Doctors, like other professional people, are expected to exercise proper care in their work. If they neglect to do so and their patients are harmed they can expect to be criticised. Over the past decade, this criticism has increasingly taken the form of civil action against the doctor by patients or their families who seek financial recompense. More rarely, a patient dies as a result of alleged negligence and the Crown Prosecution Service considers that a criminal charge of manslaughter is justified. Up to 1990 these cases were very rare. In 1970, Leahy Taylor wrote that it was "unlikely in the extreme" that any doctor would face a charge of criminal negligence.[1] He was aware of only two cases, those of Dr Percy Bateman, who had been convicted of manslaughter after an obstetric patient died, but was later pardoned on appeal,[2] and a Dr Wight, who had been sentenced to 3 months' imprisonment for performing a forceps delivery while he was under the influence of chloral hydrate, as a result of which the mother died. In 1867 a Dr Spencer was acquitted of manslaughter after a medication error in which strychnine was dispensed to a patient instead of bismuth.[3] This article focuses on errors in administering anaesthetics and in prescribing and giving medicines since these are the most common mistakes described in published reports.
Method
I examined the indexes of the Times (1971-89), the Guardian and the Observer (1990-9), the Daily Telegraph and Sunday Telegraph (1994-9), Medline (1966-October 1999), Embase (1980-October 1999), ISI Scientific database (1981-October 1999), and Justis (Weekly Law Reports, 1953-99) to identify cases of British doctors who had been charged with manslaughter between 1970 and 1999. I discovered 17 cases involving 21 doctors in which the outcome was known by December 1999--two cases involving two doctors in the periods 1970-9 and 1980-9 and 13 cases involving 17 doctors in 1990-9 (table).
The cases
Case 1--A locum anaesthetist was sent for trial for manslaughter on a coroner's warrant after an inquest into the death of a 9 year old boy during an appendectomy. The locum had used a thin walled nasotracheal tube, but had passed it through the mouth into the trachea and then secured a loose connection with sticking plaster. The thin walled tube had kinked under the sticking plaster. Alter about 10 minutes the boy was noticed to be blue, and he subsequently died. The doctor was convicted.[4]
Case 2--A 4 year old boy who had had a brain tumour removed had been given 650 mg of methotrexate "into the brain," developed convulsions, and subsequently died. The dose of methotrexate was 20 times too great. The junior doctor who had given the injection had taken the dosage from the case notes, "not knowing that it related only to intravenous drips." (The circulating blood volume is about 20 times the volume of cerebrospinal fluid.) The doctor was charged with manslaughter but was acquitted.[5]
Case 3--A 42 year old man became agitated during a private procedure to treat warts and the doctor gave him an injection of "diazepam." The patient collapsed, was taken to hospital, and later died. A blood sample taken in hospital showed that he had been given methohexitone, a short acting barbiturate anaesthetic, and not diazepam. The doctor was charged with manslaughter, and the prosecution alleged that he had intended, by himself, to anaesthetise the patient with methohexitone. The doctor pleaded that he had been befuddled because of a painkilling injection given to him for an injury he had sustained earlier that day and that the patient had been angry when he had suggested cancelling the operation. He was acquitted.[6]
Case 4--A 33 year old man was admitted to intensive care after surgery. When he became hypotensive, he was prescribed intravenous dopamine, but because the infusion was unregulated and rapid he developed severe tachycardia. The man was given verapamil and then a [Beta] adrenoceptor antagonist--a combination that is known to cause complete heart block. The patient had a cardiac arrest and died, and his medical records were subsequently altered. The locum doctor involved was charged under the Forgery and Counterfeiting Act 1981 and also with unlawful killing. However, the unlawful killing charge was abandoned before the trial.[7]
Case 5--A 33 year old man died six months after he had had a cardiac arrest during surgery for a retinal detachment. The cardiac arrest was caused by the hypoxia which occurred when the patient's endotracheal tube became disconnected from the oxygen supply. The locum anaesthetist noticed a problem only when a blood pressure alarm sounded some four and a half minutes after disconnection. At first he believed the blood pressure machine was faulty; however, one of the surgeons recognised bradycardia, cyanosis, and the disconnected endotracheal tube. The anaesthetist was charged with manslaughter. One expert described the standard of care as abysmal and another said that the doctor's conduct amounted to a gross dereliction of care. The anaesthetist argued that; though he was negligent, his acts were not so grossly negligent as to justify a verdict of manslaughter. He was convicted and subsequent appeals were unsuccessful.[8]
