ABSTRACT
MUGUNIERI, G.L. & MURILLA, G.A. 2003. Resistance to trypanocidal drugs-suggestions from field survey on drug use in Kwale district, Kenya. Onderstepoort Journal of Veterinary Research, 70: 29-36
A household survey was conducted in 21 villages of Kwale district, Kenya, to assess farmers' trypanocidal drug use characteristics for treatment of bovine trypanosomosis and their relationship to drug effectiveness. Descriptive statistical tools were used to summarize the farmers' drug use patterns. The chi-square test was the done to establish the relationship between proper drug use and recovery. The results indicate that the farmers had considerable knowledge about trypanocidal drugs with 82% (n = 65) having used these drugs within 6 months preceding the survey. Cases of incorrect drug use were reported. This study established that there was no significant relationship between correct drug use and recovery of the treated animals, suggesting the presence of drug resistance in Kwale district.
Keywords: Drug resistance, field survey, trypanocidal drugs
(ProQuest Information and Learning: ... denotes non-USASCII text omitted.)
INTRODUCTION
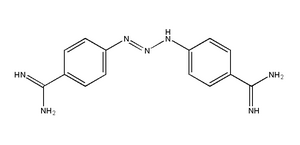
Treatment with trypanocidal drugs is the most widely used means of controlling bovine trypanosomosis in many parts of Africa where the disease is a constraint to development (Stevenson, Munga & Dolan 1993; ILRAD 1994). The drugs that are currently available are few and relatively expensive, and their widespread use has led to increased reports of drug failure (Dolan, Stevenson, Alushula & Okech 1985; ILRAD 1993). For the last 30 years, reliance has been placed on the use of three closely related compounds, i.e., isometamidium, homidium and diminazene. Resistance to these drug compounds has been detected in the laboratory, in vitro (Hirumi, Hirumi & Peregrine 1993; Kaminsky, Mamman, Chuma & Zweygarth 1993), in vivo (Codjia, Mulatu, Majiwa, Leak, Rowlands, Authie, D'lteren & Peregrine 1993; Joshua, Obwolo, Bwagamoi & Mandebvu 1995; Mulugeta, Wilkes, Mulatu, Majiwa, Masake & Peregrine 1997), by use of trypanocidal drug-ELISA (Eisler, Elliott & Holmes 1996; Murilla, Eisler, Peregrine, Ndung'u & Holmes 1999) and by use of longitudinal parasitological data (Rowlands, Mulatu, Authie, D'leteren, Leak, Nagda & Peregrine 1993). The findings of a study which preceded an investigation to establish the presence and extent of drug resistance through drug sensitivity testing in vivo of populations of Trypanosoma originating from cattle in Kwale district, Kenya, are summarized in this paper. This study was undertaken to determine the prevalence and frequency of use of trypanocidal drugs, drug use characteristics and their relationship to drug effectiveness as described by the farmers. The information generated, besides offering suggestions on presence of resistance to trypanocidal drugs, would be required when designing options for control of trypanosomosis in this area.
MATERIALS AND METHODS
Sampling
Kwale district is one of five districts in Coast Province of Kenya. Twenty-one villages were purposively selected covering all the farming systems within the district (Jaetzold & Schmidt 1983). Purposive sampling of villages was done so as to capture the spatial diversity in farming systems within this district. A list of all farmers rearing cattle in the selected villages was then complied during a survey where cattle were sampled for the presence of trypanosome parasites, using the standardized protocols for the microhaematocrit centrifugation-buffy coat technique, and thick and film blood smears (Woo 1969).
In this survey, 950 cattle belonging to 650 farmers were sampled for trypanosomes. Serum samples were collected for quantitative measurement of trypanocidal drug concentration using ELISAs for isometamidium (Eisler et al. 1996). Positive sera were sub-inoculated in irradiated mice in the field for subsequent in vivo drug sensitivity testing.
