Definition
Restless legs syndrome (RLS) is characterized by unpleasant sensations in the limbs, usually the legs, that occur at rest or before sleep and are relieved by activity such as walking. These sensations are felt deep within the legs and are described as creeping, crawling, aching, or fidgety.
Description
Restless legs syndrome, also known as Ekbom syndrome, Wittmaack-Ekbom syndrome, anxietas tibiarum, or anxietas tibialis, affects up to 10-15% of the population. Some studies show that RLS is more common among elderly people. Almost half of patients over age 60 who complain of insomnia are diagnosed with RLS. In some cases, the patient has another medical condition with which RLS is associated. In idiopathic RLS, no cause can be found. In familial cases, RLS may be inherited from a close relative, most likely a parent.
Causes & symptoms
Most people experience mild symptoms. They may lie down to rest at the end of the day and, just before sleep, will experience discomfort in their legs that prompts them to stand up, massage the leg, or walk briefly. Eighty-five percent of RLS patients either have difficulty falling asleep or wake several times during the night, and almost half experience daytime fatigue or sleepiness. It is common for the symptoms to be intermittent. They may disappear for several months and then return for no apparent reason. Two-thirds of patients report that their symptoms become worse with time. Some older patients claim to have had symptoms since they were in their early 20s, but were not diagnosed until their 50s. Suspected under-diagnosis of RLS may be attributed to the difficulty experienced by patients in describing their symptoms.
More than 80% of patients with RLS experience periodic limb movements in sleep (PLMS). These random movements of arms or legs may result in further sleep disturbance and daytime fatigue. Most patients have restless feelings in both legs, but only one leg may be affected. Arms may be affected in nearly half of patients.
There is no known cause for the disorder, but recent research has focused on several key areas. These include:
- Central nervous system (CNS) abnormalities. Several types of drugs have been found to reduce the symptoms of RLS. Based on an understanding of how these drugs work, theories have been developed to explain the cause of the disorder. Levodopa and other drugs that correct problems with signal transmission within the central nervous system (CNS) can reduce the symptoms of RLS. It is therefore suspected that the source of RLS is a problem related to signal transmission systems in the CNS.
- Iron deficiency. The body stores iron in the form of ferritin. There is a relationship between low levels of iron (as ferritin) stored in the body and the occurrence of RLS. Studies have shown that older people with RLS often have low levels of ferritin. Supplements of iron sulfate have been shown to significantly reduce RLS symptoms for these patients.
Diagnosis
A careful history enables the physician to distinguish RLS from similar types of disorders that cause night time discomfort in the limbs, such as muscle cramps, burning feet syndrome, and damage to nerves that detect sensations or cause movement (polyneuropathy).
The most important tool the doctor has in diagnosis is the history obtained from the patient. There are several common medical conditions that are known to either cause or to be closely associated with RLS. The doctor may link the patient's symptoms to one of these conditions, which include anemia, diabetes, disease of the spinal nerve roots (lumbosacral radiculopathy), Parkinson's disease, late-stage pregnancy, kidney failure (uremia), and complications of stomach surgery. In order to identify or eliminate such a primary cause, blood tests may be performed to determine the presence of serum iron, ferritin, folate, vitamin B12, creatinine, and thyroid-stimulating hormones. The physician may also ask if symptoms are present in any close family members, since it is common for RLS to run in families and this type is sometimes more difficult to treat.
In some cases, sleep studies such as polysomnography are undertaken to identify the presence of PLMS that are reported to affect 70-80% of people who suffer from RLS. The patient is often unaware of these movements, since they may not cause him to wake. However, the presence of PLMS with RLS can leave the person more tired, because it interferes with deep sleep. A patient who also displays evidence of some neurologic disease may undergo electromyography (EMG). During EMG, a very small, thin needle is inserted into the muscle and electrical activity of the muscle is recorded. A doctor or technician usually performs this test at a hospital outpatient department.
Treatment
The first step in treatment is to treat existing conditions that are known to be associated with RLS and that will be identified by blood tests. If the patient is anemic, iron (iron sulfate) or vitamin supplements (folate or vitamin B12) will be prescribed. If kidney disease is identified as a cause, treatment of the kidney problem will take priority.
Prescription drugs
In some people whose symptoms cannot be linked to a treatable associated condition, drug therapy may be necessary to provide relief and restore a normal sleep pattern. Prescription drugs that are normally used for RLS include:
- Benzodiazepines and low-potency opioids. These drugs are prescribed for use only on an "as needed" basis, for patients with mild RLS. Benzodiazepines appear to reduce nighttime awakenings due to PLMS. The benzodiazepine most commonly used to treat RLS is clonazepam (Klonopin, Rivotril). The main disadvantage of this drug type is that it causes daytime drowsiness. It also causes unsteadiness that may lead to accidents, especially for an elderly patient. Opioids are narcotic pain relievers. Those commonly used for mild RLS are low potency opioids, such as codeine (Tylenol #3) and propoxyphene (Darvocet). Studies have shown that these can be successfully used in the treatment of RLS on a long-term basis without risk of addiction. However, narcotics can cause constipation and difficulty urinating.
- Levodopa (L-dopa) and carbidopa (Sinemet). Levodopa is the drug most commonly used to treat moderate or severe RLS. It acts by supplying a chemical called dopamine to the brain. It is often taken in conjunction with carbidopa to prevent or decrease side effects. Although it is effective against RLS, levodopa may also causes a worsening of symptoms during the afternoon or early evening in 50-80% of patients. This phenomenon is known as "restless legs augmentation," and if it occurs, the physician will probably discontinue Levodopa for a brief period while an alternate drug is used. Levodopa can often be reintroduced after a short break.
