Failure of weaning from mechanical ventilation in COPD patients is often related to diaphragmatic fatigue. Whether there is a central respiratory drive fatigue and a reserve of excitability is still debated. The purpose of this study was to analyze the following in 13 COPD patients weaned from mechanical ventilation: (1) ventilatory (VE/[PETCO.sub.2]) and neuromuscular (P0.1/[PETCO.sub.2]) response to hypercapnia; (2) the maximum reserve capacity measured through changes in the VE/[PETCO.sub.2] and P0.1/[PETCO.sub.2] slopes after doxapram (DXP) infusion, which, given during the test, allows measurement of the maximum response capacity to overstimulation; and (3) analyze the influence of these changes on the outcome of weaning. The results show a variable P0.1/[PETCO.sub.2] response and a low VE/[PETCO.sub.2]. DXP infusion does not change the slopes of these relations but increases the end-expiratory volume ([DELTA]FRCd); (p < 0.02). Since there was no change in the VE/[PETCO.sub.2], P0.1/[PETCO.sub.2], and [DELTA]FRC values with or without DXP, there was no excitability reserve in patients who were successfully weaned. When weaning failed, DXP did not change VE/[PETCO.sub.2] and P0.1/[PETCO.sub.2] slope, but [DELTA]FRCd was greater the [DELTA]FRC (p < 0.001). The excitability reserve in these patients leads to an increase in end-expiratory volume, probably worsening the diaphragm dysfunction.
Weaning from mechanical ventilation is a difficult period for patients with chronic obstructive pulmonary disease (COPD), with occasional successes and failures. Failure is generally related to a peripheral cause, diaphragmatic fatigue,[1,2] or left ventricular dysfunction.[3] These peripheral causes, linked to the switch to spontaneous ventilation, increase the respiratory centers' stimulation from chemoreceptors and mechanical receptors. But the peripheral origin of fatigue cannot account on its own for the precocious increase in respiratory rate shown by some patients at the disconnection from the ventilatory[4] or the late collapse of minute ventilation and respiratory rate[5] minutes before the patient is put back on the ventilator. Questions remain about the intricate relations with the central factor: does the intensity of the central response to hypercapnia and hypoxia have an effect on the outcome of weaning? Have hyperstimulated centers reached their maximum stimulation?
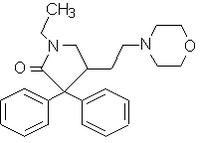
The purpose of this study was to analyze the following in COPD patients weaned from mechanical ventilation: (1) ventilatory and neuromuscular response to hypercapnia; (2) the change in [CO.sub.2] response after a short infusion doxapram (DXP), a respiratory stimulant drug which, in small doses, acts primarily on the peripheral chemoreceptors;[6,7] thus, this stimulation with DXP, together with hypercapnia stimulation, produces an overstimulation that allows measurement of maximum response capacity (MRC); and (3) analyze the influence of these changes on the outcome of weaning.
MATERIALS AND METHODS
Patients
Thirteen patients (seven men, six women) aged 58 to 74 years (67.5 [+ or -] 6.5 years), with COPD gave their informed consent. All had a long history of chronic bronchitis and were regularly treated in the unit. Functional tests performed within four months before or after decompensation confirmed the acute obstructive syndrome. Current hospitalization was due to a bacterial infection requiring mechanical ventilation. All patients had long-term tracheostomies. Medication included feeding through a nasogastric tube, macrolides and subcutaneous heparin. Theophylline therapeutic dosage was not changed during the study. No patient was given corticoids during the stay in the intensive care unit (ICU) or inhaled bronchodilator agents during the protocol.
