Objective: The purpose of the present study was to examine the following during radiofrequency ablation (RFA): (1) the risk of hemorrhage from intrapulmonary large vessels; (2) the risk of incomplete ablation of pulmonary tumors; and (3) the late effect on lung tissue.
Materials and methods: A 17-gauge, cool-tip-type radiofrequency electrode was used. The damage to the vessels and bronchi was examined by the injection of a colored silicone rubber, a liquid compound that hardens after injection. To examine the risk of hemorrhage from intrapulmonary large vessels, RFA was conducted at eight sites near the central pulmonary vessels in two swine. To examine the risk of an incomplete ablation for pulmonary tumors, 10 pulmonary nodules were made from a gelatin mixture in another two swine and were treated by RFA. To examine the late effect on lung tissue, RFA was conducted on the peripheral lung in 10 rabbits, and then the ablated regions were examined on days 1, 7, 14, 21, and 28 after RFA.
Results: The use of colored silicone rubber enabled us to examine the intrapulmonary vessels and bronchi for opening and leakage. RFA did not damage the large intrapulmonary vessels, even when they were located within the ablated regions. Lung tissue surrounding the gelatin nodules was hardly ablated over its entire circumference. Six of 10 gelatin nodules (60%) showed nonablated areas on the peripheral edges of the nodules. From 21 days after RFA, the ablated rabbit lung formed noninfectious cavities by communicating with the surrounding bronchi.
Conclusion: It was improbable for hemorrhage to occur even when RFA was conducted near the large intrapulmonary large vessels. Because an incomplete ablation that left tumor cells at the site of ablation could occur during surgery due to the difficulty of ablating the entire tumor circumference, CT scan-guided RFA would be preferable to a surgical approach for making a safe margin. Cavity formation can occur beginning 21 days after RFA, which should he carefully followed up in a clinical setting to identify infection, especially in immunocompromised patients.
Key words: complication; local recurrence; lung cancer; radiofrequency ablation
Abbreviations: RF = radiofrequency; RFA = radiofrequency ablation
**********
Radiofrequency (RF) energy that induces tissue and tumor necrosis was first proposed for the treatment of osteoid osteomas (1) and liver tumors. (2) The clinical use of RF ablation (RFA) has been expanded to the treatment of pulmonary tumors. However, there have been only two experimental studies (3,4) and a few clinical studies (5-7) of RFA for the treatment of pulmonary tumors. There are still several issues that remain to be resolved, such as the following: (1) Is RFA safe for tumors located near intrapulmonary large vessels?; (2) Can a sufficient amount of lung tissue surrounding the tumor be ablated to make a safe margin?; and (3) What happens in the long term to ablated lung tissue around the tumor after RFA? To clarify these issues, we examined the damage to vessels and bronchi after RFA, and investigated the completeness of tumor ablation in swine and rabbit models.
MATERIALS AND METHODS
Colored Silicone Rubber
A colored silicone rubber (Microfil; Flow Tech, Inc; Carver, MA) is a liquid compound that is used for examination of the lumina of organs in nonsurviving animals and postmortem tissues. The silicone rubber injected into an artery fills the capillaries in the same way as blood and then exits through the veins. Approximately 20 min after the injection, the injected silicone rubber hardens, and its position can thus be used to find any opening and leakage of vessels and bronchi. It is not difficult to make microscopic sections after the injected silicone rubber has hardened.
Experiments on Swine Lung
RFA Effect on Central Lung: Two swine, weighing 33 and 37 kg, were used to study the risk of hemorrhage from intrapulmonary large vessels. The swine were anesthetized and ventilated with a pressure-controlled ventilator. For RFA on swine lungs, a 17-gauge, 2-cm active RF electrode (Cool-tip; Radionics, Inc; Burlington, MA) and an RF generator (Cosman Coagulator-1; Radionics, Inc) were used. To examine the effect of RFA on intrapulmonary large vessels, an RF electrode was directly inserted at eight sites within 5 mm in the central large pulmonary artery or vein in the two swine. The power delivery of RFA was increased stepwise beginning at 15 W/min up to a maximum of 80 W/min, and was applied until "roll-off," which indicated excess impedance of tissue at each RFA power level. After the ablation, heparin was injected IV, and then the lung was removed. A red-colored silicone rubber was injected via the main pulmonary artery, and the lung was then fixed in a 10% formalin solution.
