Chronic Bladder Infections
Although we will be discussing some unusual infections in upcoming columns, CFIDS/FMS patients also get more of the day-to-day variety of infections. These include urinary tract (bladder) infections (UTIs), prostatitis and sinusitis.
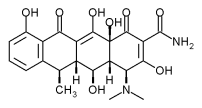
[ILLUSTRATION OMITTED]
The main symptoms of a UTI are dysuria (discomfort--for example, a burning sensation--when urinating), urgency (the feeling that you have to go very badly and right away when there is not much urine there), and frequent urination with low urine volume. This group of symptoms is also common in CFIDS/FMS patients in the absence of bladder infections and, when severe, is called interstitial cystitis (IC). However, I would not say that a person has interstitial cystitis unless this is the major symptom of their CFIDS/FMS, because almost everyone with this illness has some urinary urgency and frequency. The few people who have IC need to be careful, as many vitamin supplements can cause symptoms to flare up.
Because bladder symptoms can be seen in both UTIs and CFIDS/FMS, it is important to have a urine culture done before initiating treatment with antibiotics to make sure that it is infection, and not just muscle spasms in the bladder, that is causing these symptoms. If there is an infection, over 90% of the time it will be with Escherichia coli (E. coli). This bacteria is normally found in the intestines and, with the exception of a few rare, dangerous forms, is a healthy part of normal bowel bacteria. The problem occurs when the E. coli gets out of the bowel, where it belongs, and into the bladder. Most infectious organisms are washed out of the bladder when the urine comes out. E. coli, however, have little Velcro-like projections that stick to the bladder wall so that they cannot be washed out by urination.
Taking antibiotics will kill a bladder infection, but will also kill the healthy bacteria in the bowel. This sets you up for yeast overgrowth and other problems. Because of this, unless the patient has fever, back pain over the kidneys, or a toxic feeling, it is reasonable to try natural remedies for one to three days before going with the antibiotics. You can start these treatments while waiting for the results of the urine culture to come back.
There are two excellent natural remedies that can keep the E. coli from sticking to the bladder walls so they can be washed out. In addition, taking high doses of vitamin C (500 to 5,000 milligrams a day) can acidify the urine, making it inhospitable to the bacteria. Drinking a lot of water also helps to wash out the infection. The two natural remedies that keep the bacteria from sticking are cranberries and D-mannose (I prefer the latter). They can be very effective, but they work only for bladder infections caused by E. coli bacteria--approximately 90% of all bladder infections.
Cranberries
Because approximately 20% of the female population suffers from UTIs, several studies have been done looking at this remedy. In an early study, 44 female and 16 male patients with acute bladder infections drank 16 ounces of cranberry juice a day for fifteen days. Of these patients, 53% had positive responses and another 20% showed modest improvement. Six weeks after stopping the juice, twenty-seven patients did have persistent or recurrent infections and eight of these had no symptoms. Seventeen patients had no symptoms and negative urine cultures.
In another study of elderly women (who are more likely than younger women to have bladder infections), 153 women either received 10 ounces of cranberry drink or placebo every day for six months. The group that got the cranberry drink had 68% fewer bladder infections during that period. In this study, the juice was sweetened with saccharin instead of sugar. Other studies have also shown benefit using cranberry juice in bladder infections.
Cranberries help bladder infections because they contain compounds known as proanthocyanidins that prevent bacteria from sticking to the bladder wall. They may also decrease the risk of kidney stones, as well as possibly reducing urine odor.
Significant benefits can be achieved by using 6 to 16 ounces of cranberry juice a day. Because most cranberry juice products have a lot of sugar, which can promote yeast overgrowth and aggravate other symptoms in CFIDS/FMS, I think it is much better to use pure cranberry juice powder in capsule or tablet form. Choose a product that is standardized to contain 11 to 12% quinic acid. The therapeutic dose is one to two capsules a day. You can also use unsweetened cranberry juice and add stevia as a natural sweetener. In general, cranberry juice drinks and cranberry sauce are half as potent as the usual cranberry juice cocktails, fresh or frozen cranberries are four times as potent, pure cranberry juice is four times as potent, and cranberry capsules made from unsweetened cranberry juice powder are 32 times as potent. Over all though, I prefer to use D-Mannose.
