The HIV epidemic continues to expand in Africa and beyond, and will continue to infect women as well as men. Tens of millions of people are already infected worldwide, more than a million of them in the United States where about 7,000 HIV-infected women give birth each year.
Yet we have reasons to be optimistic. When it comes to treating the disease, we're nowhere near where we were 20 years ago--or even 10 years ago. In communities with access to care, prognoses have improved significantly. As obstetricians, we now have the tools that allow us to provide effective care for HIV-infected pregnant women and to reduce perinatal transmission. Because of our increasing use of highly active antiretroviral therapy in addition to zidovudine chemoprophylaxis and the appropriate use of elective cesarean section, we now see only a few hundred HIV-infected newborns a year.
We could reduce perinatal transmission even further with two actions: embracing the Institute of Medicine's simple and practical "opt-out" approach to HIV testing, and using rapid screening tests more frequently. The use of a rapid screening test is an important evolving step, or shift, in the management of the HIV-infected pregnant woman. It is vital that these tests be used when necessary during labor.
Once a diagnosis is made, it is our job to guide the patient through the complex but promising process of treatment and monitoring, including, when necessary, the use of resistance testing. To do this, obstetricians can partner with HIV specialists and access up-to-date, practical treatment information online.
'Opt-Out' Testing, Rapid Tests
Many of the infants born HIV-positive today are infected because their mothers were not tested. Perhaps one in nine HIV-infected pregnant women gets minimal or no prenatal care. A significant number of others do not initiate care until the third trimester.
In 1999, the Institute of Medicine recommended an informed right-of-refusal approach to testing.
In this approach, the physician informs the patient that she is going to be tested for the virus that causes AIDS and that she has the right to refuse the test. She can "opt out" by signing a consent form.
That does not mean that there are fewer safeguards with HIV testing. We're still respecting patients' autonomy. In fact, we are more cautious with this test than with other screening procedures that we routinely perform. For example, we don't have individual, informed opt-out policies for breast exams that may detect cancer. HIV infection is treatable. With early diagnosis and therapy, women have decades to live and babies can be free of the disease.
Obstetricians need to put their imprimatur on the test. That's part of our role in caring for pregnant women. If we say, "You don't need this test, do you?" instead of saying "This is a test that's good for everybody," we may as well not offer it. The goal simply put is to have HIV status determined as early as possible in all pregnancies.
The focus most recently among scientific and public health experts has been on rapid HIV tests. The Centers for Disease Control and Prevention has recommended that physicians liberalize the use of rapid screening in labor and delivery suites, emergency departments, and other settings.
These tests should be offered to any woman in labor whose serostatus is unknown. Although not as reliable as the standard approach used for prenatal testing, these tests are sensitive enough to identify HIV-infected women, and the results can be used as a basis for offering treatment while confirmatory tests are performed. Obstetricians should not wait for definitive follow-up tests to begin intrapartum and early neonatal prophylaxis. We can tell patients that if confirmatory tests turn out negative, treatment will be discontinued.
Therapy
If a pregnant woman tests positive, it is the obstetrician's job to monitor her immunologic and virologic status. Studies have shown a direct correlation between viral load and perinatal transmission, with transmission lower at any given viral load if antiretroviral therapy is used.
The viral load also can be used to counsel women about the potential utility of cesarean section: With plasma HIV-1 RNA levels higher than 1,000 copies/mL, cesarean section will reduce rates of transmission. Below that level, the additive benefit of cesarean section, beyond that which can be achieved with highly active retroviral therapy, is less certain.
A lot has changed since 1994, when the Pediatric AIDS Clinical Trials Group reported that zidovudine could reduce the risk for mother-to-child transmission 70%. Current interventions for all HIV-infected individuals focus on early initiation of HAART (highly active antiretroviral therapy)--the term used for the more aggressive and more potent combination antiretroviral regimens that can better suppress viral replication, preserve immune function, and minimize the development of resistance.
Although there are special and complex considerations to be made with regard to the choice of HAART agents in pregnancy, pregnancy per se is not a reason to defer what is now standard therapy.
In pregnancy, zidovudine should still be used whenever possible as a component of HAART regimens. Although it is similar in many ways to other nucleoside reverse transcriptase inhibitors, it has the advantage of demonstrated efficacy in preventing perinatal transmission.
