ABSTRACT. Background: Although early enteral feeding clearly reduces septic morbidity after blunt and penetrating trauma, data for head-injured patients are conflicting. This study examines the effects of early vs delayed enteral feedings on outcome in patients with severe closed-head injuries with a Glasgow Coma Scale (GCS) score greater than 3 and less than 11. Methods: Thirty patients were prospectively randomized to receive an immune-enhancing diet (Impact with fiber) early (initiated
the late group died before 72 hours. Five of the remaining 27 died, 1 in the early group and 4 in the late group. There were no significant differences between the groups in length of stay, intensive care unit (ICU) days, significant infection, or GCS score. However, major infection correlated inversely with admission GCS score (R = -0.6, p
Although victims of multiple trauma are rarely malnourished on admission to the hospital, the hypermetabolism that follows can quickly lead to depletion of lean body mass. This places patients at high risk for complications, particularly infectious complications, which can lead to increased length of hospital stay, increased morbidity, and increased costs. In many studies of patients with blunt and penetrating trauma, the use of early enteral nutrition has been shown to reduce the incidence of septic complications along with length of stay and hospital costs5 when compared with parenteral nutrition (PN). In addition, early initiation of enteral feeding has similar benefits compared with delayed enteral nutrition in certain patient populations.6,7
Studies addressing the route and timing of nutrition in head-injured patients are relatively few but it is recognized that a gastroparesis lasting 3-5 days frequently complicates the early postinjury period. Rapp et alb demonstrated that compared with delayed enteral feeding when gastroparesis had resolved, early total parenteral nutrition (TPN) appeared to improve neurologic outcome. Unfortunately, in a follow-up study, this result could not be duplicated.9 Obtaining access beyond the ligament of Treitz is necessary to institute successful early enteral feeding, and the additional costs and effort necessary to achieve this access has been justified by improved infectious outcome in one study.7 No other studies of early Us delayed enteral feeding in head-injured patients has been undertaken until now. At present, it is not clear whether the resource commitment to obtain early postligament of Treitz access is worth the costs and risks compared with early TPN or delayed enteral feeding.
In prior studies of head-injured patients, the incidence of infection is extremely high, and pneumonia rates range from 17%-60%.7,9-15 Because these patients appear to be immunocompromised, the use of an immune-enhancing formula might be expected to be beneficial in this population. These formulas have been shown to improve cellular measures of immune function in multiple models16-22 and decrease wound and infectious complications in patients with multiple trauma and those undergoing surgical procedures for upper gastrointestinal tract malignancy.20,22-24 They also have been shown to decrease length of hospital stay in trauma and burn patients.23,25,26 Therefore, in this study of early vs delayed enteral nutrition, an immune-enhancing formula was used to try to influence primary outcome measures, ie, length of hospital and ICU stay, along with the rate of infectious complications.
MATERIALS AND METHODS
This study was a prospective, randomized trial of patients with severe closed-head injuries admitted to the Regional Medical Center at Memphis, a Level I trauma center. Institutional Review Board approval was obtained before initiation of the study. Patients with severe closed-head injuries as defined by a Glasgow Coma Scale (GCS) score greater than 3 and less than 11 within 6 hours of injury were eligible. Exclusion criteria are shown in Table I. After informed consent was obtained from family or guardian, patients were randomly assigned into early us delayed enteral feeding. Patients in the early group had a nasoenteric tube (Stay-Put, Novartis Nutrition Corporation, Minneapolis, MN) placed endoscopically and feeding begun within 60 hours of injury. The delayed group had feeding initiated by the nutrition support team when gastroparesis resolved. This was determined by a decrease in nasogastric tube output to less than 500 mL/d with no abdominal distention or vomiting for approximately 24 hours after the tube was removed. Although almost all patients in the late group were fed via a small-bore nasogastric tube, one had recovered enough to take food orally. All patients receiving tube feedings were given Impact (Novartis Nutrition Corporation) with fiber, an immune-enhancing formula containing supplemental arginine, nucleic acids, w-3 fatty acids, and fiber. Goal rate of nutrition was 21 nonprotein calories per kilogram per day (27 kcal/kg/d) and 0.3 gN/kg/d. After day 15, all patients who still required enteral feeding were placed on a standard enteral formula. Patients were followed daily for 14 days, after which time only infections, length of stay, and mortality were tracked. Our protocol was that PN would be started at day 10 if patients were not receiving at least 75% of goal; however, no patient required this. Patients were dropped from the study if they expired less than 72 hours from injury or if jejunal access could not be obtained.
