Common infectious forms of vaginitis include bacterial vaginosis, vulvovaginal candidiasis, and trichomoniasis. Vaginitis also can occur because of atrophic changes. Bacterial vaginosis is caused by proliferation of Gardnerella vaginalis, Mycoplasma hominis, and anaerobes. The diagnosis is based primarily on the Amsel criteria (milky discharge, pH greater than 4.5, positive whiff test, clue cells in a wet-mount preparation). The standard treatment is oral metronidazole in a dosage of 500 mg twice daily for seven days. Vulvovaginal candidiasis can be difficult to diagnose because characteristic signs and symptoms (thick, white discharge, dysuria, vulvovaginal pruritus and swelling) are not specific for the infection. Diagnosis should rely on microscopic examination of a sample from the lateral vaginal wall (10 to 20 percent potassium hydroxide preparation). Cultures are helpful in women with recurrent or complicated vulvovaginal candidiasis, because species other than Candida albicans (e.g., Candida glabrata, Candida tropicalis) may be present. Topical azole and oral fluconazole are equally efficacious in the management of uncomplicated vulvovaginal candidiasis, but a more extensive regimen may be required for complicated infections. Trichomoniasis may cause a foul-smelling, frothy discharge and, in most affected women, vaginal inflammatory changes. Culture and DNA probe testing are useful in diagnosing the infection; examinations of wet-mount preparations have a high false-negative rate. The standard treatment for trichomoniasis is a single 2-g oral dose of metronidazole. Atrophic vaginitis results from estrogen deficiency. Treatment with topical estrogen is effective. (Am Fam Physician 2004;70:2125-32,2139-40. Copyright[C] 2004 American Academy of Family Physicians.)
Vaginitis is among the most common conditions for which women seek medical care, with vaginal discharge accounting for approximately 10 million office visits each year. (1) Although vaginitis can have a variety of causes (Table 1), it most often is associated with infection or atrophic changes. Common infectious forms of vaginitis include bacterial vaginosis, vulvovaginal candidiasis, and trichomoniasis. Although these infections generally respond to treatment, misdiagnosis and, rarely, pharmacologic resistance may occur.
In almost all patients with vaginitis, it is important to perform a thorough assessment that includes speculum examination, pH testing, wet-mount and potassium hydroxide (KOH) preparations, and cultures when indicated. This article reviews the diagnosis and management of bacterial vaginosis, vulvovaginal candidiasis, trichomoniasis, and vaginal atrophy.
Diagnosis
Although it is tempting to treat vaginal complaints empirically based on the patient's history alone, studies (2,3) have demonstrated poor correlation between symptoms and the final diagnosis. Bacterial vaginosis often is identified based on the vaginal pH and the presence of clue cells on light microscopy (two of the Amsel criteria (4)). A recent analysis (3) found that examination of wet-mount preparations is neither highly sensitive nor specific for vulvovaginal candidiasis. Culture of the vagina is costly, but may be the only way to ensure diagnosis of vulvovaginal candidiasis in equivocal cases. A reasonable alternative is to use a wet-mount and KOH preparation or Gram stain of the vagina in conjunction with the findings of the physical examination, and to reserve culture for cases of treatment failure. (5) DNA-based diagnostic tools with varying degrees of sensitivity and specificity also are avail-able. Finally, a recent study (6) showed that in adolescents, vaginal swabs for wet-mount and KOH preparations may be performed reliably without speculum examination.
Bacterial Vaginosis
Bacterial vaginosis accounts for 10 to 30 percent of the cases of infectious vaginitis in women of childbearing age. (7) In bacterial vaginosis, there is a decrease in normal lactobacilli and a proliferation of Gardnerella vaginalis, Mycoplasma hominis, and anaerobes, including Mobiluncus, Bacteroides, and Peptostreptococcus species.
