Paclitaxel, the first of the taxanes, has exhibited unique and encouraging single-agent activity in the treatment of non-small cell lung cancer (NSCLC). Yet, with single-agent response rates approaching 25%, it was logical to examine the impact of paclitaxel in combination chemotherapy regimens. In trials evaluating the activity of paclitaxel in combination with one of the platinum compounds, cisplatin or carboplatin, response rates have ranged from 35 to [is greater than] 50% and were significantly better than response rates observed with etoposide/cisplatin, the previous standard regimen for treatment of NSCLC. Docetaxel is a newer taxane that also has exhibited notable single-agent activity and response rates ranging from 20 to 50% when combined with cisplatin. Future research will look to refine the use of taxane combinations in NSCLC and to examine the potential of these unique and promising drugs when combined with newer agents that are active against this disease. (CHEST 2000; 117.144S-151S)
Key words: carboplatin; cisplatin; docetaxel; non-small cell lung cancer; paclitaxel; taxanes
Abbreviations: AUC = area under the plasma concentration-vs-time curve; ECOG = Eastern Cooperative Oncology Group;NSCLC = non-small cell lung cancer
In this article, we explore the use of paclitaxel and docetaxel combinations in chemotherapy for patients with non-small cell lung cancer (NSCLC).
PACLITAXEL IN NSCLC
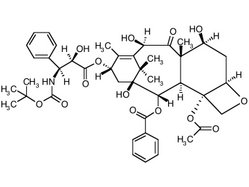
Paclitaxel (Taxol; Bristol-Myers Oncology; Princeton, NJ), the first of the taxanes, is a unique antimicrotubule agent that shifts the equilibrium of the cancer cell toward microtubule assembly and stabilizes tubulin polymer formation. This disrupts the normal dynamic reorganization of the microtubule network, which is essential for vital interphase and mitotic function.[1,2] Early studies evaluating a 24-h infusion schedule of paclitaxel in the treatment of advanced and metastatic NSCLC (Table 1) yielded response rates of 21%3 and 24%.[4] The most significant finding from the early trials with paclitaxel was the markedly improved 1-year survival rate, which reached 40%. Subsequent studies using shorter infusion schedules (3-h and 1-h)[5-8] yielded similar results (Table 1), with the added benefit of the potential for outpatient administration. More recently, dose-dense schedules (full doses administered weekly) (Table 1) also have yielded promising early results in NSCLC patients (response rate, 56%; 1-year survival rate, 53%), although neuropathy and myelosuppression are dose-limiting. The question of whether weekly paclitaxel at maximum dose intensity is, in fact, more effective than the conventional every 3- or 4-week schedule in NSCLC has not yet been answered.
(*) Administered weekly for 6 weeks.
Paclitaxel Combinations in NSCLC
The provocative results obtained with single-agent paclitaxel prompted its use in combinations with other agents that are active against NSCLC, such as the platinum compounds cisplatin and carboplatin. The combination of paclitaxel with cisplatin produced response rates of 35 to 47% in early phase I/II studies (Table 2),[11-13] although there appeared to be a sequence-dependent increase in myelotoxicity when paclitaxel was administered after cisplatin.[14,15] In a large randomized study, the paclitaxel (moderate- and high-dose)/cisplatin combination was compared with a cisplatin/etoposide regimen for the treatment of advanced and metastatic NSCLC (Table 3).[16] The response rates noted with both paclitaxel doses (moderate-dose regimen, 27%; high-dose regimen, 32%) were significantly higher than those observed with the etoposide/ cisplatin regimen (12%); in addition, there was an overall improvement in survival with the paclitaxel-containing arms, which was greatest for patients with stage IIIB disease. These results led to the assignment of paclitaxel/ cisplatin rather than cisplatin/etoposide as the reference regimen for the present randomized Eastern Cooperative Ontology Group (ECOG) study (Fig 1).[17,18]
[Figure 1 ILLUSTRATION OMITTED]
Table 2--Paclitaxel (3-h Infusion) and Cisplatin in NSCLC: Phase I/II Studies(*)
(*) NR = not reported.