Case 6--A 55 year old woman died during general anaesthesia for endoscopic examination of the larynx, pharynx, and oesophagus. A fine bore "microlaryngeal" tube had been connected directly to an oxygen cylinder and not to a ventilator. The woman received over 1000 litres of oxygen within a few minutes, and she inflated "to resemble a Michelin man of the tyre advertisements." The locum anaesthetist supervising the woman's management was convicted of manslaughter and was sentenced to six months' imprisonment, suspended for 18 months.[9]
Case 7--A 23 year old prisoner was transferred to a cell at a provincial police station, having spent eight weeks on remand elsewhere. During that time he had been weaned off heroin, and on transfer was regarded as "fit and healthy." The young man was seen separately by two police surgeons who, over the next 11 days, prescribed temazepam (160 mg at night), diazepam (80 mg daily), chlorpromazine (300 mg daily), co-proxamol (two tablets daily), and methadone (30 mg daily). "He was changed into a zombie-like figure, staggering about, unsteady on his feet, with his eyes glazed." The young man was taken to hospital, assessed, and discharged back into custody, but he was found collapsed the next morning and died in hospital shortly afterwards. The police surgeons were charged with manslaughter and were convicted, but one was acquitted on appeal.[10]
Case 8--A 16 year old boy with leukaemia was receiving chemotherapy with intravenous vincristine and intrathecal methotrexate after a relapse. A lumbar puncture was performed and a junior doctor passed two syringes to his colleague. The contents of both syringes were injected intrathecally without being checked. It was subsequently realised that the patient had been given intrathecal vincristine, and an attempt was made to lavage the theca through a cisternal needle. This punctured the brain stem and the boy died. The two doctors were convicted of manslaughter. At the trial the judge said, "You are far from being bad men. You are good men who ... were guilty of a momentary recklessness." The conviction was quashed on appeal because the trial judge had not directed the jury to consider whether each doctor was grossly negligent, taking into account the possible excuses and mitigating circumstances.[11]
Case 9--A 1 year old girl collapsed during an insulin stress test of pituitary function and was then given so much glucose solution that she developed cerebral oedema and died. A junior doctor and a consultant paediatrician were charged with manslaughter more than two and a half years later. The case was abandoned by the prosecution at the committal proceedings.[12]
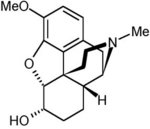
Case 10-A general practitioner performed circumcisions on four boys in his surgery and administered diamorphine to them as a sedative. One 9 year old boy remained unconscious and when he was eventually taken to hospital he was found to have suffered irreversible brain damage from which he died. The doctor at first claimed he had given the boy dihydrocodeine. He pleaded guilty to manslaughter, having used "excessive amounts of these drugs, and it was accepted that they were wholly inappropriate as sedatives." The doctor was sentenced to 12 months in prison, suspended for 12 months.[13]
Case 11--A 30 year old woman with asthma went to see her general practitioner because she was experiencing palpitation. He prescribed a [Beta] adrenoceptor antagonist. She collapsed and died hours after taking the first tablet. The general practitioner subsequently tried to erase all mention of asthma from the patient's records and the practice computer, but evidence remained in the computer's memory. The doctor was charged with manslaughter and with attempting to pervert the course of justice. He was acquitted of the first charge but convicted on the second.[14]
Case 12--A 36 year old man with an intracerebral drainage tube and an intravenous cannula died after he had been given penicillin intracerebrally rather than intravenously as prescribed. The junior doctor responsible, who had worked 110 hours in the previous week and had been on duty for 14 hours, was charged with manslaughter but acquitted. The patient's widow later said, "He had paid the price for the long hours demanded from untrained doctors."[15]