The Amsel criteria are considered to be the standard diagnostic approach to bacterial vaginosis and continue to be generally reliable. (7,8) The criteria are as follows: milky, homogeneous, adherent discharge; vaginal pH greater than 4.5; positive whiff test (the discharge typically has a fishy smell); and presence of clue cells in the vaginal fluid on light microscopy. (4) If three of the four criteria are met, there is a 90 percent likelihood of bacterial vaginosis. The presence of small gram-negative rods or gram-variable rods and the absence of longer lactobacilli on a Gram stain of the vaginal discharge also is highly predictive of bacterial vaginosis. (9) However, this method of diagnosis is impractical in most family physicians' offices. Because G. vaginalis commonly is found in asymptomatic women, culture is not useful.
According to guidelines from the Centers for Disease Control and Prevention (CDC),10 treatment of bacterial vaginosis is indicated to reduce symptoms and prevent infectious complications associated with pregnancy termination and hysterectomy. Treatment also may reduce the risk of human immunodeficiency virus (HIV) transmission. (10) Thus, it is reasonable to treat asymptomatic patients who are scheduled for hysterectomy or pregnancy termination or who are at increased risk for HIV infection; (10) other asymptomatic patients need not be treated.
Treatment
The standard treatment for bacterial vaginosis is metronidazole (Flagyl) in a dos-age of 500 mg orally twice daily for seven days (Table 2). (10) Although other treatments have been shown to have approximately equivalent efficacy, (11-16) they are associated with higher recurrence rates. These agents include 0.75 percent metronidazole gel (MetroGel-Vaginal) and 2 percent clindamycin cream (Cleocin). Less effective alter-natives include metronidazole in a single 2-g oral dose, oral clindamycin, and intra-vaginal clindamycin ovules.
BACTERIAL VAGINOSIS IN PREGNANCY
Bacterial vaginosis has been shown to be a risk factor for premature labor and perinatal infection. (17) Although evidence supports treatment of high-risk pregnant women with bacterial vaginosis (5) (defined as women who previously delivered a premature infant),7 the benefits of treating asymptomatic, low-risk pregnant women is less clear. (18-20)
A Cochrane review (21) concluded that no evidence supports screening all pregnant women for bacterial vaginosis. Guidelines from the American College of Obstetricians and Gynecologists (22) and the Agency for Healthcare Research and Quality (23) do not recommend screening in low-risk patients (i.e., those without symptoms). However, family physicians should be aware that one recent study (24) demonstrated a significant reduction in spontaneous preterm birth and late miscarriage after treatment with oral clindamycin, 300 mg twice daily for five days, in women with asymptomatic bacterial vaginosis who were at 12 to 20 weeks of gestation. Therefore, the current recommendations against screening and treating asymptomatic pregnant women may be reevaluated.
Because of concerns about teratogenicity, many physicians hesitate to use oral metronidazole in women who are in the first trimester of pregnancy. However, one meta-analysis (25) showed no increased risk of birth defect in infants exposed to metronidazole in utero. Vaginal clindamycin does not reduce the risk of preterm birth or peripartum infec-tion. (19) In fact, the CDC (10) advises that topical clindamycin cream may increase the risk of prematurity and neonatal infections.
RECURRENT BACTERIAL VAGINOSIS
Recurrent bacterial vaginosis is common and requires longer treatment (10 to 14 days) with any of the recommended or alternative therapies (9) (Table 2). (10) Although lactobacillus suppositories (26) and oral lactobacillus (27) (without concurrent antibiotic treatment) have been shown to briefly resolve bacterial vaginosis, recurrence rates with these treatments have been high. (26)
Vulvovaginal Candidiasis
Reported risk factors for vulvovaginal candidiasis include recent antibiotic use, uncontrolled diabetes mellitus, and HIV infection/acquired immunodeficiency syndrome. (28,29) Although Candida albicans frequently is the cause of vaginal yeast infections, the organism can be present in asymptomatic women. Family physicians also must remember that vaginal yeast infections may be caused by species other than C. albicans, such as Candida glabrata and Candida tropicalis. Infections with these species are less common than C. albicans infection and tend to be more resistant to treatment.
Patients with vulvovaginal candidiasis usu-ally report one or more of the following: vulvovaginal pruritus (50 percent), vulvovaginal swelling (24 percent), and dysuria (33 per-cent). (29) The characteristic vaginal discharge, when present, is usually thick and white. Because these symptoms are not specific for vulvovaginal candidiasis, family physicians also should consider other causes.