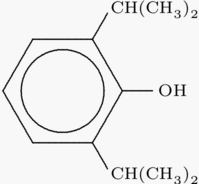
Pulmonary Tumor Model: Another two swine, weighing 32 and 35 kg, were used to study the effect of RFA on pulmonary tumors. A pulmonary tumor model was made from a mixture of gelatin (bovine skin gelatin; Wako Pure Chemical Industries; Osaka, Japan) and agar (Bacto-agar; Difco Laboratories; Detroit MI). The solution containing 25% gelatin and 5% agar was kept at 37[degrees]C. A total of 1.5 mL of mixture was injected into the peripheral lung using a 19-gauge needle to make a spherical nodule measuring about 1.5 cm in diameter (Fig 1). RFA was conducted on a total of 10 gelatin nodules in the two swine. Under visual inspection and manipulation, a 17-gauge, 2-cm, active-tip RF electrode was inserted directly into the center of each nodule. The RF energy was increased in a stepwise manner beginning at 15 W/min up to a maximum of 80 W/min and was applied until the roll-off. After RFA, the lung was removed and fixed in a 10% formalin solution.
[FIGURE 1 OMITTED]
Assessment of Damage to Rabbit Lung After RFA
Twelve adult Japanese white rabbits, 3 months old and weighing 2.6 to 3 kg, were used to study the process of lung damage after RFA. The rabbits were premedicated with a subcutaneous injection of ketamine hydrochloride (10 mg/kg) and then were maintained with a 1% propofol (Diprivan; AstraZeneca; Wilmington, DE) solution. Ventilation during surgery was conducted through a tracheostomy tube using pressure-controlled ventilation with a maximum airway pressure of 13 mm [H.sub.2]O and a respiratory rate of 25 breaths/min.
For RFA on rabbit lungs, a 17-gauge, 1-cm active-tip RF electrode (Cool-tip; Radionics, Inc) was used. After a left thoracotomy, the electrode was inserted directly into the lateral side of the left lower lobe. The RF power delivery was increased in a stepwise manner beginning at 15 W/min up to a maximum of 50 W/min, and then was applied until the roll-off. After chest closure, the rabbits were weaned from the ventilator after their normal breathing had recovered.
Ampicillin (100 mg) was administered IM from clays 1 to 5 after surgery. On each of days 1, 7, 14, 21, and 28 alter surgery, two rabbits were killed after the IV injection of heparin with an overdose of ketamine hydrochloride. After the lung and heart had been resected together, the left main pulmonary artery and the left main bronchus were cannulated with 19-gauge catheters. Red silicone rubber was injected into the left main pulmonary artery, white silicone rubber was injected into the left main bronchus, and then the materials were fixed in a 10% formalin solution.
All animals received humane care as specified in the "Guide for the Care and Use of Laboratory Animals" published by the National Institutes of Health. The present study was also approved by the Animal Care Committee of Saiseikai Central Hospital.
RESULTS
RFA Effect on Central Lung
In swine, the ablation time for the central lung tissue ranged from 12 to 15 min (mean [+ or -] SD] time, 13 [+ or -] 2 min). The RF generator showed that the initial impedance ranged from 130 to 210 [OMEGA] (mean impedance, 152 [+ or -] 38 [OMEGA]), and the temperature at the end of the ablation ranged from 64 to 75[degrees]C (mean temperature, 72 [+ or -] 6[degrees]C). Although the ablated region included large intrapulmonary vessels, the red silicone rubber filling the vessels did not leak into the lung (Fig 2). Histopathologic examination also revealed no damage to the vessels.
[FIGURE 2 OMITTED]
RFA Effect on Tumor Model
The diameters of the 10 gelatin nodules ranged from 1.4 to 1.7 cm in diameter (mean diameter, 1.5 [+ or -] 0.2 cm). The ablation time for the gelatin nodules ranged from 11 to 14 min (mean ablation time, 13 [+ or -] 2 min). The RF generator showed that the initial impedance ranged from 100 to 160 [OMEGA] (mean impedance, 137 [+ or -] 21 [OMEGA]), and the temperature ranged from 62 to 80[degrees]C (mean temperature, 73 [+ or -] 4[degrees]C). The longest diameter of the ablated nodule areas ranged from 2.3 to 2.9 cm (mean diameter, 2.6 [+ or -] 0.3 cm).
Macroscopic examination of the gelatin nodules revealed the following: (1) the ablated area generally was limited within the nodules, and the surrounding lung tissue was rarely ablated (Fig 3); and (2) even when a nodule seemed to be well-ablated over its whole area, its periphery sometimes remained unablated. Of the 10 gelatin nodules ablated, 6 had unablated areas on their peripheries (60%).
[FIGURE 3 OMITTED]
BFA on Babbit Lung
Two rabbits died within 1 h after RFA treatment from surgical and anesthetic stress. A postmortem examination of these animals did not show any bleeding or severe pneumothorax. The other rabbits tolerated the operation well and awoke without difficulty from anesthesia.