(*) Adapted from Bonomi et al.[16]
Carboplatin has comparable activity but a better toxicity profile than cisplatin in patients with NSCLC.[19-24] As carboplatin is primarily excreted by the kidney, the dose can be individualized based on creatinine clearance or glomerular filtration rates, thus avoiding any undue toxicity and optimizing the therapeutic index. Carboplatin has been evaluated in combination with paclitaxel in a number of phase I/II studies involving patients with advanced and metastatic NSCLC (Table 4).[25-27]
Table 4--Paclitaxel (24-h Infusion) and Carboplatin in Advanced and Metastatic NSCLC: Phase I/II Studies(*)
(*) G-CSF = granulocyte colony-stimulating factor. See Table 2 for other abbreviation.
([dagger]) Intrapatient escalation.
Initial studies of the carboplatin/paclitaxel combination using a 24-h infusion of paclitaxel established that myelosuppression was the dose-limiting toxicity.[28-31] In other studies, a shorter 1- or 3-h infusion schedule was associated with a significant decrease in myelosuppression, making neuropathy the dose-limiting toxicity.[32-40] The various infusion schedules, however, did not diminish the activity observed with paclitaxel/carboplatin in patients with NSCLC (Tables 5, 6).
Table 5--Paclitaxel (3-h Infusion) and Carboplatin in Advanced and Metastatic NSCLC. Phase I-II Studies
Table 6--Paclitaxel (1-h Infusion) and Carboplatin in Advanced and Metastatic NSCLC. Phase I/II Studies
(*) Intrapatient dose escalation.
Two unique observations were made from these phase I/II studies of the paclitaxel/carboplatin combination. First, most responses in patients with NSCLC occurred at paclitaxel doses [is greater than] 175 mg/[m.sup.2], suggesting a dose-response effect.[32,35] Second, the combination was not associated with significant platelet toxicity, suggesting that paclitaxel may exert a myeloprotective effect against thrombocytopenia, which is generally associated with carboplatin use.[41] The mechanism for this platelet-protective effect may involve some alteration of megakaryocytopoiesis or thrombocytopoiesis, which could result in increased levels of endogenous thrombopoietin or other cytokines. Ongoing studies are measuring the effect on thrombopoietin. It is also possible that prior exposure to paclitaxel may suppress the inhibition of proplatelet formation, which is associated with carboplatin, when measured in terms of pharmacodynamic effect on platelets.[41]
To date, the best results with the paclitaxel/carboplatin combination have come from the Fox Chase Cancer Center,[26] where a 62% response rate and 54% 1-year survival were noted with paclitaxel (escalating doses, intrapatient, between 135 and 215 mg/[m.sup.2] with subsequent courses of chemotherapy) and carboplatin (dosed to an area under the plasma concentration-vs-time curve [AUC] of 7.5). Today, the recommended doses for this combination are: paclitaxel 200 mg/[m.sup.2] to 225 mg/[m.sup.2] by 3-h or 1-h infusion or 175 mg/[m.sup.2] by 24-h infusion with carboplatin targeted to an AUC of 6 or 7.
The first large randomized study comparing paclitaxel/ carboplatin with standard cisplatin/etoposide therapy in patients with advanced or metastatic NSCLC (Fig 2) has been completed, accruing 369 patients in 15 months. The median survival time of the combined group was 8.25 months, and the 1-year survival rate was 35%.[42] The number of events required to perform a survival analysis, by study arm, has not been attained, and the results are eagerly awaited. In addition, the paclitaxel/carboplatin combination has become the most widely used regimen for patients with NSCLC in the United States based on the spectrum of activity, the case of administration, and the wide acceptance by both patients and their treating physicians. This regimen is being investigated further in ongoing randomized cooperative group studies. The controversies regarding the best schedule (24-h vs 3-h vs 1-h) and the optimum dose of paclitaxel in the combination may never be resolved, but further refinement of this regimen by the addition of cytoprotective agents, such as amifostine, to abrogate neuropathy and myelosuppression or growth factors, such as thrombopoetin or megakaryocyte growth and development factor, may prove valuable.
[Figure 2 ILLUSTRATION OMITTED]
DOCETAXEL IN NSCLC
Docetaxel has demonstrated single-agent activity in both chemotherapy-naive patients with advanced NSCLC (Table 7)[43-49] and in patients whose disease has progressed after or while receiving cisplatin-based regimens (Table 8).[50-52] Myelosuppression is the predominant toxicity observed with docetaxel in all of these studies. Other unique toxicities include nail changes, hypersensitivity reactions, and occasionally symptomatic peripheral edema or effusions.
Table 7--Phase II Studies of Docetaxel in Previously Untreated Patients With Advanced NSCLC(*)
(*) See Table 2 for abbreviation.