Caution should be exercised in basing treatment decisions on a patient's self-diagnosis of yeast infection. In one study, (30) the presence of vulvovaginal candidiasis was confirmed in only 33.7 percent of women who self-diagnosed yeast infection. Therefore, the diagnosis of vulvovaginal candidiasis should rely heavily on microscopic examination of a sample taken from the lateral vaginal wall (10 to 20 percent KOH preparation). Although vaginal culture is not routinely necessary for diagnosis, it can be helpful in women with recurrent symptoms or women with typical symptoms and a negative KOH preparation. (7,28)
TREATMENT
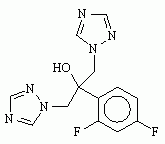
All standard treatment regimens for uncomplicated vulvovaginal candidiasis are equally efficacious, resulting in a clinical cure rate of approximately 80 percent (7) (Table 3).10,31 Various topical treatments are available without prescription. However, many women may prefer the simplicity of a single 150-mg oral dose of fluconazole (Diflucan). In women with candidal vaginitis, treatment with oral fluconazole has been shown to be safe and as effective as seven days of treatment with intravaginal clotrimazole. (31) It is important to remember that fluconazole is a pregnancy class C agent. In some patients, fluconazole may cause gastrointestinal upset, headache, dizziness, and rash, although these side effects typically are mild.
When therapy for vulvovaginal candidiasis is considered, it is helpful to classify the infection as uncomplicated or complicated (Table 4). (10) The practical importance of such classification is that the treatments differ. For example, in complicated vulvovaginal candidiasis, topical therapy has been shown to be more effective than single-dose oral therapy, (28) but treatment should be extended to 10 to 14 days. (7)
If oral therapy is preferred for severe vulvovaginal candidiasis, two sequential 150-mg doses of fluconazole, given three days apart, have been shown to be superior to a single 150-mg dose. (32) Although the optimal duration of extended oral fluconazole therapy has not been determined, one older study (33) comparing oral fluconazole with clotrimazole found that extended use of fluconazole was safe and well tolerated.
In patients with severe discomfort secondary to vulvitis, the combination of a low-potency steroid cream and a topical antifungal cream may be beneficial. (34)
RECURRENT VULVOVAGINAL CANDIDIASIS
Recurrent vulvovaginal candidiasis is defined as four or more yeast infections in one year. The possibility of uncontrolled diabetes mellitus or immunodeficiency should be considered in women with recurrent vulvovaginal candidiasis. When it is certain that no reversible causes are present (e.g., antibiotic therapy, uncontrolled diabetes, oral contraceptive pill use) and initial therapy has been completed, maintenance therapy may be appropriate. (35) Selected long-term regimens are listed in Table The role of boric acid and lactobacillus therapy remains controversial.
Culture and sensitivity results should be used to guide therapy, because non-C. albicans species often are present in women with recurrent vulvovaginal candidiasis and these species are more likely to be resistant to standard azole therapy. (35)
Trichomoniasis
Trichomonas vaginalis infection causes a foul-smelling, frothy discharge that usually is accompanied by vaginal irritation. Although the presence of motile trichomonads in a wet-mount preparation is diagnostic, the examination can be negative in up to 50 percent of women with culture-confirmed infection. (36) Therefore, when microscopic examination of a wet-mount preparation is negative but trichomoniasis still is suspected, a vaginal culture on specialized culture medium is appropriate to rule out T. vaginalis infection. (37) A DNA probe test (e.g., Affirm VPIII) also can be useful in detecting this organism.
Unlike women with asymptomatic G. vaginalis or Candida colonization, women with asymptomatic T. vaginalis infection should be treated. T. vaginalis is highly transmissible and is associated with other sexually transmitted diseases (STDs); asymptomatic infection may increase the risk of acquiring HIV. (10,38) Consequently, patients with vaginal trichomoniasis should be offered HIV and other STD screening.
