (bronchial asthma, nasal polyps, and aspirin sensitivity).
Examination of the nasopharynx was performed on all patients to rule out an obstructing mass. Audiograms and impedance tympanometry were obtained on all patients prior to treatment. All patients were monitored with serial testing during and after the completion of therapy.
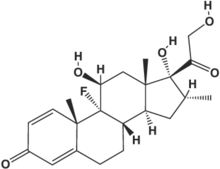
The essentials of our procedure are as follows (figure 1). The ear is anesthetized, and then a laser tympanotomy or vertical myringotomy is made over the protympanum. The middle ear and eustachian tube are examined with a 30[degrees] otoendoscope and an operating microscope to determine if there is an obstructing membrane over the eustachian tube orifice. If such a membrane is present, a small pick is used to clear it. A ventilation tube is inserted into the tympanostomy opening; this should allow for the direct visualization of the eustachian tube through the microscope when the tube is directed properly. The MicroWick is then inserted through the ventilation tube toward the eustachian tube orifice until resistance is met. Then the dexamethasone 4 mg/ml is introduced into the MicroWick.
Patients are instructed to self-administer the medication into the ear while lying down with the treated ear facing upward; they are to remain lying for 15 minutes. The dexamethasone solution is administered three times a day for 4 weeks. Patients concurrently self-administer an antibiotic solution, 2 drops at bedtime, as prophylaxis against otitis externa. At approximately 3 months, the MicroWick and tube are removed, and middle ear otoendoscopy can be repeated to visually assess the eustachian tube response. Then the tympanic membrane is allowed to close.
Results
The 11 patients were treated over a 16-month period. The average follow-up was 7.2 months. The data on one patient spans only the first 2 months postoperatively because this patient had severe otitis media and developed a profound sensorineural hearing loss; there was no evidence to suggest any association between the infection and the MicroWick steroid treatment because the infection occurred 2 months after the wick had been removed.
Air threshold levels were measured preoperatively, postoperatively, and during follow-up (table 1). (We list the means for both the four-frequency pure-tone average [PTA] and the data at each individual frequency because of the variability in the air-bone gap across frequencies.) The mean preoperative PTA was 40 dB; at the most recent follow-up, the mean PTA had improved to 34 dB. The bone threshold PTA was 28 dB preoperatively and 27 dB postoperatively, and no patient experienced sensorineural hearing loss. The mean air-bone gap decreased from 11 to 5 dB with treatment; the 6-dB improvement corresponds to a mean air-bone gap closure of 55% (table 2). This change was not statistically significant. The mean speech discrimination score rose from 94% preoperatively to 97% postoperatively.
Preoperatively, three patients (27.3%) had type A tympanograms, six (54.5%) had type B tympanograms, and two (18.2%) had type C tympanograms. After a mean postoperative follow-up of 8 months in this group, four of the eight who had either a type B or C tympanogram converted to type A, including both patients who had Samter's triad. Four patients (36.4%) had persistent perforations for at least 3 months postoperatively, and three of them subsequently underwent successful fat myringoplasty under local anesthesia in the office; the fourth patient was satisfied with her hearing results, and she chose not to have the perforation patched. Aural fullness or pressure resolved completely in eight patients (72.7%).
Discussion
The role of eustachian tube dysfunction in the development of chronic otitis media with effusion and conductive hearing loss is widely recognized. (1,4,5) However, treatment options remain limited. Middle ear aeration via tympanotomy and tube insertion has been the management of choice for chronic effusions that do not respond to medical therapy. (2) Complications of long-term ventilation tube placement include otorrhea, persistent tympanic membrane perforations, and the inconvenience of adhering to dry-ear precautions. Unfortunately, the underlying patho-physiology usually leads to a recurrence of symptoms when the tube is removed and the tympanic membrane is allowed to heal. (13,14)
The causes of eustachian tube obstruction in adults are varied, but one of the principal pathways involves mucosal edema. (4) The ability of steroids to inhibit inflammation and reduce edema has led to their use in the treatment of chronic serous otitis media. Topical steroids have been shown to shorten the duration of acute serous otitis media, and oral prednisone has been shown to be effective in treating acute serous otitis media, although the degree of its long-term efficacy is unclear. (15)
The incidence of persistent perforations in our study (36.4%) is relatively high, compared with the incidence observed following other applications of the MicroWick (e.g., gentamicin perfusion of the inner ear). It is likely that the steroid solution inhibits tympanic membrane healing by inducing atrophy around the rim of the tympanotomy. This idea is supported by the surgical findings at the time of myringoplasty (figure 2). The membranes were found to be avascular and fragile. However, fat myringoplasty was successful in all cases.