A total of 65 farmers, representing 10% of those who presented their cattle for trypanosome screening, were then selected from across all the villages with probability proportional to size. This two-stage sampling is self-weighting, making the estimation of means, totals, ratios and proportions straightforward (Poate & Daplyn 1993). The farmers were requested to complete a questionnaire, which was supervised by the authors together with a member of staff from the local veterinary investigation laboratories.
Assessment of prevalence, knowledge, and use of trypanocidal drugs
Open-ended questions were prepared in English, translated in Kiswahili, and then pre-tested and revised. The survey was conducted in November 1998 and the resulting data coded and analyzed.
Questions were asked on:
* Prevalence of use of trypanocidal drugs
* Details on the use of trypanocidal drugs. These included purpose of use (curative or prophylactic), description of frequency of use, and details on preparation, method of administration and dosage rate
* Farmers' perception on the effectiveness of the drugs used.
Use of trypanocidal drugs
The major question to be answered was whether a farmer used trypanocidal drugs when trypanosomosis was noted in the herd. In order to know the extent of drug use vis a vis infection levels, it was important to determine the following:
* The number of farmers who identified trypanosomosis in their herds either personally or with the assistance of an animal health assistant
* The number of farmers who took steps to treat their animals upon discovery of infection. This was for all diseases identified by the farmer in the 6 months preceding the survey (Six months was selected so as to capture more accurate recalls. This period also coincided with the beginning of the long rain period and provided a good point of reference).
* The number of animals infected and treated or not treated in the six months
* The person who administered the treatment.
In self-identification of trypanosomosis the approach was to understand farmers' perception of the main clinical signs of trypanosomosis and then relate this to modern veterinary knowledge. The farmers were requested to identify all diseases they had experienced in their herds by local names and by describing their clinical signs.
They were further requested to identify the vector of each of the diseases and the likely habitat for this vector. From this description, the authors, together with local veterinary field staff inferred the disease names in English. This approach was to enable the authors to understand how farmers characterize trypanosomosis in comparison to other common diseases endemic in the area (used as control diseases), mainly foot-and-mouth disease (FMD), East Coast fever (ECF) and anaplasmosis. The use of control diseases in identification of trypanosomosis was intended to avoid exaggeration of responses to trypanosomosis.
Knowledge on trypanocidal drugs
The next step was to establish whether farmers knew the drugs they used by name and whether the drugs used were administered correctly or not. Proper use of drugs entailed their preparation (water to drug ratio), administration (intra-muscular injection) and dosage rate. Farmers were requested to describe in detail all the steps they undertook in the preparation of the drugs and the subsequent administration and dosage. Questions were also posed to determine whether the treated animals recovered or not. Farmers who reported non-recovery were requested to give their opinion on what could have been the cause.
Is there resistance to trypanocidal drugs in Kwale district?-the chi-square analysis
The relationship between the recovery of animals after treatment and the procedure of treatment, i.e. correct or incorrect treatment procedure was investigated. Animals treated were reported either to have recovered or not. The idea was to investigate if there is a relationship between recovery and proper drug use. Lack of a significant relationship between recovery and proper drug use could mean that there is a possibility of there being resistance to the drugs. The chi-square test was used to establish this relationship.
RESULTS AND DISCUSSION
Prevalence of trypanosomosis and use of trypanocidal drugs
From the data collected, 91% of the farmers correctly linked the main clinical signs of trypanosomosis-like disease to trypanosomosis infection and associated this to tsetse flies as the vector. Furthermore, they correctly described the likely habitat of this vector. These farmers were therefore classified as being able to identify trypanosomosis in their herds. Ninety-two percent of the farmers reported to have experienced these trypanosomosis-like clinical signs in their herds, indicating that most of the farmers had considerable knowledge about the disease. Ninety-six percent of the farmers reported to have undertaken measures to treat the disease. Of those who treated their animals, 62% undertook the treatment by themselves, 27% sought the services of trained animal health personnel and 11% called either their neighbour or friend whom they believed had knowledge in administering of the drugs.
Farmers associated trypanosomosis with weight loss, abortion, reduced appetite, diarrhoea, coughing and loss of tail hair, and with the licking of sand or soil. If an animal died, it was reported to have a "watery" (oedematous) carcass.
