Background: There are conflicting reports on the effects of diltiazem treatment on renal function in surgical patients. We sought to determine whether diltiazem treatment alters renal function in patients undergoing major thoracic surgery.
Methods: In a prospective study, 330 patients scheduled for elective thoracic surgery received either IV diltiazem (n = 167) or placebo (n = 163) immediately after the operation and orally thereafter for 14 days in an effort to prevent postoperative atrial arrhythmias. Serum creatinine and BUN levels were compared before and during the first postoperative week.
Results: Patients treated with diltiazem were similar to control subjects in terms of age (mean [+ or -] SD, 66 [+ or -] 10 years vs 67 [+ or -] 10 years, respectively), baseline serum creatinine or BUN levels, prevalence of comorbid conditions, and surgical characteristics. During the first 5 postoperative days, the two groups did not differ in terms of serum creatinine or BUN levels. The incidence of renal failure was 0.6% in the diltiazem group and 1.2% in the placebo group (difference was not significant). There was no difference in the length of hospitalization or mortality rate.
Conclusions: In patients without renal disease who are undergoing elective thoracic surgery, prophylactic diltiazem treatment did not alter postoperative renal function. (CHEST 2001; 119:1476-1479)
Key words: diltiazem; renal function; surgery
Abbreviation: GFR = glomerular filtration rate
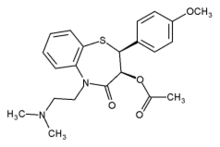
Atrial arrhythmias after cardiothoracic operations are responsible for increased morbidity and resource utilization.[1,2] Diltiazem treatment has been reported to reduce atrial arrhythmias after cardiac[3] and noncardiac thoracic surgery,[4,5] to prevent vasospasm of peripheral arterial conduits used for coronary artery bypass grafting,[6] and to reduce the incidence of acute tubular necrosis after renal transplantation.[7] A retrospective study reported that the administration of IV diltiazem after cardiac operations was associated with a greater incidence of postoperative renal dysfunction.[8] In this study, we determined prospectively whether prophylactic diltiazem treatment alters renal function in a large group of patients undergoing thoracic operations.
MATERIALS AND METHODS
This study was approved by the Institutional Review Board of Memorial Sloan-Kettering Cancer Center, and written informed consent was obtained from each patient before their operation. To be included in the study, patients' hearts had to be in sinus rhythm and the patients had to be at increased risk for developing postoperative arrhythmias, either because they were scheduled to undergo a pneumonectomy or were [is greater than] 60 years of age and scheduled to have a lobectomy. The 330 patients who underwent lobectomy (n = 232), pneumonectomy (n = 63), or extrapleural pneumonectomy (n = 35) were randomly allocated in a double-blind fashion in the immediate postoperative period to receive diltiazem or placebo in an effort to prevent atrial arrhythmias.[5]
Patients were excluded if they had a history of chronic atrial arrhythmias or second-degree atrioventricular block or were taking class I or class III antiarrhythmic drugs or calcium-channel blockers for ischemic heart disease. Patients who developed new signs of myocardial ischemia or infarction or who required inotropic support on arrival to the postanesthesia care unit were also excluded. Preoperative medications were continued until the time of surgery. Patients taking L-type calcium channel blockers for hypertension (n = 8) received other antihypertensive medications postoperatively as clinically indicated. [Beta]-Blockers were continued postoperatively to avoid withdrawal.
All patients were premedicated with midazolam and glycopyrrolate and received standard anesthetic management that consisted of isoflurane and nitrous oxide supplemented by IV fentanyl and morphine as needed. Intentional crystalloid restriction ([is less than] 25 mL/kg) during surgery was attempted in all patients. Resection was carried out using standard thoracotomy approaches in a manner designed to completely remove all neoplastic disease along with an ipsilateral mediastinal lymph node dissection. Intraoperative estimated blood loss was recorded. Postoperative pain relief was provided to all patients by the continuous administration of either epidural opioid (usually fentanyl) [n = 195] or IV opioid (usually morphine) patient-controlled analgesia (n = 135). All patients were monitored with two-channel Holter recorders for 72 to 96 h postoperatively. After an overnight stay in the postanesthesia care unit, patients were transferred to the thoracic surgical floor on the first postoperative day. Serum BUN and creatinine levels were obtained at baseline before surgery and on the mornings of postoperative days 1 to 5. Postoperative complications were recorded throughout the hospital stay. A research nurse monitored patients for complications as outpatients for 30 days and queried patients about intercurrent hospitalizations or emergency department visits. An investigator reviewed these medical records.