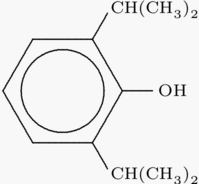
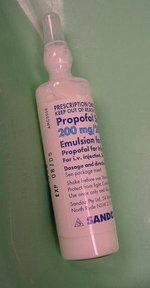
Care of the patients' head injuries was by protocol as per the neurosurgery service. Intracranial pressure monitors or ventriculostomies were placed in patients with a GCS less than 9. Euvolemia was maintained, and pulmonary artery catheters were inserted if necessary in difficult patients. Intracranial pressure (ICP) was kept below 20 if possible. Methods to decrease ICP included sedation (using narcotics, benzodiazepines, diprivan, or even paralysis or pentobarbital coma, if necessary), hyperventilation, the use of mannitol or furosemide to decrease intravascular volume, or hypertonic saline. Cerebral perfusion pressure was kept above 70; if the ICP could not be decreased or if the mean arterial pressure was low after volume resuscitation, pressors could be used to increase blood pressure.
Data collection included patient demographics, associated injury, Injury Severity Score (ISS), type of head injury, daily GCS scores, length of ICU and hospital stay, number of ventilator days, along with infectious and feeding complications. Criteria for the diagnosis of pneumonia are shown in Table II. Centers for Disease Control criteria were used to define other infections. Major infections included pneumonia, empyema, and neurologic infections. Patients were evaluated daily for the presence and severity of feeding complications including abdominal distention, vomiting, diarrhea, and aspiration. The number of days to a GCS of 14 were also recorded, because a score of 14 would correspond to a "good result" in the Glasgow Outcome Score Scale.
Statistics
Primary outcome variables were lengths of stay in the ICU and hospital, ventilator days, significant infections per patients, and numbers of patients with infections. For demographic characteristics and outcome variables, differences between the early and late groups were assessed with Student's t tests and x^sup 2^ tests. In addition, Spearman correlation coefficients were estimated to quantify associations among outcome and demographic variables. Finally, the KaplanMeier method was used to obtain survival estimates for time in days to a GCS of 14; two separate analyses strata, defined as either early and late nutrition or having and not having infections, were compared.
RESULTS
Thirty patients were entered into the study; however, three patients were dropped from analysis: two in the early group due to inability to place a nasoenteric tube and one patient in the delayed group who died less than 72 hours after injury. Demographics of the remaining 27 patients are shown in Table III. There were no significant differences between the groups. Although not an exclusion criteria, no patient with spinal cord injury was entered into the study. Five patients died during the study: one in the early group and four patients in the late group. This was not statistically significant.
As expected, patients in the early group had feeding initiated sooner than patients in the late group. In addition, the number of days fed and the number of patients who received at least 50% of their goal nutrition for longer than 5 days was greater in the early group. The average daily caloric intake (Table IV) was higher in the early group because they had several more days of feeding than the late group. There were no significant differences between groups with regard to mortality, length of hospital or ICU stay, ventilator days, number of infections per patient, or patients with pneumonia (Table V). Nine of the 13 patients with pneumonia had their diagnosis confirmed by bronchoalveolar lavage. In fact, there appears to be a trend toward increased ICU and hospital length of stay along with ventilator days in the early group. This can partially be attributed to a 27% mortality rate in the late group (Table VI).
There were a number of minor feeding complications but no statistically significant differences between groups (Table VII). Most of these complications were transient and required no specific therapy. No patients required PN due to intolerance of enteral feeding. However, there were two cases of aspiration, both in the late group. One patient developed severe pulmonary failure and died. This was the only patient in the study whose death was not attributed to his/her head injury.
A correlation analysis was performed to determine predictors of outcome. The only independent predictor of major infection was admission GCS score (R = - 0.6, p
Rapidity of neurologic recovery, as measured by the days to reach a GCS of 14 was not related to the timing of feeding but was significantly different between patients who developed major infections and those who did not. Fewer patients with infections reached a GCS of 14 during their hospital stay, and those who reached a GCS of 14 took longer to do so than patients without infections (p
DISCUSSION
The enteral route of nutrition support has been shown to have an effect on infectious morbidity in many animal models and in trauma patients. Early administration of nutrients enterally (
In one of the earliest studies of patients with severe head injuries, Rapp et alb randomly assigned 38 patients to early PN vs standard enteral nutrition. The enteral feeding was initiated after gastric ileus resolved, which usually occurred between day 5 and 9. Initiation and progression of enteral feeding was greatly delayed as evidenced by a caloric intake of more than 1400 kcal in the PN group on days 2-18 compared with the late enteral group, who did not exceed 800 kcal/d until day 14. Early mortality was higher in the enteral group, although 75% of those deaths was due to the head injury. The authors claimed that the PN group had a better neurologic recovery at 1 year but if the patients who died are removed from analysis, there were no differences in outcome. In a follow-up study by the same investigators, 51 patients with severe head injuries were randomly assigned using the same protocol: early PN or enteral feeds after gastric ileus resolved.9 Patients who were unable to tolerate tube feedings by day 7 were also started on PN. No significant differences in mortality or infection rates were found. Neurologic recovery was better in the PN group at 3 months; however, there were no differences between groups at 6 or 12 months. Together, these two studies suggest some potential benefit of early PN compared with delayed (> 1 week) enteral feeding.