Further questioning about the signs showed that farmers also noted swollen lymph nodes and a staring coat. On the aetiology, they thought that trypanosomosis was caused by tsetse flies. Haemorraghic trypanosomosis was characterized by rapid onset and short duration, diarrhoea, abortion and death. After death, a "bloody carcass" was observed with bleeding from internal organs. However, other diseases such as anthrax might cause similar disease signs. Anthrax was ruled out as a possibility since the veterinary investigation laboratories had not encountered any cases of the disease in the area during the study period.
Apart from coughing, these clinical signs are indicative of trypanosomosis. It should be noted that in trying to identify trypanosomosis, common endemic diseases were selected for comparison of disease-signs and disease-causes. This aspect of the methodology was intended to highlight differences between the other important diseases in the area in order to limit exaggeration concerning the specific interests of researchers. Further, to facilitate correct interpretation of the diseases being described by the farmer, the authors worked together with the local animal health and veterinary investigation laboratories staff in the questionnaire administration. Loss of hair is rarely cited in veterinary books as a sign of trypanosomosis. However, this sign is widely reported in the ethnoveterinary literature from pastoral areas of eastern Africa (Catley & Mohammed 1996).
Extent of trypanosomosis prevalence from parasitological data
Trypanosome infections recorded following cattle sampling in 18 of the 21 villages are shown in Table 1. The disease prevalence ranged from 0-38% in Mwena and Tsimba respectively, and 139 cattle out of the 951 sampled were infected with trypanosomosis. The overall prevalence was 14.6%.
Knowledge on trypanocidal drugs
Information on knowledge on trypanocidal drugs showed that 98% of the farmers who used drugs knew the drug they used by name. Those who did not know the drug used had engaged veterinary personnel in order to administer the treatment. The drug use characteristics of the farmers are summarized in Table 2.
The results in Table 2 show that Veriben(R) was the most widely used drug. It also had the highest incidence of incorrect preparation, administration and dosage. Incorrect preparation entailed mainly the use of less water than is recommended by the manufacturers in the mixing of the drug. Most farmers administered it correctly except in one case where a farmer reported to have dosed the drug orally. Cases of under dosage were reported. In an effort to find out whether or not the animals that were given treatment recovered, 78% of the farmers reported that their animals did recover fully after using the drugs, and therefore, in their opinion the drugs were effective in the treatment of trypanosomosis. Those who did not report recovery gave the following reasons as possible causes of non-recovery:
* Administration of the wrong dose was reported by 11% of the farmers
* Continuous existence of tsetse-33%
* Unknown reasons-56%
Evidence of drug use from laboratory findings
Isometamidium (Ismm) levels in serum of the sampled cattle were determined using isometamidium ELISA but serum diminazene levels were not determined due to lack of a suitable assay. Table 3 shows the range of lsmm concentrations and the number of cattle, both infected and non-infected, in which these drug levels were detected. In all serum samples, Ismm was detected, implying that all animals sampled had been exposed to this compound. Although only 12% of the farmers reported to have used this compound during the reporting period, most indicated to have used it immediately before this period in anticipation of the wet season associated with high trypanosomosis prevalence.
A total of 121 cattle had trypanosome infections with Ismm levels less than 0.4 ng/m..., of which 63 and 58 were infected with Trypanosoma vivax and Trypanosoma congolense, respectively. Twelve cattle had infections with Ismm levels between 0.4-2.0 ng/m.... Seven of these were infected with T. vivax and five with T. congolense. The only infection found in Ismm above 2 ng/m... was with T. vivax.
Trypanosomes appearing in cattle blood when serum isometamidium concentrations are in excess of 6.0 ng/mg express marked resistance to isometamidium. When they occur with serum concentrations of 2.0 ng/m..., or greater, they possess a moderate level of resistance to isometamidium, and those occurring in the presence of between 0.4 and 2.0 ng/m... can be considered to be slightly resistant. At serum concentrations below 0.4 ng/m..., no inference regarding drug resistance can be made (Eisler, Arowolo, Gault, Moloo, Holmes & Peregrine 1994).