Although the hearing improvement on audiometry was not statistically significant in this study, our overall results were encouraging. Considering that the patients enrolled in our study all had chronic, recurrent disease (including the two who had Samter's triad), the positive trend in hearing ability, the improvement reflected in tympanometry, and the alleviation of aural symptoms suggest that this is an effective treatment. Long-term studies to confirm our findings are under way.
In conclusion, eustachian tube dysfunction remains a common and potentially serious condition for which few treatment options exist. We have presented the results of a new technique that is aimed at reducing mucosal edema in the eustachian tube and restoring tubal patency. The MicroWick is a simple drug delivery system that can specifically target various structures in the middle and inner ear. The ET Micro Wick procedure with dexamethasone perfusion appears to be well tolerated, as side effects were minimal.
Finally, the causes of eustachian tube dysfunction are multifactorial; they include mucosal edema, muscular dysfunction, cartilage collapse, and obstruction by structures in the nasopharynx. As improvements continue in diagnostic techniques for identifying the precise underlying pathophysiology in each individual case, patient selection for this treatment will become more refined.
References
(1.) Bluestone CD, Doyle WJ. Anatomy and physiology of eustachian tube and middle ear related to otitis media. J Allergy Clin Immunol 1988;81(5 Pt 2):997-1003.
(2.) Sade J, Ar A. Middle ear and auditory tube: Middle ear clearance, gas exchange, and pressure regulation. Otolaryngol Head Neck Surg 1997;l16:499-524.
(3.) Bluestone CD, Klein JO. Otitis Media in Infants and Children. 2nd ed. Vol. 1. Philadelphia: W.B. Saunders, 1995:5-38.
(4.) Tos M. The intraluminal obstructive pathogenic concept of eustachian tube in secretory otitis media. In: Sade J, ed. Basic Aspects of the Eustachian Tube and Middle Ear Diseases. Amsterdam: Kugler and Ghedini, 1991:327-33.
(5.) Bluestone CD, Paradise JL, Beery QC. Physiology of the eustachian tube in the pathogenesis and management of middle ear effusions. Laryngoscope 1972;82:1654-70.
(6.) Cantekin EI, Bluestone CD, Parkin LP. Eustachian tube ventilatory function in children. Ann Otol Rhinol Laryngol 1976;85(2 Suppl 25 Pt 2):171-7.
(7.) Silverstein H, Jackson LE, Rosenberg SI, Conlon WS. Pediatric laser-assisted tympanostomy. Laryngoscope 2001 ;111:905-6.
(8.) Silverstein H, Rosenberg SI, Poe D, Jackson LE, eds. Minimally Invasive Otologic Surgery. Clifton Park, N.Y.: Delmar Learning, 2002.
(9.) Jansen CW. Functional repair of the eustachian tube. Am J Otol 1985;6:23 1-2.
(10.) Charachon R, Gratacap B, Lerat M. [Surgery of the bony eustachian tube and tubal isthmus]. Rev Laryngol Otol Rhinol (Bord) 1986;107:45-8.
(11.) Zini C. Osseous tube surgery. Principles and techniques. Vidiotology 1988;1:6-13.
(12.) Poe D, Kujawski O. Endoscopic diagnosis and surgery of eustachian tube dysfunction. In: Silverstein H, Rosenberg SI, Poe D, Jackaon LE, eds. Minimally Invasive Otologic Surgery. Clifton Park, N.Y.: Delmar Learning, 2002.
(13.) Schuknecht HF, Zaytoun GM, Moon CN, Jr. Adult-onset fluid in the tympanomastoid compartment. Diagnosis and management. Arch Otolaryngol 1982;108:759-65.
(14.) Lamp CB, Jr. Chronic secretory otitis media: Etiologic factors and pathologic mechanisms. Laryngoscope 1973;83:276-91.
(15.) Butler CC, van Der Voort JH. Steroids for otitis media with effusion. A systematic review. Arch Pediatr Adolesc Med 2001; 155:641-7.
COPYRIGHT 2003 Medquest Communications, LLC
COPYRIGHT 2003 Gale Group