Follow up of microfilaraemic individuals infected with Wuchereria bancrofit at five years after treatment was carried out in a tea workers population. Diethylcarbamazine citrate in the dose schedule of 72 mg/kg body weight given in equal daily doses over a period of 21 days cleared 51.6 per cent microfilaraemic individuals five year post-treatment. Eighty five subjects were successfully followed and among these, 10 (11.8%) showed increase in mf counts, 31 (36.4%) showed reduction but remained microfilaraemic and 44 (51.8%) became amicrofilaraemic. The age and sex of the host had no significant effect on the clearance of mf. Persistence of a relatively stable low number of mf in treated individuals is more likely due to survival of one or more female worms after the therapy or due to reinfection which could not be ruled out in the present study. Overall, findings indicated that diethylcarbamazine citrate appeared to give a long-term benefit to treated individuals.
Key words Bancroftian filariasis - diethylcarbamazine citrate - microfilaraemia - Wuchereria bancrofti
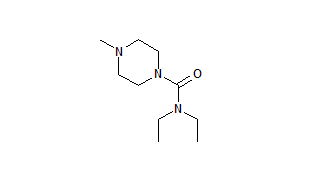
Diethylcarbamazine citrate (DEC) is the drug of choice for lymphatic filariasis1,2. Studies pertaining to the most effective dose regimen of DEC suitable for mass and selective chemotherapy have proved the high efficacy of the WHO recommended dose i.e., 72 mg DEC / kg body wt in divided daily doses over 12 days2.
Since the introduction of DEC in India, many community trials have been conducted on different dose regimens3,4. The efficacy of DEC at the dose of 6 mg/kg/day for 12 days tested in Gujarat, Uttar Pradesh and Andhra Pradesh had shown significant reduction in microfilaria (mf) prevalence and moderate to no effect on disease rate5,6. Single and biannual standard doses of DEC tried against brugian filariasis in Kerala had shown significant reduction in microfilarae and disease rate7.
Though lymphatic filariasis had been reported from Assam state8,9, no data are available on the efficacy of DEC against lymphatic filariasis. The present communication is an attempt in this direction.
Material & Methods
The prevalence of lymphatic filariasis was investigated in a labour population of a tea garden of district Dibrugarh, Upper Assam during 1992-93(10). The workers, migrants many generations earlier from Orissa, Bengal, Bihar, Madhya Pradesh, Uttar Pradesh and south Indian states, lived in established densely populated workers' lines near or around the tea factory. These workers were mainly engaged in the plucking of tea leaves and tea plantation through out the year. Almost all the workers included in this study resided in the houses provided by the tea company.
Study design : The aims and objectives of the survey were explained to the workers and informed verbal consent was taken. The workers were registered during a house-to-house survey. Following the survey, it was found that only Wuchereria bancrofti was prevalent and the garden doctor in-charge, was informed accordingly. The patients were provided DEC treatment as per the WHO recommended dose11. Using the same methods, the treated microfilaraemic individuals were re-examined after the fifth year posttreatment, for the presence of microfilaria.
Parasitological examination : Finger prick blood samples (20 cmm) were obtained between 2000 0100 h, thick blood smear was prepared, stained with 10 per cent Giemsa and examined for the presence of microfilarae. The microfilarae were counted and the number per ml of blood was calculated as per the technique of McMahon et al12. All possible efforts were made to sample the blood from individuals at the same time as per the pretreatment surveys.
DEC tablets [50 mg; Banocide(R), Burroughs' Wellcome (India) Limited] in the dose regimen of 72 mg/kg body wt i.e., 3.428 mg/kg body wt/day were given. Subjects in the present study, aged 5 yr or above, were in the weight range of 15-61 kg. Doses were calculated to the nearest half tablet (25 mg) based on the body weight measured on a portable weighing machine. Accordingly, 1 to 4 tablets per day as per the calculated dose were given for a period of 21 days. The drug was administered by the doctor of the garden hospital along with one of the research team who was also a co-investigator during the first phase of the work i.e., first night blood survey and administration of the DEC. Some irregularities or refusal of taking the drug were also recorded. Individuals complaining of minor side effects were treated accordingly.
The geometric mean microfilaria intensity (GMI) was calculated as done by Simonsen et al13 i.e, antilog [(Sigma)log(x +1)/n] where x is the number of microfilarae (mf) per ml in the blood and n is the total number of microfilaraemic subjects examined. Subjects becoming amicrofilaraemic on post treatment observation were also included when calculating the geometric mean. Those who did not complete the full treatment or missed follow up examinations due to refusal, migration or death were excluded.