The ablation time for the rabbit lung ranged from 5 to 11 min (mean time, 7 [+ or -] 3 min). The RF generator showed that the initial impedance ranged from 150 to 250 [OMEGA] (mean impedance, 198 [+ or -] 44 [OMEGA]), and the temperature ranged from 49 to 55[degrees]C (mean temperature, 53 [+ or -] 2[degrees]C). A macroscopic examination of the vessels and bronchi filled with silicone rubber showed the following: (1) there was no leakage from the vessels along their course; (2) vessels within the ablated region were opened 1 day after ablation and closed beginning 7 days after ablation; (3) bronchi within the ablated region were opened 1 day after ablation and closed beginning 7 days after ablation; and (4) the ablated region formed a cavity by communicating with the surrounding bronchi beginning 21 days after ablation (Fig 4).
[FIGURE 4 OMITTED]
Microscopically, the region within the ablated area showed the following: (1) vessel walls showed little change throughout their course; (2) thrombi partly blocked the vessels beginning 7 days after RFA, and completely blocked them beginning 14 days after RFA (Fig 5); (3) the bronchial epithelium had not changed 1 day after RFA, but had completely peeled off beginning 7 days after RFA (Fig 5); (4) the area was surrounded by collagenous fibers beginning 21 days after RFA; and (5) the surrounding bronchi opened into the area beginning 21 days after ablation, forming a sterile cavity.
[FIGURE 5 OMITTED]
DISCUSSION
Although a massive hemorrhage during RFA has been reported in only one patient, (8) RFA can still have extremely dangerous complications, especially in the ablation of tumors that are located near large intrapulmonary vessels. We found that RFA did not damage the large vessels even when they were located within the ablated region. This was considered to be due to the cooling effect by the blood flow, (ie, the so-called heat sink effect). (9,10) Although we did not examine the late effect of RFA on the central lung, hemorrhage during RFA could hardly happen even for tumors located near large vessels, as long as the tumor did not invade the vessels and the needle of the RF electrode did not injure the vessels. However, the late effect of RFA on the central lung (eg, the possibility of formation of bronchoarterial fistula) should be further investigated. The impedance of the central lung in the present study was lower (152 [+ or -] 38 [OMEGA]) than that of the peripheral lung, probably because the ablated areas of the central lung included the large vessels and bronchi, which had low impedance (but indicated little lung tissue having high impedance).
A tumor model using gelatin nodules showed the difficulty in making a safe margin during RFA. Although the length of the RF electrode, the RF energy, ablation time, and temperature in the present study were similar to those used in general clinical practice, the lung tissue surrounding the nodules could not be sufficiently ablated. In addition, the peripheries of the gelatin nodules frequently (60%) remained unablated. Although we are not sure whether these unablated areas constituted the so-called ghost phenomena, which might later become necrotic, the difficulty in making a safe margin could possibly increase the risk of local recurrence after RFA. This problem could be partly caused by the high impedance of the aerated lung. (11) Goldberg et al (3) and Miao et al (4) reported the results of RFA of pulmonary VX2 tumors in rabbits. Goldberg et al (3) reported that residual viable tumors were present in three of seven tumors (43%) after CT scan-guided RFA. Miao et al (4) reported that local growth was seen in 3 of 12 tumors (25%) after surgically guided RFA. The results of these previous experiments support our results, which showed insufficient safe margins at the peripheries of the nodules. Although Nishida et al (7) reported that six patients with pulmonary tumors showed no recurrence from 195 to 653 days after undergoing RFA, no further sufficient long-term results have been reported. On the basis of our results, we think that RFA of pulmonary tumors could pose a higher risk of local recurrence than that of liver tumors, because the lower impedance of liver tissue makes it easier to obtain a sufficiently safe margin. Although we performed RFA under thoracotomy, CT scanning is usually used in clinical practice, enabling the extent of the ablated region to be viewed as an area of ground-grass opacity. (7) We suggest-that it is better to conduct RFA under CT scan guidance to ablate a sufficient area of normal lung tissue surrounding the tumor to make a safe margin. To increase the amount of thermally induced necrosis, several techniques, such as the use of multiprobe arrays (12) or clustered cool-tip needles, (13) and the injection of saline solution around the tumor, (14) also should be considered to prevent the local recurrence of pulmonary tumors after RFA.
Our study of the rabbit lung yielded the following new findings: (1) the blood circulation within the ablated region was completely blocked by thrombus beginning 1 week after RFA; and (2) the ablated area communicated with the surrounding bronchi beginning 3 weeks after RFA, resulting in cavity formation. The thrombus could have been caused by the following: (1) although the vessels were virtually undamaged by RFA, the circulation may have been blocked by atelectasis from the damaged bronchial epithelium; and (2) a late effect of RFA could damage the capillaries within the ablated region. Marchand et al (15) reported one patient who developed a cavity within the ablated area 1 month after undergoing RFA. In our study, cavity formation occurred 3 weeks after RFA. In clinical practice, cavity formation could cause infection, such as lung abscess or aspergillosis, especially in immunocompromised patients.
