In 1988, CDC published guidelines for managing patients with suspected viral hemorrhagic fever (VHF)(1). Pending a comprehensive review of the 1988 guidelines, this notice provides interim recommendations that update the 1988 guidelines for healthcare settings in the United States. This update applies to four viruses that cause syndromes of VHF: Lassa, Marburg, Ebola, and Congo-Crimean hemorrhagic fever viruses; although the risk and/or mode of nosocomial transmission differs for each of these viruses, the limited data do not permit clear distinctions.
Background
In Africa, transmission of VHF has been associated with reuse of unsterile needles and syringes and with provision of patient care without appropriate barrier precautions to prevent exposure to virus-containing blood and other body fluids (including vomitus, urine, and stool). The risks associated with various body fluids have not been well defined as most caregivers who acquired infection had multiple contacts with multiple fluids. Epidemiologic studies of VHF in humans indicate that infection is not readily transmitted from person to person by the airborne route(1)(2). Airborne transmission involving humans has never been documented and is considered a possibility only in rare instances from persons with advanced stages of disease (e.g., one patient with Lassa fever who had extensive pulmonary involvement may have transmitted infection by the airborne route)(3). In contrast, investigation of VHF in nonhuman primates (i.e., monkeys) has suggested possible airborne spread among these species (4)(5)(6)(7). Despite uncertainties regarding the applicability to humans of data regarding airborne transmission in nonhuman primates, such information must be considered in the development of infection-control precautions because information regarding exposure and transmission in humans is limited.
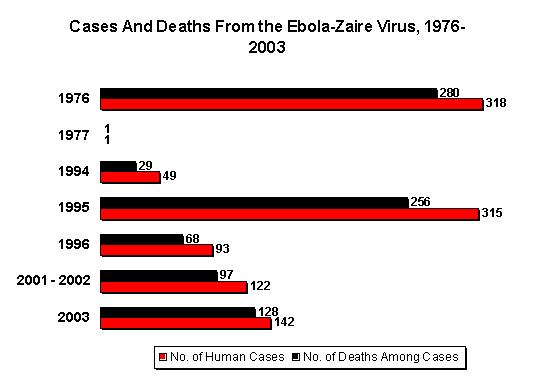
The risk for person-to-person transmission of hemorrhagic fever viruses is highest during the latter stages of illness, which are characterized by vomiting, diarrhea, shock, and often hemorrhage. VHF infection has not been reported in persons whose contact with an infected patient occurred only during the incubation period (i.e., before the patient became febrile; the incubation period ranges from 2 days to 3 weeks, depending on the etiology of the VHF [1]). In the 1995 Zaire outbreak, some instances of Ebola virus transmission within a few days after onset of fever were reported; however, other symptoms in the source patients and the level of exposure to body fluids among these secondary cases were unknown (CDC, unpublished data, 1995). In studies involving three monkeys experimentally infected with Ebola virus (Reston strain), fever and other systemic signs of illness preceded detection of infectious virus in the pharynx by 2-4 days, in the nares by 5-10 days, in the conjunctivae by 5-6 days, and on anal swabs by 5-6 days (P. Jahriling, U.S. Army Medical Research Institute of Infectious Diseases, unpublished data, 1995).
Reporting
All suspected cases of infection with Ebola virus and other hemorrhagic fever viruses should be reported immediately to local and state health departments and to CDC (telephone [404] 639-1511; from 4:30 p.m. to 8 a.m., telephone [404] 639-2888). Specimens for virus-specific diagnostic tests should be sent to CDC as rapidly as possible according to instructions provided when contact is made. General information regarding Ebola virus infection is available through the CDC Ebola Hotline (telephone [800] 900-0681).
Recommendations
The following recommendations apply to patients who, within 3 weeks before on-set of fever, have either 1) traveled in the specific local area of a country where VHF has recently occurred; 2) had direct contact with blood, other body fluids, secretions, or excretions of a person or animal with VHF; or 3) worked in a laboratory or animal facility that handles hemorrhagic fever viruses. The likelihood of acquiring VHF is considered extremely low in persons who do not meet any of these criteria. The cause of fever in persons who have traveled in areas where VHF is endemic is more likely to be a different infectious disease (e.g., malaria or typhoid fever); evaluation for and treatment of these other potentially serious infections should not be delayed.