Case 13--A 41 year old woman with severe migraine was seen by a deputising general practitioner who gave her prochlorperazine and diazepam. These drugs stopped her vomiting but did not relieve her pain. Her husband, a consultant surgeon, suggested an injection of pethidine, which the general practitioner went to fetch from a local pharmacy. Because the pharmacy had no pethidine, the general practitioner obtained an ampoule of diamorphine containing 100 mg and administered the whole dose intramuscularly. The dosage was reasonable for pethidine, but it was 10 was times too high for diamorphine. The woman went to sleep and was dead within an hour. The doctor was charged with manslaughter as "administering that amount of drug amounted to gross negligence." He was convicted and was sentenced to 12 months' imprisonment, suspended for two years.[16]
Case 14--A 22 year old heroin addict in police custody was prescribed methadone by a police surgeon and subsequently died. The doctor was alleged to have given a "lethal dose of methadone" and was charged with manslaughter. The doctor was too ill to stand trial, but the judge ordered that the charge lie on the file.[17]
Case 15--An anaesthetist was sentenced to six months' imprisonment in July 1999 for the manslaughter of a 14 year old boy with Goldenhar's syndrome whom he had anaesthetised in a dentist's surgery. The boy had been given nitrous oxide instead of oxygen postoperatively because the tubing was wrongly connected, and the doctor admitted failing to check the equipment. The abnormalities associated with Goldenhar's syndrome (including mandibular and maxillary hypoplasia and malformation of the tongue) made resuscitation more difficult, but neither the anaesthetist nor the dentist had obtained the patient's medical history. The judge stated, "This offence was one of the most gross negligence."[18]
Case 16--A 12 year old boy with T cell non-Hodgkin's lymphoma was due to have intravenous vincristine and intrathecal methotrexate which had been prescribed by a specialist registrar in paediatric haematology. Because the paediatric oncology ward was full, the boy was admitted to a general paediatric ward. He was scheduled to have lumbar puncture under anaesthesia during the day, but because he ate a biscuit the procedure had to be postponed until the evening, when it was left to a specialist registrar in paediatric anaesthesia. The registrar had never given intrathecal cytotoxic treatment before, but had discussed it by telephone with his haematological colleague. A nurse, unaware of a hospital rule that vincristine should never be taken into theatre, provided the anaesthetist with two syringes, one containing vincristine and bearing a label that read "only for IV use." The anaesthetist did not read the label, and administered the vincristine intrathecally. The boy developed an increasingly painful arachnoiditis, which was diagnosed only two days after the episode, and he subsequently died. The prosecution's expert at first maintained that the doctors' conduct had fallen "seriously and significantly" below the expected standard, and both registrars were committed for trial on a charge of manslaughter. However, before trial in the crown court more information was made available to the expert, who realised that "significant system failures within the hospital administration" were important factors in the boy's death, and the crown offered no evidence. The doctors were acquitted.[19 20]
Case 17--A state enrolled nurse gave 300 mg morphine which had been prescribed for one patient who was dying from cancer to another patient in an adjoining room at a nursing home. The 77 year old recipient was bed bound with severe emphysema and pneumoconiosis. A general practitioner advised careful observations. About 11 hours after he had been given the morphine, the man was found collapsed and in coma. An ambulance was summoned, the paramedic crew gave naloxone, and the patient recovered consciousness and was taken to hospital, but he had a further seizure and died. The general practitioner and three nurses were charged with manslaughter. The judge ruled that as the patient was subsequently revived there was no evidence that any omission by the general practitioner or the last nurse had contributed materially to his death and they were acquitted. The other nurses were acquitted subsequently.[21]
Discussion
Doctors can be convicted of manslaughter if someone dies as a result of their gross negligence. Gross negligence is defined as negligence occurring when there is a wholly irresponsible disregard of a serious risk to others, of which the defendant is aware or "to which he made himself wilfully blind."[11] The jury has to decide whether, taking into account the risk of death involved, the defendant's conduct was so bad that it must have been criminal.
