Incyte Corporation (Nasdaq:INCY) has announced positive results from Study 203, a six-month randomized double-blind Phase IIb trial, involving 199 patients and 25 clinical sites in the U.S. and Europe to evaluate the efficacy, dose response, safety and tolerability of Reverset in treatment- experienced human immunodeficiency virus (HIV) infected patients who are failing their current treatment regimens. Results from the first two stages of Study 203 presented at the 3rd International AIDS Society (IAS) Conference on HIV Pathogenesis and Treatment, in Rio de Janeiro, suggest that the highest of three once-daily doses of Reverset provided the greatest antiviral suppression in these highly treatment-experienced patients who have a wide variety of HIV mutations.
The protocol for Study 203 was divided into three stages. The first two stages of the study were designed to evaluate three different doses of Reverset (50, 100 and 200 mg once daily) versus placebo at two different time points, at week two (prior to any optimization of background therapy) and week 16 (after potential optimization of background therapy at the end of week two). The third stage of the trial, which begins at week 16 and ends at week 24, allows all placebo patients to crossover to receive either the 100 or 200 mg dose of Reverset, and permits an additional optimization of background therapy and allows for additional longer-term safety data.
Summary of Results
Two- and 16-week results presented at the IAS conference demonstrated that patients receiving the 200 mg dose of Reverset experienced significant antiviral benefit. At two weeks, when the 200 mg dose of Reverset was used as add-on therapy in patients who were failing their current treatment, patients who received Reverset achieved:
-- a 0.7 log drop in viral load overall as compared to placebo patients who did not achieve any change in viral load; and
-- a 1.1 log drop in viral load in the subset of patients not using 3TC or FTC in their background treatment regimen. At 16 weeks in the overall group, when the 200 mg dose of Reverset was used as add-on therapy in either an optimized or non-optimized regimen, patients who received Reverset achieved:
-- a 1.2 log drop in viral load versus a 0.8 log drop for the placebo patients;
-- a 1.4 log drop in viral load in the subset of patients who were not receiving 3TC or FTC in their background treatment regimen versus a 0.5 log drop for the placebo patients; and
-- a 54% response rate versus a 40% response rate as compared to placebo with response defined as more than a 1.0 log drop in viral load. The response rate among patients not receiving 3TC or FTC in their background treatment regimen was 80% versus 25% on placebo. At 16 weeks, in the non-optimized group, patients who received the 200 mg dose of Reverset achieved:
-- a 0.6 log drop in viral load as compared to non-optimized placebo patients who achieved a 0.1 log drop; and
-- a 1.5 log drop in viral load in the subset of patients who were not receiving 3TC or FTC in their background treatment regimen as compared to a 0.3 log increase in the non-optimized placebo patients not receiving 3TC or FTC.
In this trial the 100 mg and 50 mg daily doses of Reverset were less effective than the 200 mg dose, with viral load decreases of 0.3 to 0.4 log during the two week add-on phase and viral load decreases of 0.8 to 0.9 log at week 16 following the optimized background phase of the study.
Effects Against HIV Mutations
Reverset was also shown to be effective in patients with virus resistant to other commonly used nucleoside analog reverse transcriptase inhibitors (NRTIs), including viruses harboring multiple thymidine analog mutations (TAMS), including the M41L and L210W mutations, and the L74V and M184V mutations. Sixty-six percent of the patients had the M184V mutation; 46% had the M41L and L210W mutations; 44% had 4 to 6 TAMS; and 6% had K65R. There were too few instances of virus with the K65R mutation in patients receiving the 200 mg dose to draw firm conclusions; however, the viral load reduction in patients with the K65R mutation treated with lower doses of Reverset suggests that the compound is also active against this mutation.
Tolerability
Reverset was generally well tolerated in this study. Clinical adverse events were generally mild, with the only possibly related events of at least moderate severity reported in more than one of the 151 Reverset-treated patients at any dose being nausea (4 patients, 2.6%), headache (4 patients, 2.6%), diarrhea (3 patients, 2.0%), pancreatitis (2 patients, 1.3%), and myalgia (2 patients, 1.3%). During up to 24 weeks of therapy, asymptomatic increases in serum lipase to greater than 5 times the upper limit of the normal range (Grade 4) were seen in 50% of patients receiving 200 mg Reverset with ddI (didanosine), and we have concluded Reverset should not be used with ddI. Two patients receiving Reverset 100 mg with ddI and tenofovir in combination at higher than recommended doses of ddI or tenofovir developed symptoms of pancreatitis which resolved within days of discontinuation of ddI, tenofovir and Reverset. Didanosine labeling states that the dose of ddI should be reduced when co-administered with tenofovir because of increased risks of ddI toxicity, including pancreatitis. Importantly, in patients who were not also receiving didanosine (ddI), asymptomatic hyperlipasemia was reported in 2 patients (5%) receiving 200 mg Reverset and in one placebo-treated subject (3%).