We used swine because the swine lung was big enough to select points near the central vessels and to make a suitable tumor model. We used rabbits because their long-term care after undergoing RFA is easier than that of swine. Although in clinical practice RFA is usually conducted under CT scanning not under thoracotomy, we think that the effect of RFA on the central vessels and lung tissue does not differ between humans and these animals.
We concluded the following: (1) it is hardly possible that hemorrhage could occur during the RFA of pulmonary tumors, even near large intrapulmonary vessels; (2) because an incomplete ablation that leaves tumor cells could occur under surgical RFA, CT scan-guided RFA would be preferable for making a safe margin; and (3) patients should be carefully followed up after RFA to identify any infection within the ablated region, especially in immunocompromised patients.
REFERENCES
(1) Rosenthal DI, Alexander A, Rosenberg AE, et al. Ablation of osteoid osteomas with a percutaneously placed electrode: a new procedure. Radiology 1992; 183:29-33
(2) Gazella GS, Goldberg SN, Solbiati L, et al. Tumor ablation with radio-frequency energy: state of the art. Radiology 2000; 217:633-646
(3) Goldberg SN, Gazelle GS, Compton CC, et al. Radiofrequency tissue ablation of VX2 tumor nodules in the rabbit lung. Acad Radiol 1996; 3:929-935
(4) Miao Y, Ni Y, Bosmans H, et al. Radio-frequency ablation for eradication of pulmonary tumor in rabbits. J Surg Res 2001; 99:265-271
(5) Dupuy DE, Zagoria RJ, Akerley W, et al. Percutaneous RF ablation of malignancies in the lung. AJR Am J Roentgenol 2000; 174:57-60
(6) Rose SC, Fotoohi M, Levin DL, et al. Cerebral microembolization during radiofrequency ablation of lung malignancies. J Vasc Interv Radiol 2002; 13:1051-1054
(7) Nishida T, Inoue K, Kawata Y, et al. Percutaneous radiofrequency ablation of lung neoplasms: a minimally invasive strategy for inoperable patients. J Am Coll Surg 2002; 195: 426-430
(8) Vaughn C, Mychaskiw G, Sewell P. Massive hemorrhage during radiofrequency ablation of a pulmonary neoplasm. Anesth Analg 2002; 94:1149-1151
(9) Goldberg SN, Hahn PF, Halpern EF, et al. Radio-frequency tissue ablation: effect of pharmacologic modulation of blood flow on coagulation diameter. Radiology 1998; 209:761-767
(10) Rossi S, Garbagnati F, De Francesco I, et al. Relationship between the shape and size of radiofrequency induced thermal lesions and hepatic vascularization. Tumori 1999; 85: 128-132
(11) Goldberg SN, Gazelle GS, Compton C, et al. Radiofrequency tissue ablation in the lung: a safe minimally invasive procedure. Acad Radiol 1995; 2:776-784
(12) Goldberg SN, Gazelle GS, Dawson SL, et al. Radio-frequency tissue ablation using multiprobe arrays: greater tissue destruction than multiple probes operating alone. Acad Radiol 1995; 2:670-674
(13) Goldberg SN, Solbiati L, Hahn PF, et al. Large-volume tissue ablation with radio frequency by using a clustered, internally cooled electrode technique: laboratory and clinical experience in liver metastases. Radiology 1998; 209:371-379
(14) Livragni T, Goldberg SN, Lazzaroni S, et al. Saline-enhanced RF tissue ablation in the treatment of liver metastases [abstract]. Radiology 1995; 197:140
(15) Marchand B, Perol M, Roche EDL, et al. Percutaneous radiofrequency ablation of a lung metastasis: delayed cavitation with no infection. J Comput Assist Tomogr 2002; 26: 1032-1034
* From the Department of Thoracic Surgery (Drs. Nomori, Imazu, Watanabe, Ohtsuka, Naruke, and Suemasu), Saiseikai Central Hospital, Tokyo, Japan; and the Endoscopy Division (Dr. Kobayashi), National Cancer Center Hospital, Tokyo, Japan.
This work was supported in part by a grant-in-aid from the Ministry of Health, Labor, and Welfare of Japan.
Manuscript received April 2, 2004; revision accepted September 10, 2004.
Correspondence to: Hiroaki Nomori, MD, PhD, Department of Thoracic Surgery, Saiseikai Central Hospital, 1-4-17 Mita, Minato-ku, Tokyo 108-0073, Japan; e-mail: hnomori@qkg.sonet.nejp
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group