Patients were randomly assigned to receive either diltiazem or placebo with stratification based on the type of surgery (ie, lobectomy, pneumonectomy, or extrapleural pneumonectomy). The randomization of patients in permuted blocks was done between the Epidemiology and Biostatistics departments and the hospital pharmacy with sealed, opaque treatment-code envelopes. All clinical and study personnel were blinded to the study group assignments throughout the trial. Treated patients (n = 167) received an IV loading dose of diltiazem, 0.25 mg/kg (50 mL), given over 30 min, followed by 0.1 mg/kg/h (constituted as 1 mg/mL) IV for 18 to 24 h. Diltiazem was temporarily discontinued for systolic hypotension ([is less than] 80 mm Hg) or marked bradycardia ([is less than] 50 beats/min). Control patients (n = 163) received an IV placebo loading dose of 50 mL given over 30 min, followed by a placebo infusion at 0.1 mL/kg/h given over the first 18 to 24 h from arrival in the postanesthesia care unit. Starting in the morning of postoperative day 1, patients received either diltiazem sustained release, 120 mg, or placebo orally twice daily for a total of 14 days. Patients who could not take oral medication during the treatment period were temporarily switched to the IV route. Adjustments in the oral dose were made for patients weighing [is less than] 50 kg, for those who had a systolic BP of [is less than] 90 mm Hg, or for those showing other adverse effects from receiving diltiazem. Venous blood was drawn to determine plasma diltiazem levels on the morning of postoperative day 3 before receiving the morning dose. The plasma diltiazem concentration was determined by high-performance liquid chromatography with ultraviolet detection (Bioassay Laboratory; Houston, TX).
Statistical Analysis
All analyses were performed on an intention-to-treat basis, and all p values were two-tailed. A p value [is less than] 0.05 was considered to be significant. To determine the difference in patient and operative characteristics between the two treatment groups, all variables were examined by univariate analysis, Student's t test, and Fisher's Exact Test. Repeated measures analysis of variance was used to examine differences between groups in renal functions. Data are presented as the mean [+ or -] SD, unless otherwise indicated.
RESULTS
The two groups were well matched in age, gender distribution, comorbidity, and surgical data (Table 1). Plasma magnesium concentrations taken on postoperative day 3 were nearly identical in diltiazem-treated patients (1.57 [+ or -] 0.17 mEq/L) vs control subjects (1.56 [+ or -] 0.16 mEq/L; difference not significant) [normal concentration range, 1.4 to 2.2 mEq/L]. The two groups did not differ in BUN or creatinine levels at baseline or at any other time during the study period (Table 2). Two patients assigned to placebo treatment developed postoperative acute renal failure (creatinine level, [is greater than] 2.5 mg/dL) but did not require dialysis. Renal failure was attributed to prerenal causes exacerbating preoperative amphotericin nephrotoxicity in one patient and exposure to nonsteroidal anti-inflammatory analgesics in another patient.
The incidence of clinically significant atrial arrhythmias was 10% in diltiazem-treated patients and 19% in control subjects (p = 0.02).[5] Length of hospital stay did not differ Between patients assigned to diltiazem treatment compared to control subjects (8.9 [+ or -] 7.9 vs 8.7 [+ or -] 7.8 days, respectively; p = 0.82). The median length of hospital stay was 7 days for both groups. There was no significant difference in the incidence of postoperative complications between the two groups. The length of stay in the ICU did not differ between patients assigned to diltiazem treatment (8.0 [+ or -] 4.7 days; n = 7) as compared with patients assigned to placebo treatment (8.4 [+ or -] 4.8 days; n = 8; p = 0.88). The reasons for ICU admission were pneumonia (n = 8), ARDS (n = 3), atrial fibrillation/flutter (n = 2), and pulmonary embolism (n = 2). Death within 30 days of surgery occurred in three patients assigned to placebo treatment and in one patient assigned to diltiazem treatment (p = 0.37).