Method
The automated method used to determine breathing pattern and occlusion pressure at 100 ms was described earlier.[8] Changes in FRC ([DELTA]FRC) were evaluated through changes in the end-expiratory volume, measured by respiratory inductive plethysmography (RIP; Respitrace) and quantified with the deviation of the baseline tidal volume signal.[9,10] Blood gas values were measured with an apparatus (Corning). Hypercapnia response was measured through neuromuscular response (P0.1/[PETCO.sub.2]) and ventilatory response (VE/[PETCO.sub.2]) with the Read method.[11] The end-expiratory [CO.sub.2] pressure ([PETCO.sub.2]) is permanently monitored (HP-78345). The MRC [TABULAR DATA OMITTED] was evaluated by taking the same measurements after infusion of doxapram, a respiratory analeptic that in small doses produces selective stimulation of peripheral chemoreceptors.[6,7]
Protocol
Our study was started during a weaning attempt that had begun 4 h earlier. Patients receiving oxygen therapy (2 L.min-1 by cannula) presented the following weaning criteria: maximum inspiratory pressure [is greater than or equal to] 20 cm [H.sub.2O], tidal volume (VT) > [10 ml.kg.sub.-1], cardiovascular stability, [PaO.sub.2] > 50 mm Hg. Oxygen therapy was stopped for 15 min and baseline measurements of the respiratory pattern were made. If the listed weaning criteria were not met, patients were placed back on mechanical ventilation and retested later. Recordings dealt with two series of three rebreathing tests, one without DXP (VE/[PETCO.sub.2]; P0.1/[PETCO.sub.2]; [DELTA]FRC), the other after a continuous infusion of DXP (VEd/[PETCO.sub.2V]; P0.1d/[PETCO.sub.2]; [DELTA]FRCd), dosage 0.05 [mg.kg.sup.-1.min.sup.-1. A 30-min pause separated each test to allow a return to the baseline state (15 min with [O.sub.2], 15 min in ambient air). Constant monitoring of ECG and arterial pressure was performed by another member of the team for the duration of the study. Reinstitution of mechanical ventilation within the 24 h following the study was defined as a weaning failure and was performed if any one of the above criteria was not met.
Statistical Analysis
Results are given with mean [+ or -] SD, variation percentage of values recorded without DXP, and variation coefficient (VC = SD/M). Student's paired t test and analysis of variance were used for comparison of data. Patients were separated into two groups according to the weaning outcome prognosis. Comparisons between successes (n = 7) and failures (n = 6) were made using Mann-Whitney's nonparametric test.
RESULTS
During the study, no patient showed cardiovascular or neurologic change and none of them required reinstitution of mechanical ventilation.
Results are shown in Tables 1 and 2. In a baseline state, ie, before rebreathing tests, breathing ambient air (15 min), patients were hypoxic ([PaO.sub.2] = 40 [+ or -] 7.2 mm Hg; ext: 24 to 50) with variable hypercapnia ([PaCO.sub.2] = 46.9 [+ or -] 6.3 mm Hg; ext = 38-64; P0.1 average was high but with strong intraindividual variations (7.9 [+ or -] 3.1 cm [H.sub.2O], ext: 2.3 to 14.4; VC = 0.39).
During rebreathing tests without DXP, there was a strong variability in the P0.1/[PETCO.sub.2] and VE/[PETCO.sub.2] slopes among all patients; the lung volume increased to 311 [+ or -] 93 ml. DXP did not significantly increase the P0.1/[PETCO.sub.2] and VE/[PETCO.sub.2] slopes, but it increased [DELTA]FRC (p < 0.02). There was no correlation between VE/[PETCO.sub.2] and VEd/[PETCO.sub.2] values on the one hand (r = 0.02), or between P0.1/[PETCO.sub.2] and P0.1d/[PETCO.sub.2] values on the other hand (r = 0.07), but the lower the P0.1/[PETCO.sub.2] was, the higher the increase of MRC (P0.1d/[PETCO.sub.2])(r = -0.55; p < 0.05). The P0.1/[PETCO.sub.2] and P0.1d/[PETCO.sub.2] slopes on the one hand, and [DELTA]FRC on the other, were not correlated to baseline P0.1. There was a correlation between [DELTA]FRC and [DELTA]FRCd (r = 0.87; p < 0.01) and the higher P0.1/[PETCO.sub.2] was, the higher the increase of [DELTA]FRC.