Table 8--Docetaxel in Previously Treated Patients With Recurrent NSCLC(*)
(*) See Table 2 for abbreviation.
Docetaxel/Cisplatin Combination in NSCLC
Docetaxel was combined with cisplatin in a multicenter study to evaluate its efficacy against NSCLC. The recommended dose of 75 mg/[m.sup.2] docetaxel in combination with 75 mg/[m.sup.2] cisplatin with cycles repeated every 3 weeks[53,54] was administered to 47 chemotherapy-naive patients with advanced and metastatic NSCLC.[55] The main toxicities observed with this regimen were febrile neutropenia (8.5%), pulmonary toxicity (4.3%), neuromotor effects (2.1%), and asthenia (12.8%). Symptomatic fluid retention occurred in only one patient. Other adverse effects, including nausea, vomiting, diarrhea, and stomatitis, were rare. The observed response rate in this study was 21.3% (95% confidence interval, 10.7 to 35.7%) including one complete response and nine partial responses. The median survival of all patients entered is 10 + months. Based on this activity, the docetaxel/cisplatin combination is being evaluated in an ongoing randomized ECOG study (Fig 2) involving patients with stages IIIB and IV NSCLC.
The combination of docetaxel and cisplatin for NSCLC has been evaluated in three other trials.[54,56,57] Zalcberg and colleagues[54] used the same dosing schema as in our study (Table 9).[55] LeChevalier and colleagues[56] used a modified regimen of the same combination with a higher cisplatin dose (100 mg/[m.sup.2]) and administered it on a 3-week schedule for the first three cycles, then on a 6-week schedule (Table 10). The highest response rate of 48% was noted by Androulakis et al[57] (Table 9); however, the dose intensity of docetaxel was higher, and all patients received filgrastim support in this study. Thus, the combination of docetaxel and cisplatin appears to be active,[55] and confirmation of its activity in the randomized setting is awaited.
Table 9--Docetaxel and Cisplatin Combination in NSCLC: Results of Phase II Studies
Table 10--Docetaxel and Cisplatin Combination in NSCLC: Results of Phase II Studies
(*) With filgrastim, 5 [micro]g/kg, d 5 to 15.
Docetaxel/Carboplatin Combination in NSCLC
Carboplatin, developed as the less toxic analog of cisplatin, has marginal but consistent activity in patients with NSCLC.[58-61] In a large randomized ECOG study[58] comparing three cisplatin-based combination chemotherapy regimens to single-agent carboplatin and iproplatin, the best survival rate was observed on the carboplatin arm. Thus, carboplatin was considered to be suitable for combination with docetaxel.
Phase I Study of Docetaxel and Carboplatin in Advanced Solid Tumors: A phase I study[61] of patients with refractory advanced solid tumors was designed to identify the maximum tolerated dose and toxicity level of docetaxel (with and without filgrastim support) plus carboplatin in combination (Table 11). The docetaxel dose was escalated from 65 mg/[m.sup.2] (cohort 1) to 80 mg/[m.sup.2] (cohort 2), 90 mg/[m.sup.2] (cohort 3), and 100 mg/[m.sup.2] (cohort 4), with each dose followed by carboplatin administration (Table 12). The carboplatin dose was targeted to an AUC of 6 using the Calvert formula[59] (dose [in milligrams] = target AUC [glomerular filtration rate + 25]). The measured 24-h urinary creatinine clearance was substituted for the glomerular filtration rate. Cycles were repeated every 3 weeks. The dose-limiting toxicity on this docetaxel/carboplatin regimen was febrile neutropenia, reached in cohort 3 (docetaxel dose 90 mg/[m.sup.2]); thus, filgrastim was added in cohort 4 (Table 12). The maximum tolerated doses of docetaxel, with and without filgrastim support, in this combination were 100 mg/[m.sup.2] and 90 mg/[m.sup.2], respectively. Other grade 3 toxicities in this study were rare, but included hypotension, GI bleeding, low back pain, nausea, and fatigue. Carboplatin had no effect on docetaxel pharmacokinetics in this study. The authors identified a recommended docetaxel dose of 90 mg/[m.sup.2] with filgrastim support and 80 mg/[m.sup.2] without filgrastim support for further evaluation in combination with carboplatin (AUC, 6).
Table 11--Multicenter Phase II Study of Docetaxel and Carboplatin for Stage IIIB and IV NSCLC: Treatment Regimen
(*) Calvert's formula.