D-Mannose
D-Mannose is even more effective for bladder infections than cranberry juice. Mannose is a natural sugar (not the kind that causes symptoms or yeast overgrowth) that is excreted promptly into the urine. Unfortunately for the E. coli bacteria, the fingers that stick to the bladder wall stick to the D-mannose even better. When the patient takes a large amount of D-mannose, it spills into the urine, coating all the E. coli's little "sticky fingers" so that the E. coli are literally washed away with the next urination. The nice thing about the natural approach, as opposed to antibiotics, is that cranberries and D-mannose do not kill healthy bacteria, thereby not disturbing the normal balance of bacteria in the bowel. In addition, D-mannose is absorbed in the upper gut before it gets to the friendly E. coli that are normally present in the colon. Because of this, it helps clear the bladder without causing any other problems. In addition, D-mannose even tastes good.
D-Mannose is quite safe, even for long-term use, although most people need it for only a few days. People who have frequent recurrent bladder infections may, however, choose to take it every day. The usual dose of D-mannose is 1/2 teaspoon every two to three waking hours to treat an acute bladder infection; and 1/4 to 1/2 teaspoon three to four times a day to prevent severe chronic bladder infections. It is best taken dissolved in water. If the patient gets bladder infections associated with sexual intercourse, they can take 1/2 teaspoon of D-mannose one hour before and then just after intercourse to prevent an infection.
The usual cost of D-mannose is approximately $60 for 100 grams and $35 for 50 grams. One-half teaspoon is approximately 2 grams. The patient should feel much better within twenty-four to forty-eight hours on D-mannose. If they don't, check a urine culture (you may want to get the culture at the first sign of infection) and consider antibiotic treatment after two days if the culture is positive. Some evidence exists that the antibiotic nitrofurantoin (also sold under the brand names Furadantin, Macrobid, and Macrodantin) causes less yeast overgrowth than do other antibiotics. Even with other antibiotics, most bladder infections are knocked out by one to three days of antibiotic use, instead of the old seven-day regimen.
Prostatitis
Although women tend to be the ones plagued with bladder infections, men don't get off unscathed. It is very common for men with CFIDS/FMS to have prostatitis, an inflammation or infection of the prostate that is usually seen in younger men between the ages of twenty and fifty. There are three main types of prostatitis:
1. Bacterial prostatitis. This is an acute or chronic infection in the gland that causes prostate swelling and discomfort, and in which an infection can be found by doing a culture.
2. Nonbacterial prostatitis. This is a condition that causes the patient to feel swelling of the prostate with no detectable infection. My suspicion is that it is not uncommon for nonbacterial prostatitis to be associated with yeast overgrowth or other infections that cannot be cultured.
3. Prostadynia. This is a general irritation of the prostate that causes a burning sensation with urination, urinary urgency, and frequency, without any infection or swelling of the prostate. This can come from a number of causes including, I suspect, occult infections and chronic spasm or tightening of the muscles of the pelvic floor.
The symptoms of chronic prostatitis can come and go and be mild or severe. The symptoms include:
* Pain or tenderness in the area of the prostate. It is also common to have burning on the tip of the penis.
* Discomfort in the groin and, occasionally, lower back pain.
* Urinary urgency and frequency with pain on urination.
* Pain with ejaculation.
* In some cases, a slight discharge from the penis. If the discharge is cloudy and larger than one drop, or even a large drop, it is most likely bacterial prostatitis and I would then prescribe antibiotics. If a discharge is present, I would also check to make sure that there is not also a sexually transmitted disease (such as chlamydia or gonorrhea) before beginning treatment.
Severe symptoms, with fever, chills and extreme fatigue, point to acute bacterial prostatitis, requiring treatment with antibiotics. The main medications used for bacterial prostatitis are tetracycline antibiotics (for example, doxycycline [Doryx, Monodox, Vibramycin, Vibra-Tabs]), ciprofloxacin (Cipro), or sulfa drugs (such as Bactrim or Septra DS). Unfortunately, since it is hard for antibiotics to be absorbed into the prostate, symptoms often recur, even after six weeks of treatment. I prefer to use doxycycline or Cipro because these may be effective against other hidden infections that can cause CFIDS/FMS.
Although there are a number of causes of prostatitis, excessive consumption of caffeine, alcohol, and spicy foods can also contribute to the symptoms. Sitting for long periods while traveling (for example, being a truck driver) can also cause irritation of the prostate. Although normal bacteria are the most common causes, some bacteria transmitted through sexual contact can also cause prostatitis. The bioflavonoid Quercetin 500 mg 2 X day has been shown to decrease the symptoms of prostadynia.