If you don't see a substantial number of HIV-infected women, or if you don't keep up with the ever-expanding body of literature on antiretroviral drugs and patient management, I would advise co-managing your patient with an HIV specialist.
The obstetrician's key role is to ask the consultant what he or she would recommend if the patient were not pregnant, and then to take the lead in evaluating the drugs' benefits, toxicities, and risks. Obstetricians--with their dual roles of optimizing the health of the mother and preventing transmission of the virus to the child, in that order of priority--should be the ones to modify the regimen if necessary.
We often use category C drugs during pregnancy if we know that a drug is much more effective than a category B drug. However, specialists in other disciplines might recommend category B drugs, not because they are better but because of those specialists' unfamiliarity with the care of pregnant women and their fear of using category C drugs. We should be the ones to make that call, and should work with the HIV specialist in balancing efficacy and fetal safety.
The HIV specialists, on the other hand, are going to know all the ins and outs about drug combinations, about acceptable rates of viral load decrease, and about dosing schedules and other logistical details.
In general, the use of two nucleoside reverse transcriptase inhibitors along with a protease inhibitor or a nonnucleoside reverse transcriptase inhibitor is recommended. It also is often useful to choose a regimen that spares one class of antiretroviral agents in case resistance develops. There are choices within each of the three drug categories, but there also are certain medications that should not be used in combination because of overlapping toxicities or diminished efficacy.
There are also certain potential perinatal risks. Nevirapine, for instance, can cause fulminant liver disease in women who have CD4 counts greater than 250 cells/m[m.sup.3]. This drug should be used in pregnant women only if its benefit clearly outweighs the risk.
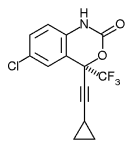
Treatment with efavirenz, for example, should be avoided during the first trimester because the drug has been associated with severe central nervous system anomalies. Overall, it's important to recognize and tell patients that we do not have long-term outcome data on the use during pregnancy of any of the available antiretroviral drugs.
The number of HAART regimens continues to increase, and there may be new reports of problems, so in addition to consulting with HIV specialists, obstetricians should also make use of the Public Health Service's Web site (www.aidsinfo.nih.gov/guidelines). The site provides thorough and regularly updated guidelines on the management of HIV in pregnant women, as well as fact sheets for patients. The perinatal guidelines--last updated in February--cover management broadly but also address the safety and toxicity of individual drugs.
Prevention of Resistance
Once therapy is underway, viral loads should be checked every month until the viral load is undetectable. At that point, monitoring should be done every 2-3 months. If the viral load is not dropping or does not become undetectable within 6 months, a decision about new therapy will have to be made.
Before therapy is stopped, however, your patient must undergo resistance testing--a practice that has become a standard component of HIV care, mainly for identifying therapies that should not be used in the new regimen.
If you stop therapy first and draw blood just a week later, the wild-type virus (the nonmutant strain) may have overgrown a minority mutant strain, and the resistant virus may not be detected. You must draw blood before discontinuing therapy.
Also remember that second regimens do not work as well as first regimens, so it is important to do everything possible to prevent nonadherence. Patients who are only intermittently adherent--who have intermediate drug levels--are more likely to develop resistance.
Be sure to explain at the start that it is critical for the patient to be committed to therapy and to take drugs in a timely fashion. And if a patient develops nausea and vomiting, have her stop her drug regimen until the symptoms subside.
Mode of Delivery
As a rule, women who have scheduled a cesarean delivery before the onset of labor and before rupture of membranes have a lower rate of perinatal HIV-1 transmission. However, for a patient whose viral load is very low, there really is no evidence that scheduled cesarean delivery can lower the risk of transmission.
In addition, there is some preliminary evidence to support the notion that even some patients whose viral load is not that low--plasma HIV-1 RNA levels higher than 1,000 copies/mL--may not benefit from cesarean delivery if they are being given HAART. Those data remain to be confirmed.
Considering all that is known and unknown, I would advise a cesarean section for women whose viral load is greater than 1,000 copies/mL. When a patient's viral load is low, however, I would tell her that there is no proven benefit to delivering surgically.
BY HOWARD L. MINKOFF, M.D.
COPYRIGHT 2005 International Medical News Group
COPYRIGHT 2005 Gale Group