Brush up on the most common lid conditions that plague contact lens wearers.
When examining and treating contact lens wearers who present with various problems, some of us tend to focus on symptoms, lenses and acute corneal signs. In many cases, however, recognizing and treating an underlying lid disease can prove just as important. This article discusses a number of the more common lid disorders that can affect a contact lens wearer's success.
IDENTIFYING A COMMON CULPRIT
Changes in tear film quality can produce many dry eye related symptoms in contact lens wearers. Meibomian gland dysfunction (MGD) is probably the number-one source for evaporative dry eye problems. Evaporative tear problems can cause symptoms such as end-of-the-day dryness; decreased wearing time; smeary or blurred vision affected by blinking; dryness when reading or using the computer; or generally decreased lens tolerance.
MGD is characterized by swollen or congested meibomian gland openings; mounding or capping of the gland openings; thickening of the meibomian secretion (meibum); and congestion, stagnation and stasis of the meibum. Upon expression of the gland with digital pressure, the normally clear, vegetable oil-like secretion may appear cloudy, thickened or even absent in MGD. Chronic meibomian stasis may cause thickening of the posterior lid margin, an increasingly irregular contour to the posterior lid and the appearance of a red line or rim to the most posterior aspect of the lid margin. This red rim consists of many small, telangiectatic vessels, which you may appreciate more with a red-free filter during slit lamp examination. These vessels may blanch slightly when applying digital pressure to test for meibomian gland stasis. Their presence is highly suggestive of chronic MGD.
Experts generally believe that meibomitis is the most common cause of MGD, although senile meibomian gland changes and seborrhea of the gland can lead to MGD too. According to Caroline & Kame (1994), the condition becomes more common as individuals age, with roughly 40% of adults having some extent of MGD. MGD doesn't appear to be related to gender, allergic history or contact lens wear.
TREATING MGD
Patients must understand that MGD is a chronic condition and that successful treatment requires developing consistent lid hygiene procedures as a routine. Explain that treatment won't cure or eliminate MGD, but it can help manage the condition for the long term.
Treatment first consists of warm compresses to closed eyes to liquefy the meibum and soften any debris or matter around the lashes or near the gland openings. Suggest five- to 10-minute soaks with a warm cloth. Recommend that the patient apply these compresses two to four times each day when the condition is problematic and once each day as maintenance treatment.
After the warm soaks, advise the patient to perform a mild lid massage to help break up clumps or strands of the thickened meibum. He may also apply slight pressure to the gland opening to encourage expression of gland contents.
Next, have the patient perform gentle lid scrubs to keep the lid and lashes clean and free from matter. He may use any available commercial eyelid scrubs, add a drop or two of baby shampoo to a clean cloth or just use the edge of a wet cloth to lightly rub the lids and lashes. The key is to keep the routine simple and relatively quick to encourage long-term compliance.
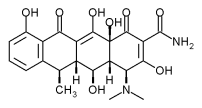
If lid hygiene alone isn't sufficient, then you may want to employ the use of systemic antibiotics (tetracyclines). A standard therapy includes 100 mg doxycycline (Doryx, Monodox) b.i.d. for two to four weeks. It's ideal for patients to take doxycycline with food but not with milk, and pregnant women shouldn't take this drug.
Some practitioners will continue doxycycline once a day for another two to three weeks, while others prescribe a second course like the first but separated by a three-week break. It appears that the treatment is beneficial not as an anti-bacterial, but as it acts more to inhibit bacterial enzymes and might have an anti-inflammatory effect in the glands.
ALTERNATIVE MGD TREATMENTS
Lower doses (50 mg or 20 mg) of doxycycline may also prove effective in treating MGD. While sub-clinical for bacterial infection, the lower dosage may provide the same non-antibacterial effects discussed previously and may prove safer and better tolerated in the long term by patients.
Reports indicate that topical cyclosporine (Restasis) may also effectively treat MGD. Its anti-inflammatory action may help limit meibomitis, as do other anti-inflammatories such as topical steroids. The chronic nature of MGD has made steroids a less attractive option because of their side effects, but they may play a short-term role in recalcitrant cases. Low-dose and/or safer forms of topical steroids may find more of a role in treating MGD, particularly if used in conjunction with cyclosporine during the two- to three-month period it takes for the cyclosporine to demonstrate an effect.