No significant difference was found between success and failure of weaning trials, whether in the baseline ventilatory pattern, the duration of mechanical ventilation, or the number of weaning trials before the study (Table 2). Patients who failed weaning showed lower VE/[PETCO.sub.2] and P0.1/[PETCO.sub.2] responses than those who succeeded, but the difference was not significant; the increase in [DELTA]FRC was stronger in patients who failed to wean (p < 0.01). The two groups showed no difference in VEd/[PETCO.sub.2] and P0.1d/[PETCO.sub.2] responses, but the increase in [DELTA]FRCd was higher than [DELTA]FRC in those who failed to wean, whereas successfully weaned patients showed no difference between [DELTA]FRC and [DELTA]FRCd (Fig 1).
DISCUSSION
The results of this study bring out the following findings: (1) Response to hypercapnia is generally weak in COPD patients weaned from mechanical ventilation but there are strong individual differences. [TABULAR DATA OMITTED]
(2) The respiratory centers can still be stimulated, as shown by the increase in P0.1d/PETCO2 in some patients, but this "overstimulation" causes an increase in the end-expiratory volume. (3) The neuromuscular and ventilatory response to hypercapnia with and without DXP does not allow prediction of the weaning outcome, but the increase of [DELTA]FRC and [DELTA]FRCd is stronger in those patients who failed to wean.
The respiratory output was measured according to the pressure in the airways during the first 100 ms of an occluded inspiration (P0.1);[12] however, for constant phrenic activity, P0.1 is affected by the power of diaphragmatic contractility and most of all by the changes in pulmonary end-expiratory volume.[13] We measured FRC variations by recording the deviations of the tidal volume signal baseline value by RIP.[10,14,15] This method had been validated in COPD patients during recording of weaning trials.[16] The short infusion of DXP during hypercapnic stimulation while performing a rebreathing test allowed us to check the response capacities to an overstimulation of the respiratory centers. With a 0.05 [mg.kg.sup.-1.min.sup.-1] DXP dose, stimulation is exerted on the peripheral chemoreceptors and produces an increase of VE and VT with no change in respiratory rate.[6]
In our study, the values of ventilatory response to [CO.sub.2] are low. The depression in the [CO.sub.2] ventilatory response in COPD patients is well known and is linked with bronchial obstruction and mechanical alteration. Despite the wide interindividual variability, our results are lower than those obtained in steady-state COPD,[17] probably because of the respiratory decompensation and mechanical aggravation. The neuromuscular response values were small as well but that does not necessarily account for a decrease in central drive, although COPD patients are totally unable to increase central drive when subject to an added inspiratory load.[8,18] The reduction in P0.1 response depends on the FRC increase during the trial and FRC variations are registered when breathing a mixture enriched with [O.sub.2] or [CO.sub.2].[19]. However, we did not find any correlation between [DELTA]FRCd and P0.1/[PETCO.sub.2] and the wide variability of P.01 values indicates [CO.sub.2] responders and nonresponders. Herein, VE/[PETCO.sub.2] did not increase with DXP, which indicates a mechanical impossibility to respond to "overstimulation." The average P0.1/[PETCO.sub.2] response did not change, but individual responses showed significant differences. There was a negative correlation between P0.1/[PETCO.sub.2] and P0.1d/[PETCO.sub.2]: patients showing a weak response without DXP will increase the relation slope with DXP; this shows the maximum response capacity in these patients. Nevertheless, the increase was limited by the pulmonary volume increase: [CO.sub.2]-responders without DXP will show the greatest increase in pulmonary volume with DXP stimulation. Besides, patients with the highest increase in pulmonary volume without DXP will also have the greatest increase under DXP, which demonstrates the bad working conditions of the diaphragm in those patients. Thus, their respiratory centers were still excitable, but the stimulation resulted only in an increase of the pulmonary volume, which is why the P0.1/[PETCO.sub.2] slope did not change and the ventilatory response was weak.