In 1989, Grahm et al7 studied 32 trauma patients with severe head injuries who were randomly divided into two groups: one that received early enteral feeds, the other delayed. The study group had nasojejunal tubes placed endoscopically and feeds were initiated within 36 hours of admission. Control subjects had gastric feeds initiated when gastric function returned. ICU length of stay was significantly shortened in the experimental group (7 us 10 days) and there were fewer infectious complications in the experimental group (3 as 14). This study supported the use of early enteral nutrition in this patient population. On the other hand, Borzotta et al21 randomly assigned 59 brain-injured patients to jejunal feeds via surgical jejunostomy or PN within 72 hours of injury. There were no differences in the incidence of infection or hospital length of stay that could be attributed to route of nutrition. Although early nutrition appears to be beneficial compared with delayed nutrition in patients with head injuries, perhaps the route is not as important as it is in trauma patients sustaining torso injuries.
In the current study comparing early us delayed nutrition using an immune-enhancing formula, timing of the feeding had no impact on major infectious complications or length of stay. It should be noted that due to an aggressive nutrition support team, some of the patients in the late group had their nutrition initiated before those in the early group. However, even when data were corrected for hour postinjury of feeding initiation, ISS, or presence of pulmonary injuries (data not shown) no differences could be found. In previous studies, investigators had difficulty feeding head-injured patients earlier than 5-7 days. In this study, all but one patient in the late group was fed by day 5, so this study could be interpreted as very early us early feeding. The primary predictor of the outcome measurement was, not surprisingly, admission GCS score. The severity of the admission mental status was inversely related to hospital length of stay, ICU length of stay, ventilator days, major infections, and pneumonia.
The reason that the use of early enteral nutrition did not appear to benefit this patient population is purely speculative. It is possible that the immune disturbances caused by head injury and the effects of the therapeutic maneuvers used to treat the injury are so substantial that any benefit incurred by early nutrition may be significantly overwhelmed. In addition, prolonged intubation, chemical paralysis, sedation, prolonged recumbency, and routine ICU care increase the risk of pneumonia and other nosocomial infections.
The use of an immune-enhancing formula in these patients did not appear to improve the rate of infectious complications when compared with historical controls. The rate of pneumonia (the vast majority of infections) was almost 50% in both groups, which approximates the pneumonia rates in previous studies of head-injured patients.9-15 However, a concurrent group of head-injured patients fed a standard formula would be needed to evaluate this further.
Admittedly, this is a small group of patients. A power analysis was not done before the initiation of this study because no other studies of head injured patients fed an immune-enhancing formula in an early us delayed fashion were available. An analysis was done after 30 patients were entered. There were not any positive trends with early feeding in any of the outcome variables. In fact, all of the trends favored delayed feeding. Because of these results, it was elected to end the study. So many patients would have been required to not only reverse the trend but to show a statistically significant benefit to early feeding that it did not seem reasonable to pursue this costly, labor-intensive therapy.
In summary, in this study of early as delayed feeding using an immune-enhancing formula in patients with severe head injury, timing of the initiation of feeding was not found to have an impact on the rate of infectious complications or length of stay. Admission GCS score was the only predictor of these outcomes. Patients with infections also took longer to reach a GCS of 14, if at all. In conclusion, although the use of early enteral nutrition using an immune-enhancing formula via an endoscopically placed nasoenteric tube appears to be safe, it does not appear to confer any benefit compared with beginning enteral nutrition when the patient's gastric ileus resolves.
ACKNOWLEDGMENTS
The authors thank Doris Parsons for her secretarial support in manuscript preparation. The study was supported by Novartis Nutrition Corporation.