MGD causes tear film instability because of the altered or absent lipids, therefore tear supplements that attempt to specifically replace these lipids may prove effective in decreasing the symptoms of MGD.
Recent research (Sullivan & Schaumberg, 2003) suggests that androgen deficiency and hormone replacement therapy may be a factor in the development of MGD in women. As this role becomes better understood, treatments such as topical androgen may prove effective for MGD.
MEETING MOD'S RELATIVES
A number of systemic conditions are associated with relatively high incidence of MGD. That's why, after diagnosing MGD, it's important to look for any related or underlying systemic condition such as:
* Rosacea. More than 50% of rosacea patients have some degree of MGD. Look for signs of facial erythema and telangiectasis, especially in the forehead, nose and cheeks.
* Seborrheic dermatitis. A chronic disorder that mainly affects adult males and has a significant association with MGD. Features to note are scales or oily red patches of skin around the eyebrows, on the eyelids, beside the nose, behind the ears or on the scalp. They may also have a seborrheic form of anterior blepharitis. If detected, consider comanaging the patient with a dermatologist.
* Accutane therapy. Ironically, this common dermatological treatment for acne carries a high incidence of MGD. You also need to educate these generally younger people, who have a higher likelihood of being contact lens wearers, on the importance of adherence to a rigorous lid hygiene regimen.
* Chlamydial infection. Sometimes referred to as inclusion conjunctivitis, chlamydial infections can include MGD as a component. These infections most often occur in younger persons of sexually active age and may present with a low-grade, persistent conjunctivitis. Look for mild conjunctival redness; tearing; mild irritation and photophobia; and lower palpebral follicles. Some cases may present with symptoms of contact lens related dryness only, and detection of MGD and other signs of chlamydia may lead to earlier diagnosis and treatment of their systemic disease.
Now that we've covered the most common lid disorder and its related conditions, we'll move on to other lid disorders that may affect contact lens wearing success.
BEATING BLEPHARITIS BLUES
Anterior blepharitis generally affects the area around the base of the eyelashes. Typical signs include an accumulation of material around the base of the lashes and inflammation of the lid margin. If it progresses, then flaky collars around lashes, harder crusts and even ulceration and bleeding can occur, and you may also note a loss of lashes and broken lashes. Staphylococcal and Seborrheic are two types of anterior blepharitis, Staphylococcal being the most common.
* Staphylococcal blepharitis. Treatment of Staphylococcol blepharitis consists of the lid hygiene procedures discussed above with the addition of topical antibiotics. Prescribe warm soaks and lid scrubs and an antibiotic ointment such as bacitracin or erythromycin for use on the lid at bedtime. Instruct patients to repeat the warm soak and lid scrubs in the morning to remove any matter and any remaining ointment. If the case is severe, then have the patient reapply a small amount of ointment to the lid margin (this tends to blur vision at least somewhat when used during waking hours).
* Seborrheic blepharitis. This form is characterized by yellowish, greasy scales that seem to adhere to the sides of eyelashes. Treatment is again lid hygiene, but possibly using one of the commercially available shampoos specific for seborrhea on the cloth for lid scrubs. These patients may also benefit from a seven- to 10-day course of bacitracin ointment to treat mixed forms of blepharitis, which frequently include a bacterial component.
Conditions that make the tear film less stable can lead to complaints of dryness, scratchiness and filminess in contact lens wearers.
BLEPHARITIS AND CL WEAR
In addition to dry eye symptoms, lid disease may play a role in other contact lens related complications, such as the following:
* Contact lens induced acute red eye (CLARE) involves sudden onset pain and photophobia, tearing and limbal and bulbar hyperemia. Usually corneal infiltrates in the peripheral or mid-peripheral cornea are present and the condition is generally associated with sleeping while wearing contact lenses. While believed to be an acute inflammatory reaction to toxins/endotoxins trapped beneath the contact lens, the presence of lid disease may increase the material under the lens that triggers the reaction.
Treatment aims mainly to remove the lens, but often includes antibiotic-steroid drops and should also include careful evaluation and treatment of any concurrent lid disease.