Results & Discussion
The results of the surveys are summarized in Table I. In the pretreatment survey, 1459 subjects (664 males; 795 females) with an average age of 22.2 yr (range 1-78 yr) were sampled and examined for the presence of mf. The prevalence rate of mf was 8.29 per cent. Of the 121 microfilaraemic subjects, 85 (70.25%) finally completed DEC treatment and were followed successfully. Of the 36 dropouts, 14 were females and 22 males . Reasons for dropout were (i) migration due to marriages of young women (7); (ii) change of job to another garden (11); (iii) noncooperation in the second survey (7); (iv) non completion of treatment (6); and (v) death (5). The geometric mean mf density was 701 for female and 666 for male per ml of blood. Total mean mf density of the 36 dropouts was 667 per ml of blood.
The standard 72 mg DEC treatment resulted in mf clearance rate of 51.8 per cent five years after treatment. No significant effect of age and sex of the host, on the clearance of mf was noticed. Of the 85 subjects who were successfully followed, 10 (11.8%; group I) showed increase in mf counts, 31 (36.4%; group II) showed reduction but remained microfilaraemic and 44 (51.8%; group III) became amicrofilaraemic. However, on grouping of the 85 treated patients into low, moderate and high mf counts before and after the DEC treatment, reduction in mean mf counts was found in all the groups as compared to pre-treatment counts (Table II). Age-- wise mean mf density before and after treatment are presented in the Fig.
Although DEC is considered the drug of choice, many basic questions remain about its effectiveness and how best to use it for controlling filariasis in a population14. Our findings suggest that the effect of DEC treatment on the mf status in treated individuals remains for a considerable period. The efficacy of DEC in terms of microfilaria clearance and reduction in mf density might have been more clear if surveys were conducted yearly, but this was not done due to limitation in the study design. The probability of reinfection could not be ruled out as the individuals resided in an endemic area where no effective vector control measures had been undertaken. Microfilaria in treated individuals is probably due to survival of a few female worms or due to reinfection. Three types of subjects were observed in respect of response to the drug and mf clearance1. In the first pattern, individuals showed increase in mf count, second were subjects who showed reduction in mf count but were microfilaraemic and third were individuals who became amicrofilaraemic. However, it is not known how these patterns vary among the population. DEC kills parasites indirectly by activating the host immune response and it appears that varying degrees of immunity in subjects may be responsible for the differential action of the drug on the parasite15,16 or by modifying the parasite cuticular surface17. Increased or a static mf count post-treatment was probably due to a very low pre-treatment mf count and a slight increase in the post-treatment count gave rise to an unusually large percentage increase or it was due to reinfection1. Moreover, when all the 85 treated mf carriers were grouped in low (50 mf) mf counts per 20 cmm of blood on the basis of pretreatment counts, it was seen that after therapy, highest i.e., 65.2 per cent of the cases became negative in low count group and lowest in high count group (36.8%). However, in terms of reduction in mean mf density after treatment, highest reduction was seen in the high mf count group (Table II). Reduction in mean mf density in treated individuals after a period of five years suggests a prolonged effect of DEC on microfilaraemia status. The finding of constant low level microfilaraemia for longer period in same individuals is difficult to explain on the basis of what is known about filarial biology or through DEC resistant in microfilarae among treated individuals. The longevity of microfilarae in host blood in an experimental model has been shown to be 1-1.5 yr only19. The adulticidal action of DEC is now well established20, however, total clearance of adult worms from treated individuals is difficult and the probability of survival of one or a few adult females is fairly high21. The persistence of a relatively stable low number of mf over a period of several years is more likely due to survival of one or more female worms which mate and periodically release new microfilarae22.
The results of this study suggest that DEC at the dose of 72 mg/kg body wt administered over 21 days is efficacious and provides long-term benefits to treated individuals. However, the presence of some microfilaria carriers following therapy indicates persistence of infection due to survival of some female worms or due to reinfection which cannot be ruled out in this study.
Acknowledgment
The authors thank the management and medical personnel of the tea garden for help in carrying out the study.
References
1. Ottesen EA. Efficacy of diethylcarbamazine in eradicating infection with lymphatic-dwelling filariae in humans. Rev Infect Dis 1985: 7: 341-56.
2. Lymphatic filariasis : The disease and its control. Fifth report of the WHO Expert Committee on Filariasis. Tech Rep Ser No. 821. Geneva : World Health Organisation, 1992 : 42-8.
3. Rao CK, Sen T, Roychowdhury SP, Dutta KK, Das M, Rao CK, et al. Rural filariasis control with diethylcarbamazine. J Commun Dis 1978; 10: 194-6.