REFERENCES
1. Moore FA, Moore EE, Jones TN, et al: TEN versus TPN following major abdominal trauma-Reduced septic morbidity. J Trauma 29:916-923, 1989
2. Feliciano DV, Spjut-Patrinely V, Burch JM: Enteral versus parenteral nutrition in patients with severe penetrating abdominal trauma. Contemn Sure 39:30-36. 1991
3. Kudsk KA, Croce MA, Fabian TC, et al: Enteral versus parenteral feeding. Ann Surg 215:503-513, 1992
4. Moore FA, Feliciano DV, Andrassy RJ, et al: Early enteral feeding, compared with parenteral, reduces postoperative septic complications. Ann Surg 216:172-183, 1992
5. Trice S, Melinik G, Page CP: Complications and costs of early postoperative parenteral versus enteral nutrition in trauma patients. Nutr Clin Pract 12:114-119, 1997
6. Moore EE, Jones TN: Benefits of immediate jejunostomy feeding after major abdominal trauma-A prospective, randomized study. J Trauma 26:874-881, 1986
7. Grahm TW, Zadrozny DB, Harrington T: The benefits of early jejunal hyperalimentation in the head-injured patient. Neurosurgery 25:729-735, 1989
8. Rapp RP, Young B, Twyman D, et al: The favorable effect of early parenteral feeding on survival in head-injured patients. J Neurosurg 58:906-911, 1983
9. Young B, Ott L, Twyman D, et al: The effect of nutritional support on outcome from severe head injury. J Neurosurg 67:668-676, 1987
10. Woratyla SP, Morgan AS, Mackay L, et al: Factors associated with early onset pneumonia in the severely brain-injured patient. Conn Med 59:643-647, 1995
11. Quattrocchi KB, Issel BW, Miller CH, et al: Impairment of helper T-cell function following severe head injury. J Neurotrauma 9:1-9, 1992
12. Rodriguez JL, Gibvbons KJ, Bitzer LG, et al: Pneumonia, incidence, risk factors, and outcome in injured patients. J Trauma 31:907-914, 1991
13. Hsieh AH-H, Bishop MJ, Kubilis PS, et al: Pneumonia following closed head injury. Am Rev Respir Dis 146:290-294, 1992
14. Piek J, Chesnut RM, Marshall LF, et al: Extracranial complications of severe head injury. J Neurosurg 77:901-907, 1992
15. Borzotta AP, Pennings J, Papasadero B, et al: Enteral versus parenteral nutrition after severe closed head injury. J Trauma 37:459-468, 1994
16. Schilling J, Vranjes N, Fierz W, et al: Clinical outcome and immunology of postoperative arginine, omega-3 fatty acids, and nucleotide-enriched enteral feeding: A randomized prospective
comparison with standard enteral and low calorie/low fat i.v. solutions. Nutrition 12:423-429, 1996
17. Cerra FB, Lehmann S, Konstantinides N, et al: Improvement in immune function in ICU patients by enteral nutrition supplemented with arginine, RNA, and Menhaden oil is independent of nitrogen balance. Nutrition 7:193-199, 1991
18. Kemen M, Senkal M, Homann H-H, et al: Early postoperative enteral nutrition with arginine-w-3 fatty acids and ribonucleic acid-supplemented diet versus placebo in cancer patients: An immunologic evaluation of Impact. Crit Care Med 23:652-659, 1995
19. Braga M, Vignali A, Gianotti L, et al: Immune and nutritional effects of early enteral nutrition after major abdominal operations. Eur J Surg 162:105-112, 1996
20. Moore FA, Moore EE, Kudsk KA, et al: Clinical benefits of an immune-enhancing diet for early postinjury enteral feeding. J Trauma 37:607-615, 1994
21. Mendez C, Jurkovich GJ, Wener MH, et al: Effects of supplemental dietary arginine, canola oil, and trace elements on cellular immune function in critically injured patients. Shock 6:7-12, 1996
22. Daly JM, Lieberman MD, Goldfine J, et al: Enteral nutrition with supplemental arginine, RNA, and omega-3 fatty acids in patients after operation: Immunologic, metabolic, and clinical outcome. Surgery 112:56-67, 1992
23. Daly JM, Weintraub FN, Shou J, et al: Enteral nutrition during multimodality therapy in upper gastrointestinal cancer patients. Ann Surg 221:327-338, 1995
24. Mendez C, Jurkovich GJ, Garcia I, et al: Effects of an immuneenhancing diet in critically injured patients. J Trauma 42:933940, 1997
25. Kudsk KA, Minard G, Croce MA, et al: A randomized trial of isonitrogenous enteral diets following severe trauma: An immune-enhancing diet (IED) reduces septic complications. Ann Surg 224:531-543, 1996
26. Gottschlich MM, Jenkins M, Warden GD, et al: Differential effects of three enteral dietary regimens on selected outcome variables in burn patients. JPEN 14:225-236, 1990
Gayle Minard, MD*; Kenneth A. Kudsk, MD*; Sherry Melton, MD*; Joseph H. Patton, MD*; and Elizabeth A. Tolley, PhD^
From the Departments of *Surgery, and ^Biostatistics & Epidemiology, The University of Tennesse, Memphis
Received for publication, August 21, 1998.
Accepted for publication, December 20, 1999.
Correspondence: Gayle Minard, MD, 956 Court Avenue, Suite E228, Memphis, TN 38163. Electronic mail may be sent to gminard@utmem.edu.
Presented at the 22nd Clinical Congress of the American Society for Parenteral & Enteral Nutrition, Lake Buena Vista, Florida, January 18-21, 1998.
Copyright American Society for Parenteral and Enteral Nutrition May/Jun 2000
Provided by ProQuest Information and Learning Company. All rights Reserved