* Contact lens peripheral ulcer (CLPU) involves a round, dense non-central corneal infiltrate with an overlying break in the epithelium. While an inflammatory event, bacterial contamination on or trapped under the contact lens may play a role in triggering the response. Treatment needs to first protect against the possibility of an infectious ulcer (fluoroquinolones), but you may try a topical steroid to treat the infiltrate. Both CLPU and CLARE have a tendency to recur, again suggesting that chronic conditions such as lid disease may play a role, and treatment should probably include good lid hygiene.
* Epithelial splits or superior epithelial arcuate lesions (SEALs) are thin arcuate erosion-like lesions in the superior cornea in the area covered by the upper lid. Thought to be mainly mechanical in origin, though probably a more complex etiology, at least one report suggests treatment of upper lid blepharitis can lessen SEALs occurrence. It's possible that the improved lid hygiene lessens the material held against the cornea by the lens and upper lid, or that it decreases lid thickening so the lid does not push the lens down as firmly. Generally, SEALs is treated by lens changes, but keep lid disease in mind as well.
* Giant papillary conjunctivitis (GPC). Reports have implicated MGD as a factor in some GPC (more on this condition below). Therefore, if MGD is present when managing GPC, include an evaluation and treatment of MGD.
GETTING TO KNOW GPC
GPC involves the upper tarsal conjunctiva and is characterized by papillae of varying sizes, hyperemia and increased mucous production. Symptoms include itching, especially marked after lens removal, ropey discharge and increased lens movement or displacement with the blink. GPC is mainly associated with soft lenses, but GP lenses and the presence of exposed ocular sutures can also cause it. Experts believe that GPC is mainly caused by a hypersensitivity reaction, but mechanical irritation can also be a factor.
TREATING GPC
Because the upper tarsal conjunctiva is rubbing across the surface of the contact lens, the cleaner the surface, the less likely to induce a GPC reaction. Therefore, treatment involves keeping the lens surface as clean as possible through improved lens care, or more often by frequent lens replacement. GPC has lessened with more frequent replacement of lenses, and is also less when lenses are not worn overnight.
Frequent replacement of lenses will not prevent GPC in all cases, as even daily lens replacement patients can still have problems. When more aggressive treatment is required, mast cell stabilizers are used to lessen the immune reaction. If the condition is severe, initial treatment may also include topical steroids or topical antihistamine. Once the condition is quieter and the lid hyperemia lessens, mast cell stabilizers alone may be used for maintenance.
In cases where the GPC is localized, you may consider a mechanical component. The location and configuration of a lens edge, edge stand-off, or a stiff lens may all be implicated, and changes to the lens fit or design may alleviate the GPC.
CONSIDER OTHER POSSIBILITIES
The following are a few other lid conditions that affect contact lens wearers:
* Cosmetics can affect lid cleanliness, and possibly occlude gland openings. Cosmetics also can trigger allergic reactions, causing lid edema. Treatment is to eliminate the offending cosmetic and provide acute allergy therapy.
* Lid-surfacing problems. Palsies, lid retraction, lower lid laxity, ectropion and cosmetic eye lid surgeries can all cause greater exposure and incomplete surface wiping on blinks. Treatment is mainly tear replacement, or in some cases surgery, but you must rule out problems such as seventh nerve involvement.
* Lid-wiper epitheliopathy. Donald Korb described this condition as the area on the underside of the upper lid that physically contacts the front lens surface becomes abraded. Diagnosis is based on fluorescein and rose bengal staining of this "lid-wiper" area, seen with lid eversion. The condition is more common in patients who have dry eye symptoms, but no specific treatment has been suggested.
TAKING A LESSON WITH YOU
So remember, the next time a contact lens patient presents with a problem, rule out an underlying lid condition before you focus too much on his signs, symptoms and lenses. Doing so could save you time and your patient further discomfort.
BY NEIL A. PENCE, O.D., F.A.A.O., AND DEAN A. VANNASDALE, O.D.
Dr. Pence is a member of the faculty at Indiana University School of Optometry. In addition to teaching responsibilities, he has directed the Contact Lens Research Clinic and conducted numerous clinical investigations. Currently, Dr. Pence serves as chair of the Association of Optometric Contact Lens Educators (AOCLE).
Dr. VanNasdale is a graduate of the Michigan College of Optometry. He currently holds the Contact Lens Residency position at Indiana University School of Optometry.
Copyright Boucher Communications, Inc. Feb 2004
Provided by ProQuest Information and Learning Company. All rights Reserved