In no patient was there a precipitous drop in BP seen with any dose of diltiazem. Six patients receiving diltiazem and one receiving placebo required a transient interruption in therapy because of mild hypotension in the postoperative anesthesia care unit (p = 0.12). Two diltiazem-treated patients had an interruption of IV drug therapy for [is greater than] 12 h because of a borderline systolic BP but continued with their oral therapy. The oral dose of diltiazem was decreased in two patients whose sitting systolic BP was 90 to 100 mm Hg before discharge from the hospital. even patients refused to continue in the study within the first 48 h, and two patients elected to drop out after 7 days of treatment. Side effects potentially related to diltiazem included dyspepsia (one patient) and rash (one patient). The mean plasma diltiazem level determined on the morning of postoperative day 3 was 310 [+ or -] 164 ng/mL (range, 26 to 742 ng/mL; median, 283 ng/mL) and was within the reported therapeutic range (79 to 294 ng/mL).[9]
DISCUSSION
Our findings that diltiazem does not adversely affect postoperative renal function are consistent with other reports in the literature.[4,7,10,11] In our study, patients undergoing major noncardiac thoracic surgery without cardiopulmonary bypass were treated with intentional crystalloid restriction to minimize the chances of postoperative pulmonary edema. Despite these measures, diltiazem did not increase common indexes of renal dysfunction in the postoperative period and proved to be effective in reducing the incidence of,clinically significant arrhythmias.[5] Postoperative acute renal failure developed in two patients assigned to placebo treatment and was attributed to drug-related nephrotoxicity, which was exacerbated by our policy of restricting fluid administration. Our incidence of renal failure in control subjects (1.2%) or in the entire study population (0.6%) is considerably lower than that of 15% reported by Patel et al[12] in similar patients.
A 1998 study compared patients who were administered diltiazem for 24 h after cardiac operations (n = 271) to similar patients not receiving diltiazem after surgery (n = 143), and the results showed that the use of diltiazem was associated with acute renal failure requiring dialysis in 12 of 271 patients (4.4%) compared with 1 of 143 control subjects (0.7%).8 The limitations of this retrospective report are primarily the lack of randomization for treatment and the disproportionately small sample size of the control group. In addition, a loading dose of diltiazem was not employed, and plasma diltiazem concentrations were not determined. In contrast, Zanardo et al[10] prospectively studied 35 patients undergoing coronary artery bypass grafting and found that patients randomized to receive diltiazem had a higher glomerular filtration rate (GFR) during and after cardiopulmonary bypass when compared to control subjects. In a similar group of patients, Amano et al[11] compared the effects of diltiazem with no treatment on perioperative renal function, plasma atrial natriuretic peptide level, and the renin-angiotensin-aldosterone system. These workers also found that diltiazem had a beneficial effect on postoperative urine output, creatinine clearance, and free water clearance, despite a reflex activation of the renin-angiotensin-aldosterone system induced by peripheral vasodilatation.[11]
In patients undergoing cadaveric kidney transplantation, diltiazem was shown to reduce the incidence of postoperative acute tubular necrosis and to improve GFR in patients with primary graft function during the first postoperative week.[7] The proposed mechanisms for these protective effects were the ability of diltiazem to reduce the calcium influx into smooth vascular muscle cells during ischemia and to reduce the accumulation of harmful free radicals in the renal tubular system.[7] Others have shown that the primary effect of diltiazem on the kidney was to reduce renal vascular resistance and to increase renal blood flow, thus increasing GFR.[13,14]
In conclusion, the indications for the use of diltiazem in surgical[3-7] patients appear to be increasing. Diltiazem also has been recommended as an adjunct in the treatment of acute renal failure unrelated to surgery.[15] The bulk of evidence from prospective studies does not support the results of one retrospective study on the adverse effects of diltiazem treatment on postoperative renal function. In this double-blind study, diltiazem treatment did not alter postoperative renal function in patients undergoing major noncardiac thoracic surgery.