Changing incidence
Seventeen doctors were charged with manslaughter in the 1990s, compared with two in each of the preceding two decades. However, a true eightfold increase in gross negligence seems unlikely as civil negligence cases only doubled between 1990 and 1998.[22] More plausible explanations are a greater readiness to call the police or to prosecute, perhaps because the Crown Prosecution Service perceives that juries are readier to convict nowadays.
Background to medical errors
Medical errors are suddenly consequential. The US Institute of Medicine and the UK Department of Health have recently published important position statements,[20 23] and the BMJ devoted a special issue to the subject (18 March 2000). The Institute of Medicine's view is clear: "The problem is not bad people; the problem is that the system [of medical care] needs to be made safer."[23] According to the Department of Health's expert group, "In the great majority of cases, the causes of serious failures stretch far beyond the actions of the individuals immediately involved."[20] However, it includes the rider that individuals must be held to account, "in particular if there is evidence of gross negligence or recklessness, or of criminal behaviour."[20]
The system of medical care, like all other systems, is safe only if human error is recognised as inevitable and the system is designed to minimise the consequences. An error is a failure to perform an action as intended. Errors can arise in planning actions or in executing them. Errors in planning actions are technically known as mistakes.[24] They arise particularly when a task is unfamiliar or where there is insufficient information to formulate an analytical solution (J T Reason, Reducing error in health care, BMA/BMJ conference, London, 21 March 2000). Proper education and supervision should reduce the incidence of mistakes. Errors in executing tasks are called slips, and those due to failure of memory are defined as lapses. When we are faced with familiar tasks, like preparing a cup of tea, or prescribing a commonly used drug, we perform them rapidly and automatically. But the automatic processes can be derailed. An example of an automatic process is writing the date--a process that is often in error each January. Slips and lapses are more likely in the presence of tiredness, interruptions, and distraction by competing tasks, all of which are inevitable in medical practice. Systems can be changed and structural alterations carried out to make them safer--for example, the number of safety checks can be increased and all potassium chloride strong solution moved from clinical areas to a locked pharmacy store.
It is sometimes difficult or impossible to categorise errors. In this series, mistakes were primarily responsible for seven deaths and slips or lapses for nine; one death could not be assessed (table).
Doctors accused of manslaughter after deaths due to errors in drug treatment or anaesthesia, United Kingdom 1970-99
(*) Where stated.
([dagger]) Classified as mistakes (errors in planning an action) and slips (errors in its execution).
Does convicting doctors help?
Doctors who are evil or who abuse alcohol or drugs and who kill patients as a result should clearly face prosecution. For most errors, though, the criminal law is unsatistactory. Convicting doctors of manslaughter may satisfy a desire for retribution, but deters careful consideration of the ways of preventing tragedies from recurring. Police investigation has three advantages: it is professional, independent, and treated with the utmost seriousness. An independent investigative body, perhaps related to the Commission for Health Improvement, that can inquire into fatal medical errors and make its findings public would have those advantages, while being able to examine issues of system failure, and make informed recommendations on strategies to prevent recurrence. It would supplement the work of coroners, who might be well placed to refer cases to it.
The Department of Health's expert group recommends a unified mechanism for reporting and analysing errors in medical care, a "more open culture in which errors or service failures can be reported and discussed," and a "much wider appreciation of the value of the systems approach in preventing, analysing and learning from errors." This is entirely reasonable, but we also need an independent investigative body whose remit is to safeguard patients and which can marshal the expertise necessary to analyse failures in complex systems. Patients and doctors would be safer if an independent inquiry were guaranteed, and the criminal law could be reserved for those doctors who show "such disregard for life and safety as to amount to a crime against the state."[2]
[Figures 1-2 ILLUSTRATION OMITTED]
Summary points
If a doctor is grossly negligent and the patient dies as a result, the doctor can be charged with manslaughter
The numbers of doctors charged with and convicted of manslaughter have increased appreciably in the past decade
Blaming one or a few people for an error that may be the result of difficulties at many stages in a complex process is dangerous
This action encourages secrecy and inhibits system changes that would reduce the likelihood of future errors
I am most grateful to colleagues who were kind enough to discuss their own experiences with me.