Table 12--Dose-Escalation Schema for the Phase I Study of Docetaxel/Carboplatin
Phase II Trial of Docetaxel and Carboplatin in NSCLC: Preliminary results from a phase II multicenter study of docetaxel and carboplatin in the treatment of advanced and metastatic NSCLC were presented at the 1997 meeting of the International Association for the Study of Lung Cancer.[62] There were 33 patients enrolled and 26 patients evaluable for response in this study; 1 complete response and 14 partial responses were observed in this population, for an overall response rate of 58%. The main toxicities included severe myalgia (15%), asthenia (12%), arthralgia (6%), and febrile neutropenia (12%). The incidence of grade 3/4 neutropenia was 67%, leading the investigators to reduce the dose of carboplatin for the next group of patients to an AUC of 5. Nonetheless, the regimen of docetaxel/carboplatin was considered active against metastatic NSCLC.
FUTURE DIRECTIONS
The search for new agents and treatment approaches remains an important goal of research in NSCLC. The development of three-drug combination regimens, for example, currently is underway. Newer agents found to be active in NSCLC, such as gemeitabine, vinorelbine, or irinotecan, are being combined with the paclitaxel/carboplatin or the docetaxel/carboplatin combinations. Paclitaxel or docetaxel has been combined with these agents to form nonplatinum doublets, and their activity is being evaluated as well. For the first time, a nonplatinum doublet, paclitaxel/gemeitabine, has been incorporated into the investigational arm of a proposed European Organization for Research and Treatment of Cancer study (Fig 3). A large randomized study comparing the docetaxel/carboplatin doublet to the docetaxel/cisplatin and vinorelbine/cisplatin doublets has been initiated. These ongoing studies will provide further insight into the activity and toxicity of combination chemotherapy for NSCLC. With the encouraging results obtained in advanced and metastatic NSCLC, the paclitaxel- and docetaxel-based regimens and combinations are being investigated in earlier stages of the disease, and the results appear to be promising.
[Figure 3 ILLUSTRATION OMITTED]
The taxanes, with their wide spectrum of activity and unique mechanism of action, have sparked a great deal of interest about their use in the management of NSCLC. Ongoing and future investigations will aim to optimize and refine the paclitaxel and docetaxel combinations.
REFERENCES
[1] Rowinsky EK, Donehower RC. Paclitaxel (Taxol). N Engl J Med 1995; 332:1004-1014
[2] Horwitz SB. Mechanism of action of Taxol. Trends Pharmacol Sci 1992; 13:134-136
[3] Chang AY, Kim K, Glick J, et al. Phase II study of Taxol, merbarone, and piroxantrone in stage IV non-small-cell lung cancer: The Eastern Cooperative Ontology Group Results. J Natl Cancer Inst 1993; 85:388-394
[4] Murphy WK, Fossella FV, Winn RJ, et al. Phase II study of Taxol in patients with untreated advanced non-small-cell lung cancer. J Natl Cancer Inst 1993; 85:384-388
[5] Gatzemeier U, Heckmayer M, Neuhauss R, et al. Chemotherapy of advanced inoperable non-small cell lung cancer with paclitaxel: a phase II trial. Semin Oncol 1995; 22(suppl): 24-28
[6] Millward M J, Bishop JF, Friedlander M, et al. Phase II trial of a 3-hour infusion of paclitaxel in previously untreated patients with advanced non-small-cell lung cancer, J Clin Oncol 1996; 14:142-148
[7] Rowinsky EK, Eisenhauer EA, Chaudhry V, et al. Clinical toxicities encountered with paclitaxel (Taxol). Semin Oncol 1993; 20(suppl):1-15
[8] Eisenhauer EA, ten Bokkel Huinink WW, Swenerton KD, et al. European-Canadian randomized trial of paclitaxel in relapsed ovarian cancer: high-dose versus low-dose and long versus short infusion. J Clin Oncol 1994; 12:2654-2666
