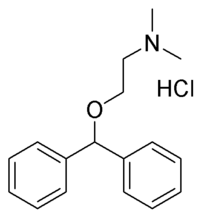
Diphenhydramine
Diphenhydramine hydrochloride (trade name Benadryl®, or Dimedrol outside the US) is an over-the-counter (OTC) antihistamine and sedative. It is also given in conjunction with typical antipsychotics to prevent akathisia. It is a member of the ethanolamine class of antihistaminergic agents. more...
Diphenhydramine is widely used in nonprescription sleep aids (Nytol, Sominex, Unisom, Compoz, Excedrin PM, etc.) with a 50mg recommended dose mandated by the FDA. In the United Kingdom, Australia, New Zealand, South Africa, and other countries, a 50 to 100mg recommended dose is permitted. In spite of its use and effectiveness as a sleep-inducing agent, when this drug is sold as an antihistamine, warning of the potential loss of alertness is never prominently displayed on packaging, leading to unknown numbers of traffic fatalities.
Unlike true antihistamines, which prevent the release of histamine, diphenhydramine works by blocking the effect of histamine at H1 receptor sites. This results in effects such as the reduction of smooth muscle contraction, making diphenhydramine a popular choice for treatment of the symptoms of allergic rhinitis, hives, motion sickness, and insect bites and stings.
Diphenhydramine is a first generation antihistamine drug. Despite being one of the oldest antihistamines on the market, it is by and large the most effective antihistamine available, either by prescription or over-the-counter, and has been shown to exceed the effectiveness of even the latest prescription drugs. Consequently, it is frequently used when an allergic reaction requires fast, effective reversal of the (often dangerous) effects of a massive histamine release. However, it is not always the drug of choice for treating allergies. Like many other first generation antihistamines, is also a potent anticholinergic agent. This leads to profound drowsiness as a very common side-effect, along with the possibilities of motor impairment (ataxia), dry mouth and throat, flushed skin, rapid or irregular heartbeat (tachycardia), blurred vision at nearpoint due to lack of accommodation (cycloplegia), abnormal sensitivity to bright light (photophobia), pupil dilatation, urinary retention, constipation, difficulty concentrating, short-term memory loss, visual disturbances, hallucinations, confusion, and delirium.
In the 1960s it was found that diphenhydramine inhibits reuptake of the neurotransmitter serotonin. This discovery led to a search for viable antidepressants with similar structures and fewer side effects, culminating in the invention of fluoxetine (Prozac), a selective serotonin reuptake inhibitor (SSRI). A similar search had previously led to the synthesis of the first SSRI zimelidine from chlorpheniramine, also an antihistamine.
Recreational drug users sometimes take several times the recommended dose of diphenhydramine in order to attain an intense hallucinogenic (more accurately, delirious) state. Abusers often call diphenhyramine "The Pink Panther", in reference to the pink colored pills and syrups or they will say they are "drillin" or "Benatrippin" because of the common name brand, Benadryl®. The mental effects are described by many as "dreaming while awake" involving visual and auditory hallucinations which, unlike those experienced with most psychedelics, often cannot be readily distinguished from reality. Many users report a side effect profile consistent with tropane glycoalkaloidal poisoning. This is due to antagonism of muscarinic acetylcholine receptors in both the central and autonomic nervous system, inhibiting various signal transduction pathways. In the CNS, diphenhydramine readily crosses the blood-brain barrier, exerting effects within the visual and auditory cortex, accounting for reported visual and auditory disturbances. Other CNS effects occur within the limbic system and hippocampus, causing confusion and temporary amnesia. Toxicology also manifests in the autonomic nervous system, primarily at the neuromuscular junction, resulting in ataxia and extrapyramidal side-effects, and at sympathetic post-ganglionic junctions, causing urinary retention, pupil dialation, tachycardia, and dry skin & mucous membranes. Considerable overdosage can lead to myocardial infarction, serious ventricular dysrhythmias, coma and death. Such a side-effect profile is thought to give ethanolamine-class antihistamines a relatively low abuse liability.
Read more at Wikipedia.org