- Pergolide (Permax). Pergolide acts on the same part of the brain as Levodopa. It is less likely than Levodopa to cause daytime worsening of symptoms (occurs in about 25% of patients). However, it is not recommended as the first choice in drug therapy since it causes a high rate of minor side effects. Pergolide is often used only if Levodopa has been discontinued.
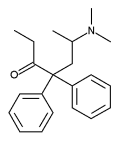
- High potency opioids. If the symptoms of RLS are difficult to treat with the above medication, higher dose opioids will be used. These include methadone (Dolophine), oxycodone, and clonidine (Catapres, Combipres, Dixarit). A significant disadvantage of these drugs is risk of addiction.
- Anticonvulsants. Some cases of RLS may be improved by anticonvulsant drugs, such as carbamazepine (Tegretol).
- Combination therapy. Some patients respond well to combinations of drugs such as a benzodiazepine and Levodopa.
Many drugs have been investigated for treatment of RLS, but it seems as though the perfect therapy has not yet been found. However, careful monitoring of side effects and good communication between patient and doctor can result in a flexible program of therapy that minimizes side effects and maximizes effectiveness.
Alternative treatment
It is likely that the best alternative therapy will combine both conventional and alternative approaches. Levodopa may be combined with a therapy that relieves pain, relaxes muscles, or focuses in general on the nervous system and the brain. Any such combined therapy that allows a reduction in dosage of levodopa is advantageous, since this will reduce the likelihood of unacceptable levels of drug side effects. Of course, the physician who prescribes the medication should monitor any combined therapy. Alternative methods may include:
- Acupuncture. Patients who also suffer from rheumatoid arthritis may especially benefit from acupuncture to relieve RLS symptoms. Acupuncture is believed to be effective in arthritis treatment and may also stimulate those parts of the brain that are involved in RLS.
- Homeopathy. Homeopaths believe that disorders of the nervous system are especially important because the brain controls so many other bodily functions. The remedy is tailored to the individual patient and is based on individual symptoms as well as the general symptoms of RLS.
- Reflexology. Reflexologists claim that the brain, head, and spine all respond to indirect massage of specific parts of the feet.
- Nutritional supplements. Supplementation of the diet with vitamin E, calcium, magnesium, and folic acid may be helpful for people with RLS.
Some alternative methods may treat the associated condition that is suspected to cause restless legs. These include:
- Anemia or low ferritin levels. Chinese medicine will emphasize stimulation of the spleen as a means of improving blood circulation and vitamin absorption. Other treatments may include acupuncture and herbal therapies, such as ginseng (Panax ginseng) for anemia-related fatigue.
- Late-stage pregnancy. There are few conventional therapies available to pregnant women, since most of the drugs prescribed are not recommended for use during pregnancy. Pregnant women may benefit from alternative techniques that focus on body work, including yoga, reflexology, and acupuncture.
Prognosis
RLS usually does not indicate the onset of other neurological disease. It may remain static, although two-thirds of patients get worse with time. The symptoms usually progress gradually. Treatment with Levodopa is effective in moderate to severe cases that may include significant PLMS. However, this drug produces significant side effects, and continued successful treatment may depend on carefully monitored use of combination drug therapy. The prognosis is usually best if RLS symptoms are recent and can be traced to another treatable condition that is associated with RLS. Some associated conditions are not treatable. In these cases, such as for rheumatoid arthritis, alternative therapies such as acupuncture may be helpful.
Prevention
Diet is key in preventing RLS. A preventive diet will include an adequate intake of iron and the B vitamins, especially B12 and folic acid. Strict vegetarians should take vitamin supplements to obtain sufficient vitamin B12. Ferrous gluconate may be easier on the digestive system than ferrous sulfate, if iron supplements are prescribed. Some medications may cause symptoms of RLS. Patients should check with their doctor about these possible side effects, especially if symptoms first occur after starting a new medication. Caffeine, alcohol, and nicotine use should be minimized or eliminated. Even a hot bath before bed has been shown to prevent symptoms for some sufferers.
Key Terms
- Anemia
- A condition that affects the size and number of red blood cells. It often results from lack of iron or certain B vitamins and may be treated with iron or vitamin supplements.
- Insomnia
- Trouble sleeping. People who suffer from RLS often lose sleep either because they spend time walking to relieve discomfort or because they have PLMS, which causes them to wake often during the night.
- Periodic limb movements in sleep (PLMS)
- Random movements of the arms or legs that occur at regular intervals of time during sleep.
Further Reading
For Your Information
Books
- The Editors of Time-Life Books. The Medical Advisor. The Complete Guide to Conventional and Alternative Medicine. Alexandria, VA: Time Life Books, 1997.
- Long, James W., and James J. Rybacki. The Essential Guide to Prescription Drugs. New York: HarperPerennial, 1995.
- Mills, Simon, and Stephen J. Finando. Alternatives in Healing. New York: New American Library, 1989.
- "Peripheral Neuropathies." In Mayo Clinic Family Health Book, edited by David E. Larson. New York: William Morrow and Company, 1996.
Periodicals
- Montplaisir, Jaques, et al. "Clinical, Polysomnographic, and Genetic Characteristics of Restless Legs Syndrome: A Study of 133 Patients Diagnosed with New Standard Criteria." Movement Disorders 12 (1997): 61-65.
- O'Keeffe, Shaun T. "Restless Legs Syndrome: A Review." Archives of Internal Medicine 56 (Feb 12, 1996): 243-246.
- Silber, Michael H. "Concise Review for Primary-Care Physicians. Restless Legs Syndrome." Mayo Clinical Proceedings 72 (March 1997): 261-264.
Organizations
- Restless Legs Syndrome Foundation. 1904 Banbury Road, Raleigh, NC 27608-4428. (919) 781-4428. http://www.rls.org.
Gale Encyclopedia of Medicine. Gale Research, 1999.