ACKNOWLEDGMENTS: We thank Ilana Ginsburg, RN, for data collection.
REFERENCES
[1] Mathew JP, Parks R, Savino JS, et al. Atrial fibrillation after coronary artery bypass graft surgery: predictors, outcomes, and resource utilization. JAMA 1996; 276:300-306
[2] Amar D, Roistacher N, Burt M, et al. Clinical and echocardiographic correlates of symptomatic tachydysrhythmias after non-cardiac thoracic surgery. Chest 1995; 108:349-354
[3] Seitelberger R, Hannes W, Gleichauf M, et al. Effects of diltiazem on perioperative ischemia, arrhythmias and myocardial function in patients undergoing elective coronary bypass grafting. J Thorac Cardiovasc Surg 1994; 107:811-821
[4] Amar D, Roistacher N, Burt M, et al. Effects of diltiazem versus digoxin on dysrhythmias and cardiac function after pneumonectomy. Ann Thorac Surg 1997; 63:1374-1382
[5] Amar D, Roistacher N, Rusch VW, et al. Effects of diltiazem prophylaxis on the incidence and clinical outcome of atrial arrhythmias after thoracic surgery. Thorac Cardiovasc Surg 2000; 120:790-798
[6] Brodman RF, Frame R, Camacho M, et al. Routine use of unilateral and bilateral radial arteries for coronary artery bypass graft surgery. J Am Coll Cardiol 1996; 28:959-963
[7] Wagner K, Albrecht S, Neumayer HH. Prevention of posttransplant acute tubular necrosis by the calcium antagonist diltiazem: a prospective randomized study. Am J Nephrol 1987; 7:287-291
[8] Young EW, Diab A, Kirsh MM. Intravenous diltiazem and acute renal failure after cardiac operations. Ann Thorac Surg 1998; 65:1316-1319
[9] Dias VC, Weir SJ, Ellenbogen KA. Pharmacokinetics and pharmacodynamics of intravenous diltiazem in patients with atrial fibrillation or atrial flutter. Circulation 1992; 86:1421-1428
[10] Zanardo G, Michielon P, Rosi P, et al. Effects of a continuous diltiazem infusion on renal function during cardiac surgery. J Cardiothorac Vasc Anesth 1993; 7:711-716
[11] Amano J, Suzuki A, Sunamori M, et al. Effect of calcium antagonist diltiazem on renal function in open heart surgery. Chest 1995; 107:1260-1265
[12] Patel RL, Townsend ER, Fountain SW. Elective pneumonectomy: factors associated with morbidity and operative mortality. Ann Thorac Surg 1992; 54:84-88
[13] Rodger L, Epstein M. Effects of calcium antagonists on renal hemodynamics. Am J Physiol 1985; 249:F619-F629
[14] Becker G, Witzke O, Baltes A, et al. Diltiazem minimizes tubular damage because of FK506-medicated nephrotoxicity after ischemia and reperfusion in rats. Transpl Immunol 1996; 4:68-71
[15] Conger JD. Interventions in clinical acute renal failure: what are the data? Am J Kidney Dis 1995; 26:565-576
(*) From the Department of Anesthesiology and Critical Care Medicine (Dr. Amar) and the Department of Clinical Laboratories (Dr. Fleisher), Memorial Sloan-Kettering Cancer Center, New York, NY.
Supported in part by a grant from the International Anesthesia Research Society.
Manuscript received July 6, 2000; revision accepted June 11, 2000.
Correspondence to: David Amar, MD, FCCP, Memorial Sloan-Kettering Cancer Center, 1275 York Ave, Room M-304, New York, NY 10021; e-mail: amard@mskcc.org
COPYRIGHT 2001 American College of Chest Physicians
COPYRIGHT 2001 Gale Group