Occasionally, T. vaginalis is found incidentally in a routine Papanicolaou (Pap) test. Detection by this method is reported to be 57 percent sensitive and 97 percent specific for trichomoniasis. (39)
When trichomoniasis is found during routine Pap testing, management should be based on the pretest probability of infection in the patient, which is determined by the prevalence of T. vaginalis infection in the community; information on prevalence usually can be obtained from the local health department. For example, if the pretest probability of T. vaginalis infection is 20 percent and the protozoan is found in a patient's Pap smear, the positive predictive value of the test is 83 percent, which warrants treatment. Alternatively, the patient can be offered the options of treatment or confirmatory culture followed by treatment if the culture is positive. (39)
TREATMENT
The standard treatment for trichomoniasis is a single 2-g oral dose of metronidazole. (10) An alternative treatment is oral metronidazole in a dosage of 500 mg twice daily for seven days. (10) Because T. vaginalis can colonize the urethra and associated glands, topical therapy is less effective. (10) However, topical agents have been shown to decrease symptoms and may be useful in patients with the rare problem of metronidazole resistance. (40)
Because metronidazole is the only agent that is used to treat T. vaginalis infection, potential management problems include hypersensitivity and drug resistance. A desensitization protocol is available for the management of documented trichomoniasis and frank allergy to metronidazole. (41)
Although evidence indicates that resistance of T. vaginalis to metronidazole can be overcome by increasing the dosage and duration of therapy, many patients cannot tolerate the regimens. If tolerance is a problem, the CDC (10) recommends repeating the 2-g dose of metronidazole orally and if the patient still is infected, giving oral metronidazole in a dosage of 2 g per day for three to five days. (10) If the infection does not respond to this regimen, consultation with the CDC is available by telephone (800-227-8922) or via the CDC Web site (http://www.cdc.gov/std/).
Several alternative regimens for trichomoniasis have been shown to be efficacious. Tinidazole (marketed as Fasigyn) is widely used in Europe and developing countries. This agent is effective and generally well tolerated, (42) but has not been approved by the U.S. Food and Drug Administration and, therefore, is not available in this country. Another treatment option is paromomycin (Humatin) in a dosage of 5 g intravaginally per day for 14 days. This treatment is reported to be effective in 58 percent of patients. (43) However, paromomycin must be used with caution because of its side effects, which include vulvitis and local ulceration.
TRICHOMONIASIS DURING PREGNANCY
T. vaginalis infection during pregnancy has been linked to preterm labor and low birth weight. (10) Unfortunately, treatment of asymptomatic trichomoniasis has not been shown to prevent these outcomes. (44) The decision to treat trichomoniasis during pregnancy is further complicated by the fact that physicians are reluctant to use metronidazole in pregnant women. As previously noted, how-ever, the risk of teratogenicity appears to be overstated. (25) Risks and benefits of treatment must be considered in formulating a treatment plan for pregnant patients who have T. vaginalis infection. The CDC (10) advises treatment of symptomatic pregnant women with a single 2-g oral dose of metronidazole but does not recommend treatment of asymptomatic pregnant women.
Atrophic Vaginitis
The decrease in estrogen levels during perimenopause and after menopause can cause vaginal atrophy. One important physiologic change is thinning of the vaginal epithelium; another is loss of glycogen, which leads to changes in the vaginal pH and flora. Many women with these vaginal changes are minimally symptomatic and require only explanation and reassurance. In women with more severe changes, vaginal irritation, dyspareunia, and fragility may become problems. Atrophy is diagnosed by the presence of a thin, clear or bloody discharge, a vaginal pH of 5 to 7, loss of vaginal rugae, and the finding of parabasal epithelial cells on microscopic examination of a wet-mount preparation. (18)
Treatment with topical estrogen (cream, tablet, or ring) usually provides complete relief of symptoms within weeks. In the interim, patients may obtain relief through use of vaginal lubricants and moisturizers (e.g., Astroglide, Replens). Rarely, endometrial hyperplasia can be a side effect of vaginal estrogen treatment. (45,46) The authors indicate that they do not have any conflicts of interest. Sources of funding: none reported.