1. Because most ill persons undergoing prehospital evaluation and transport are in the early stages of disease and would not be expected to have symptoms that increase the likelihood of contact with infectious body fluids (e.g., vomiting, diarrhea, or hemorrhage), universal precautions are generally sufficient (8). If a patient has respiratory symptoms (e.g., cough or rhinitis), face shields or surgical masks and eye protection (e.g., goggles or eyeglasses with side shields) should be worn by caregivers to prevent droplet contact (8). Blood, urine, feces, or vomitus, if present, should be handled as described in the following recommendations for hospitalized patients.
2. Patients in a hospital outpatient or inpatient setting should be placed in a private room. A negative pressure room is not required during the early stages of illness, but should be considered at the time of hospitalization to avoid the need for subsequent transfer of the patient. Nonessential staff and visitors should be restricted from entering the room. Caretakers should use barrier precautions to prevent skin or mucous membrane exposure to blood and other body fluids, secretions, and excretions. All persons entering the patient's room should wear gloves and gowns to prevent contact with items or environmental surfaces that may be soiled. In addition, face shields or surgical masks and eye protection (e.g., goggles or eyeglasses with side shields) should be worn by persons coming within approximately 3 feet of the patient to prevent contact with blood, other body fluids, secretions (including respiratory droplets), or excretions. The need for additional barriers depends on the potential for fluid contact, as determined by the procedure performed and the presence of clinical symptoms that increase the likelihood of contact with body fluids from the patient (8). For example, if copious amounts of blood, other body fluids, vomit, or feces are present in the environment, leg and shoe coverings also may be needed. Before entering the hallway, all protective barriers should be removed and shoes that are soiled with body fluids should be cleaned and disinfected as described below (see recommendation 6). An anteroom for putting on and removing protective barriers and for storing supplies would be useful, if available (1).
3. For patients with suspected VHF who have a prominent cough, vomiting, diarrhea, or hemorrhage, additional precautions are indicated to prevent possible exposure to airborne particles that may contain virus. Patients with these symptoms should be placed in a negative-pressure room (9). Persons entering the room should wear personal protective respirators as recommended for care of patients with active tuberculosis (high efficiency particulate air [HEPA] respirators or more protective respirators) (9).
4. Measures to prevent percutaneous injuries associated with the use and disposal of needles and other sharp instruments should be undertaken as outlined in recommendations for universal precautions (8). If surgical or obstetric procedures are necessary, the state health department and CDC's National Center for Infectious Diseases, Hospital Infections Program (telephone [404] 639-6425) and Division of Viral and Rickettsial Diseass (telephone [404] 639-1511; from 4:30 p.m. to 8 a.m., telephone [404] 639-2888) should be consulted regarding appropriate precautions for these procedures.
5. Because of the potential risks associated with handling infectious materials, laboratory testing should be the minimum necessary for diagnostic evaluation and patient care. Clinical laboratory specimens should be obtained using precautions outlined above (see recommendations 1--4 above), placed in plastic bags that are sealed, then transported in clearly labeled, durable, leakproof containers directly to the specimen handling area of the laboratory. Care should be taken not to contaminate the external surfaces of the container. Laboratory staff should be alerted to the nature of the specimens, which should remain in the custody of a designated person until testing is done. Specimens in clinical laboratories should be handled in a class II biological safety cabinet following biosafety level 3 practices (10). Serum used in laboratory tests should be pretreated with polyethylene glycol p-tert-octylphenyl ether (Triton[R] X-100)(*); treatment with 10 [micro]L of 10% Triton[R] X-100 per 1 mL of serum for 1 hour reduces the titer of hemorrhagic fever viruses in serum, although 100% efficacy in inactivating these viruses should not be assumed. Blood smears (e.g., for malaria) are not infectious after fixation in solvents. Routine procedures can be used for automated analyzers; analyzers should be disinfected as recommended by the manufacturer or with a 500 parts per million solution of sodium hypochlorite (1:100 dilution of household bleach: 1/4 cup to 1 gallon water) after use. Virus isolation or cultivation must be done at biosafety level 4 (10). The CDC mobile isolation laboratory is no longer available (1).
6. Environmental surfaces or inanimate objects contaminated with blood, other body fluids, secretions, or excretions should be cleaned and disinfected using standard procedures (8). Disinfection can be accomplished using a U.S. Environmental Protection Agency (EPA)-registered hospital disinfectant or a 1:100 dilution of household bleach.