Weaning from mechanical ventilation is a long and difficult period for a COPD patient and failures to wean are generally related to peripheral origin, diaphragmatic fatigue, and left ventricular dysfunction.[1-3] As regards failures to wean, Tobin et al[20] reported a precocious increase in respiratory rate with rapid shallow breathing as soon as the ventilator was disconnected. The observation of paradoxic breathing, proposed as a clinical sign of fatigue, is rather a sign of an inspiratory resistive load than of fatigue.[21] In a previous study,[8] we showed that COPD patients being weaned from mechanical ventilation show different compensation mechanism when subject to small inspiratory resistive loads: some of them succeed in maintaining tidal volume by increasing inspiratory time. Thus, they maintain alveolar ventilation and wean successfully. Others, not ready to stand weaning, cannot compensate and develop shallow breathing. Thus, faced with peripheral stimulation, the respiratory centers can adjust their response. Several authors suggested valuation of the central drive by measuring P0.1 and its changes during the weaning attempts[22,23]: weaning failures present a high P0.1 or an increasing P0.1 after disconnection, which shows an intense respiratory effort leading to fatigue and to the failure of weaning. Montgomery et al[24] showed that the neuromuscular response was stronger in patients who failed to wean than in those who succeeded. Amaha and Sha[25] showed a progressive increase of the ventilatory response to [CO.sub.2] with clinical stabilization and no later decompensation. However, as the changes in FRC are not evaluated in these studies, P0.1 changes must be analyzed with precaution. Our study was performed on patients who had been weaned for 4 h; there was no difference in ambient air among P0.1, P0.1/[PETCO.sub.2], and VE/[PETCO.sub.2] values for the two groups. In the failure group, however, the increase in FRC was stronger than in the successful group, which would indicate a less efficient neuromusculoventilatory transmission and an aggravation of the auto-PEEP phenomenon.[15] This hypothesis was confirmed with DXP: the P0.1d/[PETCO.sub.2] and VEd/[PETCO.sub.2] slopes remained unchanged but the pulmonary volume showed a marked increase. Thus, in patients who failed to wean, peripheral chemoreceptors are more sensitive to a DXP stimulation that raises the excitability threshold during the reinhalation trial. The hypoxic-type sensitivity stimulates the respiratory activity, but ventilation cannot increase because of adverse mechanical conditions and the pulmonary volume in turn worsens the diaphragm dysfunction. Conversely, in patients successfully weaned, DXP did not infer any significant change in P0.1d/[PETCO.sub.2], VEd/[PETCO.sub.2], and [DELTA]FRC. We suggest two hypotheses: (1) the respiratory centers have reached their maximum stimulation level and any further stimulation is without any effect, and (2) there is an alteration in the structure of chemoreceptors related to the strong stimulation of decompensation or, on the contrary, related to mechanical ventilation and suppression of all stimulation. Whatever the hypothesis, the absence of response is welcome because it does not infer an increase in the end-expiratory volume and of respiratory work, which allows the weaning to succeed.
In conclusion, during weaning from mechanical ventilation, COPD patients show depressed respiratory responses with variable neuromuscular responses leading to a distinction between responders and nonresponders to hypercapnia. Doxapram does not change the respiratory and neuromuscular responses, but individual responses are different, according to changes in FRC. During the rebreathing trial, those patients who failed to wean show a greater increase in end-expiratory volume, increased again by DXP; thus, their respiratory center has an excitability reserve but this is of no effect on ventilation because of the end-expiratory volume increase. Moreover, this work confirms the uselessness of respiratory stimulants in COPD patients.