[9] Hainsworth JD, Thompson DS, Greco FA. Paclitaxel by 1-hour infusion: an active drug in metastatic non-small-cell lung cancer. J Clin Oncol 1995; 13:1609-1614
[10] Akerley W, Choy H, Safran H, et al. Weekly paclitaxel: marked activity, diminished toxicity and platelet stimulating effect [abstract]. Lung Cancer 1997; 18(suppl):19
[11] Klastersky J, Sculier jP. Cisplatin plus Taxol in non-small cell lung cancer: a dose finding trial [abstract]. Proc Am Assoc Cancer Res Annu Meet 1995; 36:A1423
[12] Pirker R, Krajnik G, Zoehbauer S, et al. Paclitaxel/cisplatin in advanced non-small cell lung cancer (NSCLC). Ann Oncol 1995; 6:833-835
[13] Belli L, LeChevalier T, Gottfried M, et al. Phase I-II trial of paclitaxel (Taxol) and cisplatin in previously untreated advanced non-small cell lung cancer (NSCLC) [abstract]. Proc Am Soc Clin Oncol Annu Meet 1995; 14:350
[14] Rowinsky EK, Citardi MJ, Noe DA, et al. Sequence-dependent cytotoxic effects due to combinations of cisplatin and the antimicrotubule agents Taxol and vincristine. J Cancer Res Clin Oncol 1993; 119:727-733
[15] Rowinsky EK, Gilbert MR, McGuire WP, et al. Sequences of Taxol and
cisplatin: a phase I and pharmacologic study, J Clin Oncol 1991; 9:1692-1703
[16] Bonomi PD, Kim K, Chang A, et al. Phase III trial comparing etoposide (E) cisplatin versus Taxol (T) with cisplatin G-CSF (G) versus cisplatin in advanced non-small cell lung cancer: Eastern Cooperative Oncology Group (ECOG) [abstract]. Proc Am Soc Clin Oncol Annu Meet 1996; 15:382
[17] Gelmon KA, Tolcher A, O'Reilly S, et al. Phase I/II trial of biweekly paclitaxel (Taxol) in metastatic breast cancer [abstract]. Proc Am Soc Clin Oncol Annu Meet 1995; 14:132
[18] Georgiadis MS, Brown JE, Schuler BS, et al. Phase I study of a four clay continuous infusion of paclitaxel followed by cisplatin in patients with advanced lung cancer [abstract]. Proc Am Soc Clin Oncol Annu Meet 1995; 14:353
[19] Bonomi PD, Finkelstein DM, Ruckdeschel JC, et al. Combination chemotherapy versus single agents followed by combination chemotherapy in stage IV non-small cell lung cancer: a study of the Eastern Cooperative Oncology Group. J Clin Oncol 1989; 7:1602-1613
[20] Kramer BS, Birch R, Greco A, et al. Randomized phase II evaluation of iproplatin (CHIP) and carboplatin (CBDCA) in lung cancer. Am J Clin Oncol 1988; 11:643-645
[21] Kreisman H, Ginsberg S, Propert KJ, et al. Carboplatin or iproplatin in advanced non-small cell lung cancer: a Cancer and Leukemia Group B study. Cancer Treat Rep 1987; 71:1049-1052
[22] Gandara DR, Wold H, Perez EA, et al. Cisplatin dose intensity in non-small cell lung cancer: phase II results of a day 1 and day 8 high-dose regimen. J Natl Cancer Inst 1989; 81:790-794
[23] Wozniak AJ, Crowley JJ, Balcerzak SP, et al. Randomized phase III trial of cisplatin (CDDP) vs. CDDP plus navelbine (NVB) in treatment of advanced non-small cell lung cancer (NSCLC): report of a Southwest Oncology Group study (SWOG-9308) [abstract]. Proc Am Soc Clin Oncol Annu Meet 1996; 15:374
[24] Klastersky J, Sculier JP, Bureau G, et al. Cisplatin versus cisplatin plus etoposide in the treatment of advanced non--small cell lung cancer. J Clin Oncol 1989; 7:1087-1092
[25] Belani CP, Aisner J, Hiponia D, et al. Paclitaxel and carboplatin in metastatic non-small cell lung cancer: preliminary results of a phase I study. Semin Oncol 1996; 23(suppl): 19-21
[26] Langer CJ, Leighton JC, Comis RL, et al. Paclitaxel and carboplatin in combination in the treatment of advanced non-small cell lung cancer: a phase II toxicity, response, and survival analysis. J Clin Oncol 1995; 13:1860-1870