Chronic Sinusitus--The Yeasty Beasties Revisited!
Years ago, we speculated that the chronic sinus congestion seen in CFIDS/FMS could be caused by yeast overgrowth. An interesting recent study reported in the Mayo Clinic Proceedings supports this thought. In the study, researchers found that most people with chronic sinus infections had a reaction to fungal growth in their sinuses. They felt that the inflammation was being caused by an immune response (the body's reaction) to the fungus. This research is interesting because more and more studies are showing that treating chronic sinusitis with antibiotics doesn't really do much and that shorter courses of treatment work just as well as the long courses. I find that conservative treatment is more effective than antibiotics for chronic sinusitis.
It's good that medicine is finally starting to catch up with reality. The report in the Mayo Clinic Proceedings noted that "fungus allergy was thought to be involved in less than 10% of cases ... our studies indicate, in fact, fungus is likely the cause of nearly all of these problems and that it is not an allergic reaction but an immune reaction." In this study, the researchers studied 210 patients with chronic sinusitis. Using new methods to collect and test sinus/nasal mucus, they found fungus in 96% of patients.
It's interesting to observe how medical research works. The researchers are now working with different drug companies to set up trials to test medications to control the fungus, but feel that it will be at least two years before any treatments will be available. In my experience, though, these problems often respond dramatically to either Sporanox or Diflucan--which, by no coincidence, are very powerful antifungal agents. Diflucan has now gone generic, and a 6 week course of 200 mg/day can be bought for $60 instead of $600. It is not clear why the researchers did not simply try these medications.
It is important to distinguish between chronic sinusitis, which lasts for over three months, and acute sinusitis, which usually has been going on for a few days and less than a month. For these shorter attacks of sinusitis, bacteria are a more common cause and antibiotics (combined with natural remedies) can be helpful. Some researchers still continue to argue that fungus is not a cause of chronic sinusitis. They note that fungi are seen even in healthy noses, which is correct, but they neglect to discuss the immune changes that are also seen in these noses. Because so many people have responded dramatically to antifungals for the treatment of their chronic sinusitis, my suspicion is that the Mayo Clinic researchers are probably correct.
Three excellent topical treatments for sinusitis are:
1. Sinusitis Nose Spray (Rx) -- By prescription from Cape Drug (800-248-5978). Contains Sporanox, Xylitol, Bactroban, Beclamethasone and Nystatin. Use 1-2 sprays in each nostril twice a day for 6-12 weeks. If it irritates the nose, use nasal saline spray just before using the prescription. Use with silver spray below.
2. Nasal silver spray -- 5-10 sprays in each nostril three times a day for 7-14 days until the sinusitis resolves (from www.EndFatigue.com. Wholesale from www.natural-immunogenics.com or 888-328-8840)
3. Nasal Irrigations (Rx) -- Get 1 liter of normal saline with 100mg Amphotericin B and a second liter with 80mg gentamycin. Use 1 ounce of each in each nostril as a nasal rinse twice a day as needed. By prescription from Cape Drug (800-248-5978) or other compounding pharmacies. Amphotericin B and gentamycin will precipitate if combined in the same bottle.
The patient's lowered defenses play a large role in CFIDS/FMS. The good news is that by treating the many underlying infections common in CFIDS/FMS and by treating any sleep, yeast infections (to be discussed soon), hormonal and nutritional deficiencies, you can bring their immune system back to a healthy state!
by Jacob Teitelbaum, MD
Jacob Teitelbaum MD is director of the Annapolis Center for Effective CFS/Fibromyalgia Therapies, which sees patients with CFS/FMS from all over the world (410-573-5389; www.EndFatigue.com) and author of the best selling book From Fatigued to Fantastic! and Three Steps To Happiness! Healing Through Joy. His newest book Pain Free 1-2-3! has just been released. He gives workshops on effective CFS/Fibromyalgia therapies and pain management for both prescribing and non-prescribing practitioners (see www.EndFatigue.com). He accepts no money from any company whose products he recommends and 100% of his royalties for products he makes is donated to charity.
COPYRIGHT 2004 The Townsend Letter Group
COPYRIGHT 2004 Gale Group