7. Soiled linens should be placed in clearly labeled leak-proof bags at the site of use and transported directly to the decontamination area. Linens can be decontaminated in a gravity displacement autoclave or incinerated. Alternatively, linens can be laundered using a normal hot water cycle with bleach if universal precautions to prevent exposures are precisely followed (8) and linens are placed directly into washing machines without sorting.
8. There is no evidence for transmission of hemorrhagic fever viruses to humans or animals through exposure to contaminated sewage; the risk of such transmission would be expected to be extremely low with sewage treatment procedures in use in the United States. As an added precaution, however, measures should be taken to eliminate or reduce the infectivity of bulk blood, suctioned fluids, secretions, and excretions before disposal. These fluids should be either autoclaved, processed in a chemical toilet, or treated with several ounces of household bleach for [greater than or equal to] 5 minutes (e.g., in a bedpan or commode) before flushing or disposal in a drain connected to a sanitary sewer. Care should be taken to avoid splashing when disposing of these materials. Potentially infectious solid medical waste (e.g., contaminated needles, syringes, and tubing) should either be incinerated or be decontaminated by autoclaving or immersion in a suitable chemical germicide (i.e., an EPA-registered hospital disinfectant or a 1:100 dilution of household bleach), then handled according to existing local and state regulations for waste management.
9. If the patient dies, handling of the body should be minimal. The corpse should be wrapped in sealed leakproof material, not embalmed, and cremated or buried promptly in a sealed casket. If an autopsy is necessary, the state health department and CDC should be consulted regarding appropriate precautions (1).
10. Persons with percutaneous or mucocutaneous exposures to blood, body fluids, secretions, or excretions from a patient with suspected VHF should immediately wash the affected skin surfaces with soap and water. Application of an antiseptic solution or handwashing product may be considered also, although the efficacy of this supplemental measure is unknown. Mucous membranes (e.g., conjunctiva) should be irrigated with copious amounts of water or eyewash solution. Exposed persons should receive medical evaluation and follow-up management (1).
Reported by: Hospital Infections Program, Div of Viral and Rickettsial Diseases, and Div of Quarantine, National Center for Infectious Diseases; Office of the Director, National Institute for Occupational Safety and Health; Office of Health and Safety, CDC.
References
(1.)CDC. Management of patients with suspected viral hemorrhagic fever. MMWR 1988; 37 (no. S-3):1--15.
(2.)Baron RC, McCormick JB, Zubeir OA. Ebola virus disease in southern Sudan: hospital dissemination and intrafamilial spread. Bull WHO 1983; 61:997--1003.
(3.)Carey DE, Kemp GE, White HA, et al. Lassa fever: epidemiological aspects of the 1970 epidemic, Jos, Nigeria. Trans R Soc Trop Med Hyg 1972; 66:402--8.
(4.)Dalgard DW, Hardy RJ, Pearson SL, et al. Combined simian hemorrhagic fever and Ebola virus infection in cynomolgus monkeys. Lab Anim Sci 1992; 42:152--7.
(5.)CDC. Update: filovirus infections among persons with occupational exposure to nonhuman primates. MMWR 1990; 39:266--7.
(6.)Johnson E, Jaax N, White, Jahrling P. Lethal experimental infection of rhesus monkeys by aerosolized Ebola virus. Int J Exp Pathol (in press).
(7.)Pokhodynev VA, Gonchar NI, Pshenichnov VA. Experimental study of Marburg virus contact transmission. Vopr Virusol 1991; 36:506--8.
(8.)CDC. Guidelines for prevention of transmission of human immunodeficiency virus and hepatitis B virus to health-care and public safety workers. MMWR 1989; 38:(no. S-6):1--37.
(9.)CDC. Guidelines for preventing the transmission of Mycobacterium tuberculosis in healthcare facilities. MMWR 1994; 43(no. RR-13):33--34, 71--81.
(10.)CDC/National Institutes of Health. Biosafety in microbiological and biomedical laboratories. 3rd ed. Atlanta, Georgia: US Department of Health and Human Services, Public Health Service, 1993; DHHS publication no. (CDC)93-8395.
(*)Use of trade names and commercial sources is for identification only and does not imply endorsement by the Public Health Service or the U.S. Department of Health and Human Services.
COPYRIGHT 1995 U.S. Government Printing Office
COPYRIGHT 2004 Gale Group