Is there resistance to trypanocidal drugs in Kwale district?
The presence of trypanosomes circulating in blood with serum Ismm levels above 0.4 ng/m... suggests the presence of resistant strains in Kwale district. However, based on the questionnaire findings, VeribenO was the only drug used by a large enough sample to enable cross-tabulation analysis between recovery and proper drug use (Poate & Daplyn 1993). The first step was to set out the response frequencies of drug use (correct and incorrect) and recovery (recovered and not recovered) in a table. This is shown in Table 4. To be able to calculate the chi-square value, the expected frequencies were computed and are shown. The calculated chi-square falls in the acceptance region. The null hypothesis that proper drug use and recovery are unrelated was therefore accepted. Although this test does not tell us anything about the cause of the non-relationship, it provides grounds to suggest that there is drug resistance within the sampled cattle in Kwale district.
Evidence of resistance from laboratory findings
Table 5 shows the number of irradiated mice sub-inoculated with T. congolense positive sera and those in which the inoculated parasites established. Stabilates were then prepared from all the positive mice and cryopreserved in liquid nitrogen. One stabilate from each village was tested for drug sensitivity in mice. Five mice were used for each stabilate, for each dosage. The dosages used were 0.1, 1.0 and 10 mg/kg body mass for isometamidium and 1, 20 and 40 mg/kg body mass for diminazene aceturate. The number of mice that relapsed for each dosage rate is shown in Table 6.
Isometamidium chloride is the most commonly used chemoprophylactic agent and the recommended dose for this purpose is 0.5-1.0 mg/kg body mass (b.m.), given intramuscularly. Dosages of 0.25-0.50 mg/kg via the same route are recommended for therapeutic purposes.
Table 6 shows relapses in mice treated with dosage level of 1 and 10 mg/kg b.m., suggesting presence of resistance to isometamidium. Furthermore, the occurrence of relapses at doses above the recommended dose of 7 mg/kg b.m. diminazene aceturate also suggests the presence of resistance to this compound.
CONCLUSION
When this study was undertaken, most farmers demonstrated awareness about trypanosomosis. Over 90 % of the respondents gave more than five correct clinical signs of the disease and correct measures that can be used to control it. They were also able to link trypanosomosis to its vector and correctly describe the likely habitat of the vector. The results from the descriptive statistics show that knowledge on trypanocidal drugs was high with over 95 % of the farmers having used the drugs in the past. These farmers could positively relate trypanocidal drugs with trypanosomosis. This study also confirms that trypanocidal drugs were the main technology in use in the management of trypanosomosis (Stevenson et al. 1993; ILRAD 1994). Additional analysis showed that untrained personnel did 73 % of the treatment and this led to cases of incorrect drug use being reported. The chi-square test showed no significant relationship between proper drug use and recovery of the treated animals. For the drugs to be said to be effective in the management of trypanosomosis such a relationship should exist. The absence of such a relationship provides grounds to suggest the presence of resistance to trypanocidal drugs in this district.
The results of the survey therefore suggest the presence of resistance to trypanocidal drugs in Kwale district. This was subsequently confirmed by laboratory findings. Thus, an approach similar to this can be useful in identifying regions where resistance to drugs is likely to occur before committing more resources for verification.
REFERENCES
CATLEY, A. & MOHAMMED, A.A. 1996. Ethnoveterinary knowledge in Sanaag region, Somaliland (Part 1): notes on local descriptions of livestock diseases and parasites. Nomadic Peoples, 36/37:2-16.
CODJIA, V., MULATU, W., MAJIWA, P.A.O., LEAK, S.G.A., ROWLANDS, G.J., AUTHIE, E., D'ITEREN, G.D.M., & PEREGRINE, A.S. 1993. Epidemiology of bovine trypanosomosis in the Ghibe valley, southwest Ethiopia. 3. Occurrence of populations of Trypanosoma congolense resistant to diminazene, isometamidium and homidium. Ada Tropica, 53:151-163.