REFERENCES
[1] Fleury B, Murciano D, Talamo C, Aubier M, Pariente R, Milic-Emili J. Work of breathing in patients with chronic obstructive pulmonary disease in acute respiratory failure. Am Rev Respir Dis 1985; 131:822-27
[2] Pourriat JL, Lamberto CH, Hoang PH, Fournier JL, Vasseur B. Diaphragmatic fatigue and breathing pattern during weaning from mechanical ventilation in COPD patients. Chest 1986; 90:703-07
[3] Lemaire F, Teboul JL, Cinotti L, Giotto G, Abrouk F, Steg G, et al. Acute left ventricular dysfunction during unsuccessful weaning from mechanical ventilation. Anesthesiology 1988; 69:157-60
[4] Tobin MJ. Predicting weaning outcome. Chest 1988; 94:227-28
[5] Cohen CA, Zabelbaum GE, Gross D, Roussos C, Macklem PT. Clinical manifestations of inspiratory muscle fatigue. Am J Med 1982; 73:308-16
[6] Burki NK. Ventilatory effects of doxapram in conscious human subjects. Chest 1984; 85:600-04
[7] Scott RM, Whitwam JG, Chakrabarti MK. Evidence of a role for the peripheral chemoreceptors in the ventilatory response to doxapram in man. Br J Anaesth 1977; 49:227-31
[8] Pourriat JL, Lamberto C, Fosse JP, Vasseur B, Cupa M. Steadystate breathing pattern responses to small inspiratory resistive loads in COPD patients. Chest 1988; 95:364-69
[9] Stradling JR, Chadwick GA, Quirk C, Phillips T. Respiratory inductance plethysmography: calibration techniques, their validation and the effects of posture. Bull Eur Physiopathol Respir 1985; 21:317-24
[10] Tobin MJ, Jenouri G, Birch S, Lind B, Gonzalez H, Ahmed T, et al. Effect of positive end-expiratory pressure on breathing patterns of normal subjects and intubated patients with respiratory failure. Crit Care Med 1983; 11:859-67
[11] Read DJC. A clinical method for assessing the ventilatory response to [CO.sub.2]. Aust Ann Med 1967; 16:20-32
[12] Whitelaw WA, Derenne JP, Milic-Emili J. Occlusion pressure as a measure of respiratory center output in conscious man. Respir Physiol 1975; 23:181-99
[13] Grassino AE, Derenne JP, Almirall J, Milic-Emili J, Whitelaw W. Configuration of the chest wall and occlusion pressures in awake humans. J Appl Physiol 1981; 50:134-42
[14] Lennox S, Mengeot PM, Martin JG. The contributions of rib cage and abdominal displacements to the hyperinflation of acute bronchospasm. Am Rev Respir Dis 1985; 132:679-84
[15] Hoffman RA, Ershowsky BS, Krieger BP. Determination of auto-PEEP during spontaneous and controlled ventilation by monitoring changes in end-expiratory thoracic gas volume. Chest 1989; 96:813-16
[16] Tobin MJ, Guenther SM, Perez W, Lodato RF, Mador MJ, Allen SJ, et al. Konno-Mead analysis of ribcage-abdominal motion during successful and unsuccessful trials of weaning from mechanical ventilation. Am Rev Respir Dis 1987; 135:1320-28
[17] Bradley CA, Fleetham JA, Anthonisen NR. Ventilatory control in patients with hypoxemia due to obstructive lung disease. Am Rev Respir Dis 1979; 120:21-30
[18] Altose MD, Kelson SG, Stanley NM, Cherniack NS, Fishman AP. Effects of hypercapnia and flow-resistive loading on tracheal pressure during airway occlusion. J Appl Physiol 1976; 40:345-51
[19] Fitzgerald RS, Garfinkel F, Silbergeld E, Loscutoff SC. Factors in the interpretation of mouth occlusion pressure during measurements of chemosensitivity. Chest 1976; 70 (suppl): 145-49
[20] Tobin MJ, Perez W, Guenther SM, Semmes BJ, Mador MJ, Allen SJ. The pattern of breathing during successful and unsuccessful trials of weaning from mechanical ventilation. Am Rev Respir Dis 1986; 134:1111-18
[21] Tobin MJ, Perez W, Guenther SM, Lodato RF, Dantzker DR. Does ribcage abdominal paradox signify respiratory muscle fatigue? J Appl Physiol 1987; 63:851-60
[22] Aubier M, Murciano D, Fournier M, Milic-Emili J, Pariente R, Derenne JP. Central respiratory drive in acute respiratory failure of patients with chronic obstructive pulmonary disease. Am Rev Respir Dis 1980; 122:191-99
[23] Sassoon CSH, Te TT, Mahute CK, Light RW. Airway occlusion pressure: an important indicator for successful weaning in patients with chronic obstructive pulmonary disease. Am Rev Respir Dis 1987; 135:107-13
[24] Montgomery AB, Holle RHO, Neagley SR, Pierson DJ, Schoene RB. Prediction of successful ventilator weaning using airway occlusion pressure and hypercapnic challenge. Chest 1987; 91:496-99
[25] Amaha K, Sha M. Ventilatory response to [CO.sub.2] in patients after long-term ventilation for acute respiratory failure secondary to chronic obstructive lung disease. Crit Care Med 1981; 9:796-800
COPYRIGHT 1992 American College of Chest Physicians
COPYRIGHT 2004 Gale Group