[27] Johnson DH, Paul DM, Hande KR, et al. Paclitaxel plus carboplatin in advanced non-small cell lung cancer: a phase II trial. J Clin Oncol 1996; 14:2054-2060
[28] Lee FH, Cabetta R, Ussekk BF, et al. New platinum complexes in clinical trials. Cancer Treat Rev 1983; 10:43-45
[29] Canetta R, Franks C, Smaldone L, et al. Clinical status of carboplatin. Oncology 1987; 1:61-69
[30] Bonomi PD, Finkelstein DM, Ruckdeschel JC, et al. Combination chemotherapy versus single agents followed by combination chemotherapy in stage IV non-small-cell lung cancer: a study of the Eastern Cooperative Oncology Group (ECOG). J Clin Oncol 1989; 7:1602-1613
[31] Bunn PA Jr. Review of therapeutic trials of carboplatin in lung cancer. Semin Oncol 1989; 16(suppl):27-33
[32] Natale RB. Preliminary results of a phase I/II clinical trial of paclitaxel and carboplatin in non-small cell lung cancer. Semin Oncol 1996; 23(suppl):2-6
[33] Rowinsky EK, Flood WA, Sartorius SE, et al. Phase I study of paclitaxel as a 3-hour infusion followed by carboplatin in untreated patients with stage IV non-small cell lung cancer. Semin Oncol 1995; 22(suppl):48-54
[34] Schutte W, Bork I, Sucker S. Phase II trial of paclitaxel and carboplatin as firstline treatment in advanced non-small cell lung cancer (NSCLC) [abstract]. Proc Am Soc Clin Oncol Annu Meet 1996; 15:398
[35] Bunn PA Jr, Kelly K. A phase I study of carboplatin and paclitaxel in non-small cell lung cancer: a University of Colorado Cancer Center study. Semin Oncol 1995; 22(suppl): 2-6
[36] Giaccone G, Huizing M, Postmus PE, et al. Dose-finding and sequencing study of paclitaxel and carboplatin in non-small cell lung cancer. Semin Oncol 1995; 22:78-82
[37] Hainsworth JD, Thompson DS, Urba WJ, et al. One hour paclitaxel plus carboplatin in advanced non-small cell lung cancer (NSCLC): preliminary results of a multi-institutional phase II study [abstract]. Proc Am Soc Clin Oncol Annu Meet 1996; 15:379
[38] Langer C, Kaplan R, Rosvold E, et al. Paclitaxel (P) by 1 hour (hr) infusion combined with carboplatin (C) in advanced non-small cell lung carcinoma [abstract]. Proc Am Soc Clin Oncol Annu Meet 1996; 15:396
[39] Roa V, Conner A, Mitchell RB. Carboplatin and paclitaxel for chemotherapy-naive patients with advanced non-small cell lung cancer [abstract]. Proc Am Soc Clin Oncol Annu Meet 1996; 15:404
[40] Evans WK, Stewart DJ, Tomiak E, et al. Carboplatin (C) and paclitaxel (P) by one hour infusion for advanced non-small cell lung cancer (NSCLC) [abstract]. Proc Am Soc Clin Oncol Annu Meet 1995; 14:374
[41] Kearns CM, Belani CP, Erkmen K, et al. Reduced platelet toxicity with combination carboplatin and paclitaxel; pharmacodynamic modulation of carboplatin associated thrombocytopenia [abstract]. Proc Am Soc Clin Oncol Annu Meet 1995; 14:170
[42] Belani CP, Natale R, Lee JS, et al. Randomized study of cisplatin/etoposide versus paclitaxel/carboplatin in advanced and metastatic non-small cell lung cancer [abstract]. Proc Am Soc Clin Oncol Annu Meet 1998; 17:455a
[43] Cerny T, Kaplan S, Pavlidis N, et al. Docetaxel (Taxotere) is active in non-small cell lung cancer: a phase II trial of the EORTC early clinical trials group (ECTG). Br J Cancer 1994; 70:384 -387
[44] Francis PA, Rigas JR, Kris MG, et al. Phase II trial of docetaxel in patients with stage III and IV non-small cell lung cancer. J Clin Oncol 1994; 12:1232-1237
[45] Burris HA, Eckardt J, Fields S, et al. Phase II trials of taxotere in patients with non-small cell lung cancer [abstract]. Proc Am Soc Clin Oncol Annu Meet 1993; 12:335
[46] Fossella FV, Lee JS, Murphy WK, et al. Phase II study of docetaxel for recurrent or metastatic non-small cell lung cancer. J Clin Oncol 1994; 12:1238-1244