DOLAN, R.B., STEVENSON, P.G.W., ALUSHULA, H. & OKECH, G. 1985. Failure of chemoprophylaxis against bovine trypanosomosis in Kenya. Acta Tropica, 51:113-121.
EISLER, M.C., ELLIOTT, CT. & HOLMES, P.H. 1996. A simple competitive enzyme immunoassay for the detection of the trypanocidal drug isometamidium. Therapeutic Drug Monitoring, 18:73-9.
EISLER, M.C., AROWOLO, R.O.A., GAULT, E.A., MOLOO, S.K., HOLMES, P.H. & PEREGRINE, A.S. 1994. Isometa-midium concentrations in the serum of treated cattle: correlation with prophylaxis against tsetse-transmitted Trypanosoma congolense. Acta Tropica, 56:39-50.
HIRUMI, H., HIRUMI, K. & PEREGRINE, A.S. 1993. Axenic culture of Trypanosoma congolense: application to the detection of sensitivity levels of bloodstream trypanomastigotes to diminazene aceturate, homidium chloride, isometamidium chloride and quinapyramine sulphate. Journal of Protozoology Research, 3:52-63.
ILRAD 1993. Annual Scientific Report of the International Laboratory for Research on Animal Disease. Nairobi.
ILRAD 1994. Annual Reports. Nairobi.
JAETZOLD, R. & SCHMIDT, H. 1983. Farm Management Handbook of Kenya II. Nairobi: Ministry of Agriculture.
JOSHUA, R.A., OBWOLO, M.J., BWANGAMOI, O. & MANDEBVU, E. 1995. Resistance to diminazene aceturate by Trypanosoma congolense from cattle in the Zambezi valley of Zimbabwe. Veterinary Parasitology, 60:1-6.
KAMINSKY, R., MAMMAN, M., CHUMA, F. & ZWEYGARTH, E. 1993. Time-dose-response of Trypanosoma brucei brucei to diminazene aceturate (Berenil) and in vitro simulation of drug-concentration time profiles in cattle plasma. Acta Tropica, 54:19-30.
MULUGETA, W., WILKES, J., MULATU, W., MAJIWA, P.A.O., MASAKE, R. & PEREGRINE, S. 1997. Long-term occurrence of Trypanosoma congolense resistant to diminazene, isometamidium and homidium in cattle at Ghibe, Ethiopia. Acta Tropica, 64:205-217.
MURILLA, G.A., EISLER, M.C., PEREGRINE, A.S., NDUNG'U, J.M. & HOLMES, P.H. 1999. Development and evaluation of an enzyme-linked immunosorbent assay (ELISA) for determination of the trypanocidal drug homidium in serum of treated cattle. Journal of Veterinary Pharmacology, 22:301-307.
POATE, C.D. & DAPLYN, P.P. 1993. Data for agrarian development. Cambridge: Cambridge University Press.
ROWLANDS, G.J., MULATU, W., AUTHIE, E., D'IETEREN, G.D.M., LEAK, S.G.A., NAGDA, SM. & PEREGRINE, A.S. 1993. Epidemiology of bovine trypanosomiasis in the Ghibe valley, southwest Ethiopia. 2. Factors associated with variations in trypanosome prevalence, incidence and new infections and prevalence of recurrent infection. Acta Tropica, 53:135-150.
STEVENSON, P., MUNGA, L. & DOLAN, R.B. 1993. The detrimental effects of frequent treatment of cattle with trypanocidal drugs. ISCTRC Conference Proceedings, Kampala, Uganda: 130-135.
WOO, P.T.K. 1969. The haematocrit centrifugation for the detection of trypanosomes in blood. Canadian Journal of Zoology, 47:921-923.
G.L MUGUNIERI and G.A. MURILLA
Kenya Trypanosomiasis Research Institute (KETRI), P.O. Box 362, Kikuyu, Kenya
* Author to whom correspondence is to be addressed. E-mail: ketri@net2000ke.com
Accepted for publication 13 January 2003-Editor
Copyright Onderstepoort Veterinary Institute Mar 2003
Provided by ProQuest Information and Learning Company. All rights Reserved