Members of various medical faculties develop articles for "Practical Therapeutics." This article is one in a series coordinated by the Department of Family and Preventive Medicine at Emory University School of Medicine, Atlanta. Guest editor of the series is Timothy L. Clenney, M.D.
REFERENCES
(1.) Kent HL. Epidemiology of vaginitis. Am J Obstet Gynecol 1991;165(4 pt 2):1168-76.
(2.) Schaaf VM, Perez-Stable E, Borchardt K. The limited value of symptoms and signs in the diagnosis of vaginal infections. Arch Intern Med 1990;150:1929-33.
(3.) Bornstein J, Lakovsky Y, Lavi I, Bar-Am A, Abramovici H. The classic approach to diagnosis of vulvovaginitis: a critical analysis. Infect Dis Obstet Gynecol 2001;9:105-11.
(4.) Amsel R, Totten PA, Spiegel CA, Chen KC, Eschenbach D, Holmes KK. Nonspecific vaginitis. Diagnostic criteria and microbial and epidemiologic associations. Am J Med 1983;74:14-22.
(5.) Lurie S, Woliovitch I, Rotmensch S, Sadan O, Glezerman M. Value of vaginal culture in management of acute vaginitis. Arch Gynecol Obstet 2001;265:187-9.
(6.) Blake DR, Duggan A, Quinn T, Zenilman J, Joffe A. Evaluation of vaginal infections in adolescent women: can it be done without a speculum? Pediatrics 1998;102:939-44.
(7.) Sobel JD. Vaginitis. N Engl J Med 1997;337:1896-903. 8. Egan ME, Lipsky MS. Diagnosis of vaginitis. Am Fam Physician 2000;62:1095-104.
(9.) Sobel J. Bacterial vaginosis. Annu Rev Med 2000;51:349-56.
(10.) Sexually transmitted diseases treatment guideline 2002. Centers for Disease Control and Prevention MMWR Recomm Rep 2000;51(RR-6):1-80. Accessed online June 28, 2004, at: http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5106a1.htm.
(11.) Hanson JM, McGregor JA, Hillier SL, Eschenbach DA, Kreutner AK, Galask RP, et al. Metronidazole for bacterial vaginosis. A comparison of vaginal gel vs. oral therapy. J Reprod Med 2000;45:889-96.
(12.) Mikamo H, Kawazoe K, Izumi K, Watanabe K, Ueno K, Tamaya T. Comparative study on vaginal or oral treatment of bacterial vaginosis. Chemotherapy 1997;43:60-8.
(13.) Fischbach F, Petersen EE, Weissenbacher ER, Martius J, Hosmann J, Mayer H. Efficacy of clindamycin vaginal cream versus oral metronidazole in the treatment of bacterial vaginosis. Obstet Gynecol 1993;82:405-10.
(14.) Schmitt C, Sobel JD, Meriwether C. Bacterial vaginosis: treatment with clindamycin cream versus oral metronidazole. Obstet Gynecol 1992;79:1020-3.
(15.) Ferris D, Litaker M, Woodward L, Mathis D, Hendrich J. Treatment of bacterial vaginosis: a comparison of oral metronidazole, metronidazole vaginal gel, and clindamycin vaginal cream. J Fam Pract 1995;41:443-9.
(16.) Ahmed-Jushuf I, Shahmanesh M, Arya OP. The treatment of bacterial vaginosis with a 3 day course of 2% clindamycin cream: results of a multicenter, double blind, placebo controlled trial. B V Investigators Group. Genitourin Med 1995;71:254-6.
(17.) French JI, McGregor JA, Draper D, Parker R, McFee J. Gestational bleeding, bacterial vaginosis, and common reproductive tract infections: risk for preterm birth and benefit of treatment. Obstet Gynecol 1999;93(5 pt 1):715-24.
(18.) McDonald HM, O'Loughlin JA, Vigneswaran R, Jolley PT, Harvey JA, Bof A, et al. Impact of metronidazole therapy on preterm birth in women with bacterial vaginosis flora (Gardnerella vaginalis): a randomised, placebo-controlled trial. Br J Obstet Gynaecol 1997;104:1391-7.
