Kaletra soft gelatin capsules are bright orange and imprinted with the Abbott corporate logo and "PK" in black ink. A liquid formulation is also available. Dosing may vary.
On September 15, 2000, the US Food and Drug Administration (FDA) granted Abbott Laboratories accelerated approval for the marketing of Kaletra (lopinavir/ritonavir), making it the seventeenth agent licensed for the treatment of HIV infection. The FDA based its approval on the results of 3 surrogate marker studies.
Also known as: ABT-378
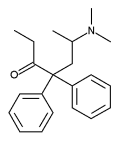
Background and indication. An inhibitor of HIV protease, Kaletra binds to the enzyme's active site, disrupting its normal function. The result is the production of immature, noninfectious virions. Kaletra is indicated, in conjunction with other antiretrovirals, for the treatment of HIV infection. Kaletra is a combination product, containing 2 protease inhibitors: lopinavir and ritonavir (Norvir); however, the antiviral activity of Kaletra is almost wholly attributable to lopinavir. The addition of ritonavir is for the purpose of raising levels of lopinavir in the blood.
How supplied and description. Kaletra is supplied in both capsules and solution. The capsules contain 133.3 mg of lopinavir and 33.3 mg of ritonavir. They are orange, soft gelatin and imprinted with Abbott's corporate logo. The solution contains 400 mg of lopinavir and 100 mg of ritonavir per 5 mL. It is light yellow to orange in color. The solution is 42.4% alcohol.
Dose. If taken by capsule, the correct dose of Kaletra is 3 capsules twice daily, for a total of 6 capsules a day. If taken by solution, the correct dose is 5 mL twice daily, for a total of 10 mL a day. However, when Kaletra is combined with either efavirenz (Sustiva) or nevirapine (Viramune) in treatment experienced patients, the correct dose is 4 capsules twice daily or 6.5 mL of solution twice daily.
Food restrictions. Since food enhances the drug's absorption, Kaletra should be taken with a meal or snack.
Storage. Both the capsules and the solution should be refrigerated at 36 [degrees] F to 46 [degrees] F until dispensed; however, both formulations can be kept at a room temperature of up to 77 [degrees] F if used within 2 months.
Side effects. The clinical side effects most commonly associated with Kaletra therapy are nausea and diarrhea. The most common laboratory abnormalities are increases in some tests of liver function, as well as increases in triglycerides and total cholesterol. Elevated triglycerides are associated with a risk of developing pancreatitis. Of note, during clinical trials of Kaletra, approximately 1 in 4 treatment experienced patients saw a grade 3 or grade 4 laboratory abnormality. Grade 3 abnormalities are considered serious and grade 4 abnormalities are life-threatening.
Resistance and cross-resistance. Genomic point mutations associated with resistance to lopinavir/ritonavir have not yet been identified; however, isolates with reduced to susceptibility to Kaletra have been selected both in vitro and in vivo.
The relevance of resistance to other protease inhibitors (PIs) on the virologic success of Kaletra has not yet been fully characterized. In a study of 56 patients who had been treated with at least 2 other PIs, a Kaletra-containing regimen suppressed viral load below the limits of quantification (400 copies/mL) in 24 of 25 patients whose baseline virus contained 5 point mutations associated with resistance to PI therapy. However, these 25 patients, all of whom were naive to non-nucleoside reverse transcriptase inhibitors (NNRTIs), were given efavirenz (Sustiva), a potent NNRTI, in addition to Kaletra and nucleoside reverse transcriptase inhibitors (NRTIs). Therefore, it is difficult to assess the relative contribution of Kaletra to the virologic success experienced by the patients in that study.