4. Rajagopalan PK, Pani SP. Community drug trials for lymphatic filariasis control in India. Natl Med J India 1991; 4: 71-6.
Raina VK, Kosare GJ, Das M, Rao CK. Impact of diethylcarbamazine treatment of selective microfilaria carriers and filarial cases under rural filaria control project in Valsad district, Gujarat. J Commun Dis 1984; 16 : 247-9. 6. Sharma SP, Biswas H, Pandey DS, Pandey RS, Das M, Sharma GK. Control of bancroftian filariasis in a rural area through selected treatment with diethylcarbamazine. J Commun Dis 1987; 19: 322-5.
Rajagopalan PK, Krishnamoorthy K, Panickar KN, Sabesan S. Epidemiological assessment of different intervention measures for the control of malayan filariasis in Shertallai, South India. Vector Control Res Centre Misc Publ 1990; 17: 1-9.
Basu PC. Filariasis in Assam state. Indian J Malariol 1957; ll: 293-308.
Population exposed to the risk of filariasis, microfilaria. carriers and chronic filaria cases as in 1989. In : Health information of India. New Delhi : Directorate General of Health Services, Ministry of Health and Family Welfare, Govt. of India, 1990: 148.
10. Dutta P, Gogoi BK, Chelleng PK, Bhattacharyya DR, Khan SA, Goswami BK, et al. Filariasis in the labour population of a tea state in Upper Assam. Indian J Med Res 1995; Inl: 245-6.
1. WHO Expert Committee on Filariasis, Third Report, WHO Tech Rep Ser No. 542, Geneva: World Health Organisation, 1974 : 9-10.
12. McMahon JE, Marshall TF, De C, Vaughan JP, Abaru DE. Bancroftian filariasis : a comparison of microfilarae counting techniques using counting chamber, standard slide and membrane (nucleopore) filtration. Ann Trop Med Parasitol 1979; 73 : 457-64.
13. Simonsen PE, Meyrowitsch DW, Makunde WH. Bancroftian filariasis: long term effect of the DEC provocative day test on microfilaraemia. Trans R Soc Trop Med Hyg 1997; 91 290-3.
14. Eberhard ML, Lammie PJ, Dickinson CM, Roberts JM. Evidence of non susceptibility to diethylcarbamazine in Wuchereria bancrofti. J Infect Dis 1991; 163: 1157-60. 15. Lammie PJ, Leiva LE, Ruff AJ, Eberhard ML, Lowrie RC, Katz SP. Bancroftian filariasis in Haiti : preliminary characterization of the immunological responsiveness of microfilaremic individuals. Am J Trop Med Hyg 1988; 38 125-9.
16. Lammie PJ, Eberhard ML, Leiva LE, Lowrie RC Jr, Katz SP. The effect of diethylcarbamazine treatment of bancroftian filariasis on the immunological reactivity of microfilaraemic individuals. Trans R Soc Trop Med Hyg 1988; 82: 726-9. 17. Ottesen EA. Description mechanism and control of reactions to treatment in human filariasis. In: Filariasis. Ciba Foundation Symposium No. 127. 1987: 265-83. 18. Eberhard ML, Dickerson JW, Hightower AW, Lammie PJ. Bancroftian filariasis : long term effects of treatment with diethylcarbamazine in a Haitian population. Am J Trop Med Hyg 1991; 45: 728-33.
19. Eberhard ML. Longevity of microfilariae following removal of the adult worms. Trop Med Parasitol 1986; 37: 361-3.
20. Figueredo-Silva J, Jungmann P, Noroes J, Piessens WF, Coutinho A, Brito C, et al. Histological evidence for adulticidal effect of low doses of diethylcarbamazine in bancroftian filariasis. Trans R Soc Trop Med Hyg 1996; 90: 192-4. 21. Dreyer G, Amaral F, Noroes J, Medeiros Z, Addiss D. A new tool to assess the adulticidal efficacy in vivo of antifilarial drugs for bancroftian filariasis. Trans R Soc Trop Med Hyg 1995; 89: 225-6.
22. Beaver PC, Orihel TC, Johnson MH. Dipetalonema viteae in the experimentally infected jird, Meriones unguiculatus. II : Microfilaremia in relation to worm burden. J Parasitol 1974; 60: 310-5.
A.M. Khan, P. Dutta, S.A. Khan, N.K. Baruah, C.K. Sarma & J. Mahanta
Regional Medical Research Centre, Dibrugarh
Reprint requests: Dr J. Mahanta, Director, Regional Medical Research Centre Northeastern Region (ICMR), Box No. 105, Dibrugarh 786001
Copyright Indian Council of Medical Research Oct 1998
Provided by ProQuest Information and Learning Company. All rights Reserved