(19.) Kekki M, Kurki T, Pelkonen J, Kurkinen-Raty M, Cacciatore B, Paavonen J. Vaginal clindamycin in preventing preterm birth and peripartal infections in asymptomatic women with bacterial vaginosis: a randomized, con-trolled trial. Obstet Gynecol 2001;97(5 pt 1):643-8.
(20.) Duff P, Lee ML, Hillier SL, Herd LM, Krohn MA, Eschenbach DA. Amoxicillin treatment of bacterial vaginosis during pregnancy. Obstet Gynecol 1991;77:431-5.
(21.) McDonald H, Brocklehurst P, Parsons J, Vigneswaran R. Antibiotics for treating bacterial vaginosis during pregnancy. Cochrane Database Syst Rev 2004;(1):CD000262.
(22.) American College of Obstetricians and Gynecologists. ACOG Practice Bulletin. Assessment of risk factors for pre-term birth. Clinical management guidelines for obstetrician-gynecologists. Number 31, October 2001 (Replaces Technical Bulletin number 206, June 1995; Committee Opinion number 172, May 1996; Committee Opinion number 187, September 1997; Committee Opinion num-ber 198, February 1998; and Committee Opinion number 251, January 2001). Obstet Gynecol 2001;98:709-16.
(23.) Screening for bacterial vaginosis: recommendations and rationale. Rockville, Md.: Agency for Healthcare Research and Quality. Accessed March 19, 2004, at: http://www3.ahcpr.gov/clinic/ajpmsuppl/bvrr.htm.
(24.) Ugwumadu A, Manyonda I, Reid F, Hay P. Effect of early oral clindamycin on late miscarriage and preterm deliv-ery in asymptomatic women with abnormal vaginal flora and bacterial vaginosis: a randomised controlled trial. Lancet 2003;361:983-8.
(25.) Caro-Paton T, Carvajal A, Martin de Diego I, Martin-Arias LH, Alvarez Requejo A, Rodriguez Pinilla E. Is metronidazole teratogenic? A meta-analysis. Br J Clin Pharmacol 1997;44:179-82.
(26.) Hallen A, Jarstrand C, Pahlson C. Treatment of bacterial vaginosis with lactobacilli. Sex Transm Dis 1992;19:146-8.
(27.) Reid G, Bruce AW, Fraser N, Heinemann C, Owen J, Henning B. Oral probiotics can resolve urogenital infec-tions. FEMS Immunol Med Microbiol 2001;30:49-52.
(28.) Sobel JD, Faro S, Force RW, Foxman B, Ledger WJ, Nyirjesy PR, et al. Vulvovaginal candidiasis: epidemiologic, diagnostic, and therapeutic considerations. Am J Obstet Gynecol 1998;178:203-11.
(29.) Eckert LO, Hawes SE, Stevens CE, Koutsky LA, Eschenbach DA, Holmes KK. Vulvovaginal candidiasis: clinical manifestations, risk factors, management algorithm. Obstet Gynecol 1998;92:757-65.
(30.) Ferris DG, Nyirjesy P, Sobel JD, Soper D, Pavleti c A, Litaker MS. Over-the-counter antifungal drug misuse associated with patient-diagnosed vulvovaginal candi-diasis. Obstet Gynecol 2002;99:419-25.
(31.) Sobel JD, Brooker D, Stein GE, Thomason JL, Wermeling DP, Bradley B, et al. Single oral dose fluconazole com-pared with conventional clotrimazole topical therapy of Candida vaginitis. Fluconazole Vaginitis Study Group. Am J Obstet Gynecol 1995;172(4 pt 1):1263-8.
(32.) Sobel JD, Kapernick PS, Zervos M, Reed BD, Hooton T, Soper D, et al. Treatment of complicated Candida vaginitis: comparison of single and sequential doses of fluconazole. Am J Obstet Gynecol 2001;185:363-9.
(33.) Stein GE, Christensen S, Mummaw N. Comparative study of fluconazole and clotrimazole in the treatment of vulvovaginal candidiasis. DICP 1991;25:582-5.
(34.) Haefner HK. Current evaluation and management of vulvovaginitis. Clin Obstet Gynecol 1999;42:184-95.