Calvin Cohen, M.D., M.S., the presenting clinical investigator and Research Director for both Harvard Vanguard Medical Associates and Community Research Initiative of New England, stated, "The 200 mg dose of Reverset demonstrated potent, clinically meaningful antiviral effects in highly treatment-experienced patients, including patients carrying many of the common resistant viruses that we as physicians struggle to combat. When Reverset was used without other cytidine analogs, 3TC and FTC, it was a very powerful drug against resistant virus. The fact that Reverset was generally well tolerated in these highly treatment-experienced patients at the 200 mg once-daily dose is equally important and warrants confidence in its potential therapeutic value." Robert Murphy, M.D., Professor of Medicine, Northwestern University, and the principal investigator for Study 203, added, "As one of the original Reverset investigators, it is especially gratifying to see these positive longer-term results. Reverset is clearly a very potent and potentially important new HIV therapy with its once-a-day formulation, good tolerability and activity against key mutations. I look forward to seeing Reverset advance into Phase III development."
About Study 203
Study 203 was designed to assess the efficacy, safety and tolerability of Reverset over a six-month period, to determine the most appropriate dose of Reverset, and to identify patients for whom Reverset is likely to provide the greatest benefit.
The study involves 199 treatment-experienced patients who were failing their current treatment regimen. Patients in Study 203 had a mean baseline viral load of 4.5 log10. At entry, patients were randomized to receive one of three doses of Reverset (50, 100 and 200mg) once a day or placebo. During the first 14 days of the trial, study medication was added to a patient's failing regimen. At the end of 14 days, physicians had the option to optimize the background regimen of any patient based on their prior treatment history and the results of a viral genotype obtained during the screening period. In approximately seventy percent of the patients in the study, the physician optimized the background regimen at this point, with the remaining thirty percent continuing the original failing regimen plus randomized study medication (these latter patients were defined as non-optimizers). At week 16, all placebo patients were randomized to either the 100 or 200 mg dose of Reverset and study physicians were again given the option to reoptimize the background therapy of any patient if appropriate.
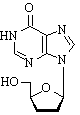
About Reverset
Reverset is a nucleoside analog reverse transcriptase inhibitor that is being developed as a once-daily oral HIV therapy by Incyte Corporation and Pharmasset, Inc. under their collaborative licensing agreement.
About Incyte
Incyte is a Wilmington, Delaware-based drug discovery and development company with a growing pipeline of oral compounds to treat HIV, inflammation, cancer and diabetes. The company's most advanced product candidate, Reverset, is an oral, once-a-day therapy in Phase II clinical trials to treat patients with HIV infection. The company's lead internal compounds include INCB3284, a proprietary oral CCR2 antagonist that is in Phase II development for a number of chronic inflammatory conditions, and INCB7839, a proprietary, oral sheddase inhibitor that is in Phase I development as a potential treatment for solid cancers. Incyte has several other early drug discovery programs underway in the areas of cancer, inflammation, diabetes and HIV.
About Pharmasset
Pharmasset is an emerging pharmaceutical company committed to the discovery, development, and commercialization of novel antiviral drugs. The company leverages its expertise in nucleoside chemistry to develop therapeutics to combat infections caused by drug-resistant human immunodeficiency virus (HIV) and hepatitis viruses. Pharmasset's product candidates include Clevudine(TM), which is in late-stage clinical trials for the treatment of chronic Hepatitis B, Reverset and Racivir(R), two drugs in Phase 2 clinical trials for the treatment of HIV, and several other antiviral compounds in advanced preclinical studies.
In 2003, Pharmasset entered into a collaborative licensing agreement with Incyte Corporation for the development and commercialization of Reverset in certain territories. In 2004, Pharmasset entered into a collaboration agreement with Hoffmann-La Roche for the development and commercialization of PSI-6130 in certain territories for the treatment of Hepatitis C. Pharmasset retains proprietary development and commercialization rights to the balance of its clinical and preclinical pipeline.
For more information, call 302/498-6944.
COPYRIGHT 2005 Worldwide Videotex
COPYRIGHT 2005 Gale Group