Drug interactions. Kaletra is metabolized in the liver by cytochrome P450, almost wholly by the CYP3A isoform. Other drugs that are metabolized by the same pathway are therefore contraindicated with Kaletra. These drugs are:
* flecainide (Tambocor)
* propafenone (Rythmol)
* astemizole (Hismanal)
* terfenadine (Seldane)
* any ergot derivative (e.g. dihydroergotamine or DHE)
* cisapride (Propulsid)
* pimozide (Orap)
* midazolam (Versed)
* triazolam (Halcion)
* lovastatin (Mevacor)
* simvastatin (Zocor)
* hypericum perforatum (St. John's wort)
When co-administered with Kaletra, sildenafil (Viagra) should be limited to 25 mg every 48 hours. When Kaletra and didanosine (Videx) are combined, didanosine should be taken 1 hour before or 2 hours after Kaletra. HIV-infected women who are taking estrogen-based contraceptives should use additional or alternative contraceptives while on Kaletra.
Important interactions between Kaletra and other agents, including rifabutin (Mycobutin), disulfiram (Antabuse), metronidazole (Flagyl), methadone (Dolophine) and corticosteroids, may require adjusted dosing of either drug and are noted in Kaletra's package insert.
Finally, Kaletra has the potential to reduce the plasma concentrations of zidovudine (Retrovir) and abacavir (Ziagen); however, the clinical significance of those reductions, if any, is unknown.
Clinical data in treatment naive patients. Study 863 is a double-blind trial in which investigators randomized 653 treatment naive patients to a regimen of Kaletra plus stavudine (Zerit)and lamivudine (Epivir) or nelfinavir (Viracept) plus stavudine and lamivudine. The participants, mostly Caucasian males, had an average baseline CD4 T cell count of 259 cells/[mm.sup.3] and an average baseline viral load of approximately 79,000 copies/mL. After 24 weeks, 79% of participants in the Kaletra arm had viral loads less than 400 copies/mL, with 65% having viral loads less than 50 copies/mL. Participants saw an average CD4 T cell increase of 154 cells/[mm.sup.3].
Importantly, 3 patients in the Kaletra arm and 3 patients in the nelfinavir arm experienced new AIDS-defining clinical events despite having viral loads below the limit of quantification. These data demonstrate that while a reduction in viral load greatly reduces the risk of disease progression on a population basis, even an unquantifiable viral load does not preclude the occurrence of AIDS-defining events in the individual.
Clinical data in treatment experienced patients. Study 765 is a randomized, blinded trial using 2 doses of Kaletra, namely 400 mg of lopinavir and 100 mg of ritonavir or 400 mg of lopinavir and 200 mg of ritonavir. The participants, all of whom had taken 1 prior protease inhibitor but were naive to NNRTIs, also took the NNRTI nevirapine (Viramune) plus 2 NRTIs. The study volunteers were mostly Caucasian males with an average baseline CD4 T cell count of 372 cells/[mm.sup.3] and an average baseline viral load of approximately 10,000 copies/mL.
After 72 weeks of treatment, 75% of volunteers in the 400 mg/100 mg arm had viral loads less than 400 copies/mL, with 58% having viral loads less than 50 copies/mL. The average CD4 T cell increase was 174 cells/[mm.sup.3].
Patient assistance. For those who qualify, Abbott Laboratories offers a patient assistance program for Kaletra. For more information, call 800.222.6885. Select option 1.
Summary and analysis. In view of the widespread need for second generation therapies, activists and the community press have eagerly awaited the arrival of Kaletra. Although Kaletra's resistance profile has yet to be adequately characterized, the clinical data strongly suggest that the drug has durable activity against HIV in patients previously exposed to other PIs. Although Kaletra's twice daily dosing with food is no improvement over other agents in convenience, its apparent activity against PI-resistant virus is a meaningful therapeutic advance.
Kaletra's introduction to the market is, however, accompanied by reasonable concerns about the drug's safety in previously treated patients. Among subjects with a history of prior therapy, the level of serious drug-related laboratory abnormalities, as reported in clinical trials, is worrisome. Moreover, abnormalities in tests of liver function suggest that Kaletra's clinical utility may be hampered among those with chronic hepatitis, who now constitute perhaps a third of the HIV-infected population.
Recommendation. The Center for AIDS recommends that the Panel on Clinical Practices for Treatment of HIV Infection classify Kaletra as a "preferred" therapy.
COPYRIGHT 2000 The Center for AIDS: Hope & Remembrance Project
COPYRIGHT 2001 Gale Group