(35.) Sobel JD. Recurrent vulvovaginal candidiasis (RVVC). Int J STD AIDS 2001;12(suppl 2):9.
(36.) Krieger JN, Tam MR, Stevens CE, Nielsen IO, Hale J, Kiviat NB, et al. Diagnosis of trichomoniasis. Comparison of conventional wet-mount examination with cytologic studies, cultures, and monoclonal antibody staining of direct specimens. JAMA 1988;259:1223-7.
(37.) Patel SR, Wiese W, Patel SC, Ohl C, Byrd JC, Estrada CA. Systematic review of diagnostic tests for vaginal trichomoniasis. Infect Dis Obstet Gynecol 2000;8:248-57.
(38.) Forna F, Gulmezoglu AM. Interventions for treating trichomoniasis in women. Cochrane Database Syst Rev 2004;(1):CD000218.
(39.) Wiese W, Patel SR, Patel SC, Ohl CA, Estrada CA. A meta-analysis of the Papanicolaou smear and wet mount for the diagnosis of vaginal trichomoniasis. Am J Med 2000;108:301-8.
(40.) DuBouchet L, Spence MR, Rein MF, Danzig MR, McCor-mack WM. Multicenter comparison of clotrimazole vaginal tablets, oral metronidazole, and vaginal suppositories containing sulfanilamide, aminacrine hydro-chloride, and allantoin in the treatment of symptomatic trichomoniasis. Sex Transm Dis 1997;24:156-60.
(41.) Pearlman MD, Yashar C, Ernst S, Solomon W. An incremental dosing protocol for women with severe vaginal trichomoniasis and adverse reaction to metronidazole. Am J Obstet Gynecol 1996;174:934-6.
(42.) Sobel JD, Nyirjesy P, Brown W. Tinidazole therapy for metronidazole-resistant vaginal trichomoniasis. Clin Infect Dis 2001;33:1341-6.
(43.) Nyirjesy P, Sobel JD, Weitz MV, Leaman DJ, Gelone SP. Difficult-to-treat trichomoniasis: results with paromomycin cream. Clin Infect Dis 1998;26:986-8.
(44.) Klebanoff MA, Carey JC, Hauth JC, Hillier SL, Nugent RP, Thom EA, et al. Failure of metronidazole to prevent preterm delivery among pregnant women with asymptomatic Trichomonas vaginalis infection. N Engl J Med 2001;345:487-93.
(45.) Pandit L, Ouslander JG. Postmenopausal vaginal atrophy and atrophic vaginitis. Am J Med Sci 1997;314:228-31.
(46.) Handa VL, Bachus KE, Johnston WW, Robboy SJ, Ham-mond CB. Vaginal administration of low-dose conjugated estrogens: systemic absorption and effects on the endometrium. Obstet Gynecol 1994;84:215-8.
Although it is tempting to treat vaginal complaints empirically based on the patient's history alone, studies have demon-strated poor correlation between symptoms and the final diagnosis.
* Patient information: A handout on vaginitis, written by the authors of this article, is provided on page 2139.
The Authors
MARION K. OWEN, M.D., is in private family practice in Atlanta. She received her medical degree from the University of North Carolina at Chapel Hill School of Medicine and completed a family medicine residency at Emory University School of Medicine, Atlanta.
TIMOTHY L. CLENNEY, CDR, MC, USN, is a staff family physician in the family medicine residency program at the Naval Hospital Jacksonville (Fla.), as well as assistant professor of family medicine at the Uniformed Services University of the Health Sciences F. Edward Hebert School of Medicine, Bethesda, Md. Dr. Clenney received his medical degree from the University of South Florida College of Medicine, Tampa, and completed a family medicine residency at the Naval Hospital Jacksonville. He also completed a faculty development fellowship and a master of public health degree at Emory University.
Address correspondence to Timothy L. Clenney, CDR, MC, USN, 1705 Broad Water Ct., Orange Park, FL 32003 (e-mail: tclenney@msn.com). Reprints are not available from the authors.
COPYRIGHT 2004 American Academy of Family Physicians
COPYRIGHT 2004 Gale Group