Funding: None.
Competing interests: REF has received fees for writing medicolegal reports.
[1] Leahy Taylor J. The doctor and the law. London: Pitman Medical and Scientific, 1970.
[2] Medico-legal. Rex v Bateman. BMJ 1925;i:1022-3.
[3] Dyer C. Coroners and manslaughter. BMJ 1975;iii:108-9.
[4] Doctor sent for trial on coroner's warrant. Times 1974 October 31:4.
[5] Doctor cleared over boy's drug death. Times 1978 April 28:4.
[6] Doctor accused of killing by overdose. Times 1982 July 7:3;July 15:4.
[7] Doctor charged. Times 1986 December 5:2.
[8] Regina respondent and Adomako appellant. Appeal Cases [House of Lords] 1995;1:171-90.
[9] Anaesthetist convicted of manslaughter. Guardian 1990 July 31:6.
[10] Nelson-Jones R, Burton F. Medical negligence case law. London: Butterworths, 1995:511-3a.
[11] Reg v Prentice. Queen's Bench Law Reports [Court of Appeal] 1994:311.
[12] Halle M. Doctors charged over child death. Observer 1994 February 13:7.
[13] Doctor admits killing. Guardian 1994 March 4:3.
[14] Doctor jailed for attempting to cover up fatal error. Guardian 1994 May 7:8.
[15] Doctor charged over death. Guardian 1995 March 7:2.
[16] Stokes P. Suspended jail term for doctor in lethal injection case. Daily telegraph 1998 November 28. www.telegraph.co.uk:80/et?&pg=/et/98/11/ 28/ndoc28.html (accessed 30 Aug 2000).
[17] Stokes P. Surgeon too ill to stand trial. Daily Telegraph 1999 March 17. www.telegraph.co.uk:80/et?&pg=/et/99/3/17/nsur17.html (accessed 30 Aug 2000).
[18] Anaesthetist jailed over death. Daily Telegraph 1999 July 30. www.telegraph.co.uk:80/et?&pg=/et/99/7/30/nbu130.html#go3 (accessed 30 Aug 2000).
[19] Clough S. Doctors cleared of killing boy, 12, in cancer jab mix-up. Daily Telegraph 1999 January 6.www.telegraph.co.uk:80/et?&pg=/et/99/1/6/ nkid06.html (accessed 30 Aug 2000).
[20] An organization with memory. Report of an expert group on learning from adverse events in the NHS chaired by the chief medical officer. Norwich. London: Stationery Office, 2000. www.doh.gov.uk/orgmemreport/index.htm (accessed 12 July 2000.)
[21] Stokes P. Patient `died after nurse's morphine tablet blunder.' Daily Telegraph 1999 Oct 5. www.telegraph.co.uk:80/et?&pg=/et/99/10/5/ nmorp05.html (accessed 30 Aug 2000).
[22] Fenn P, Diacon S, Gray A, Hodges R, Rickman N. Current cost of medical negligence in NHS hospitals: analysis of claims database. BMJ 2000;320:1567-71.
[23] Kohn LT, Corrigan JM, Donaldson MS, eds. To err is human:building a safer health system. Washington: National Academy Press, 1999. www.nap.edu/ books/0309068371/html/ (accessed 20 Aug 2000.)
[24] Reason JT. Human error. Cambridge: Cambridge University Press, 1990.
(Accepted 24 July 2000)
West Midlands Centre for Adverse Drug Reaction Reporting, City Hospital, Birmingham B18 7QH
R E Ferner director
r.e.ferner@bham. ac.uk
BMJ 2000;321:1212-6
COPYRIGHT 2000 British Medical Association
COPYRIGHT 2001 Gale Group