[47] Watanabe K, Yokoyama A, Furuse K, et al. Phase II trial of docetaxel in previously untreated non-small cell lung cancer (NSCLC) [abstract]. Proc Am Soc Clin Oncol Annu Meet 1994; 13:331
[48] Miller VA, Rigas JR, Francis PA, et al. Phase II trial of a 75 mg/[m.sup.2] dose of docetaxel with prednisone premedication for patients with advanced non-small lung cancer. Cancer 1995; 75:968-972
[49] Lira-Puerto V, Zepeda G, Mohar A, et al. Phase-II trial of Taxotere (docetaxel) in advanced non-small cell lung cancer [abstract]. Proc Am Soc Clin Oncol Annu Meet 1995; 14:382
[50] Burris H, Eckardt J, Fields S, et al. Phase II trials of Taxotere in patients with non-small cell lung cancer [abstract]. Proc Am Soc Clin Oncol Annu Meet 1993; 12:338
[51] Fossella FV, Lee JS, Shin DM, et al. Phase II study of docetaxel (Taxotere) for advanced or metastatic platinum-refractory non-small cell lung cancer. J Clin Oncol 1995; 13:645-651
[52] Gandara DR, Vokes E, Green M, et al. Docetaxel (Taxotere) in platinum-treated non-small cell lung cancer (NSCLC): confirmation of prolonged survival in a multicenter trial [abstract]. Proc Am Soc Clin Oncol Annu Meet 1996; 16:508
[53] Pronk LC, Schellens JH, Planting AS, et al. Phase I and pharmacologic study of docetaxel and cisplatin in patients with advanced solid tumors. J Clin Oncol 1997; 15:1071-1091
[54] Zalcberg JR, Bishop JF, Millward MJ, et al. Interim results of a phase II trial of docetaxel in combination with cisplatin in patients with metastatic or locally advanced non-small cell lung cancer (NSCLC) [abstract]. Eur J Cancer 1995; 31A(suppl):S226
[55] Belani CP, Bonomi P, Dobbs T, et al. Multicenter phase II trial of docetaxel and cisplatin combination in patients with non-small cell lung cancer [abstract]. Proc Am Soc Clin Oncol Annu Meet 1997; 16:221a
[56] LeChevalier T, Belli L, Monnier A, et al. Phase II study of docetaxel (Taxotere) and cisplatin in advanced non-small cell lung cancer (NSCLC): an interim analysis [abstract]. Proc Am Soc Clin Oncol Annu Meet 1995; 14:350
[57] Androulakis N, Dimopoulos AM, Kourousis C, et al. First-line treatment of advanced non-small cell lung cancer (NSCLC) with docetaxel and cisplatin: a multicenter phase II study [abstract]. Proc Am Soc Clin Oncol Annu Meet 1997; 16:461a
[58] Bonomi PD, Finkelstein DM, Ruckdeschel JC, et al. Combination chemotherapy versus single agents followed by combination chemotherapy in stage IV non-small cell lung cancer: a study of the Eastern Cooperative Oncology Group. J Clin Oncol 1989; 7:1602-1613
[59] Calvert AH, Harland SJ, Newell DR, et al. Early clinical studies with cis-diammine-1, 1 cyclobutane-decarboxylate platinum II. Cancer Chemother Pharmacol 1982; 9:140-147
[60] Curt GA, Grygeil JJ, Corden BJ, et al. A phase I and pharmacokinetic study of diammine-cyclobutane-decarboxylate-platinum (NSC 241240). Cancer Res 1983; 43:4470-4473
[61] Belani CP, Hadeed V, Ramanathan R, et al. Docetaxel and carboplatin: a phase I and pharmacokinetic trial for advanced non-hematologic malignancies [abstract]. Proc Am Soc Clin Oncol Annu Meet 1997; 16:220a
[62] Belani CP, Einzig A, Bonomi P, et al. Multi-institutional phase II trial of docetaxel and carboplatin combination in patients with stage IIIB and IV non-small cell lung cancer (NSCLC) [abstract]. Lung Cancer 1997; 18:16
(*) From the Division of Medical Oncology, Department of Medicine, University of Pittsburgh School of Medicine, and University of Pittsburgh Cancer Institute, Pittsburgh, PA.
Correspondence to: Chandra P. Belani, MD, University of Pittsburgh Cancer Institute, 200 Lothrop St, MUH N-725, Pittsburgh, PA 15213; e-mail: belanicp@msx.upmc.edu
COPYRIGHT 2000 American College of Chest Physicians
COPYRIGHT 2000 Gale Group