To the Editor:
The Oxford Miniature Vaporizer (OMV) 50 and the Ohmeda Portable Anesthesia Complete (PAC) are the modern draw-over anesthetic vaporizers used to deliver anesthesia in austere and battlefield conditions. These vaporizers are used by the British and American armed forces involved in far forward surgical team (FST) support of military actions. Light weight and rugged draw-over anesthetic vaporizers are considered a mainstay of battlefield anesthetic techniques. Drawover anesthesia is also used in third world countries where logistical and technical support will not allow the use of more conventional anesthesia apparatuses. In austere locations, versatility of manpower and equipment are a must. The Ohmeda PAC augments the versatility of the FST's, allowing the practitioner to deliver a variety of agents: halothane, isoflurane, enflurane or diethyl ether. Any one of these agents can be used depending on its availability.
Most anesthesiologists are not acquainted with drawover anesthesia delivery. In the United States Army the Forward Surgical Teams deployed with each maneuver brigade are equipped with the Ohmeda PAC as the primary anesthesia apparatus. Despite work on a New Field Anesthesia Machine the American and British forces will rely on the drawover technology for the foreseeable future in austere and battlefield medical support operations.
Tighe compared the traditional use of drawover halothane and trichloroethylene in the Triservice Anesthesia Apparatus (TSA) with the use of the newer potent inhaled agent isoflurane while providing field surgical support in Northern Iraq (Operation Desert Storm). He advocated the use of isoflurane as the sole inhaled agent to be used with the TSA in the military environment. This simple change reduces the amount and type of logistical support required for military surgical units. Additionally, the use of a single inhaled agent and one vaporizer in this austere setting is simple and satisfactory. If isoflurane is chosen to be used as the potent inhaled agent primarily and an inhaled induction is desirable, then either another device charged with halothane is required or the drawover device must be emptied and recharged with a different agent.
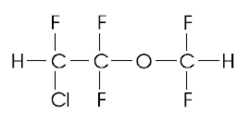
The operating characteristics of the Ohmeda PAC when delivering sevoflurane are quite compatible with the use of a new volatile anesthetic drug, sevoflurane. Sevoflurane has been studied and its characteristics documented elsewhere. Briefly, this fluorinated methyl-ethyl ether has low solubility with a Blood/Gas partition coefficient at 37[degrees] C of 0.69. The rate of rise in alveolar concentration toward the inspired concentration of sevoflurane is surpassed only by nitrous oxide and desflurane. Sevoflurane is stable in storage and requires no additives or stabilizers. Sevoflurane is nonpungent. Lack of respiratory irritability with consequent minimal coughing and laryngospasm allows sevoflurane to be used as an induction agent in addition to its use as a maintenance anesthetic. The cardiovascular effects of sevoflurane seem most similar to isoflurane in that cardiac index is maintained with a mild increase in heart rate. The arrythmogenic potential of sevoflurane is also similar to isoflurane. Despite initial concerns, sevoflurane's renal effects are minimal. Associated elevations of fluoride levels do not seem to be clinically significant due to the speed of sevoflurane's washout. Plyman & Teiken have described the same results we obtained in similar investigation.
Our bench study was conducted to evaluate the output characteristics of the Ohmeda PAC delivering sevoflurane. An Ohmeda PAC anesthesia device was cleared of all volatile anesthetic agent. This was verified by a side-stream sampling of the output with an Ohmeda respiratory gas monitor (RGM) Model 5250. An Ohio V5A anesthesia ventilator was connected to the t-piece at the vaporizer outlet to simulate the controlled ventilation of a patient using the self-inflating bag which is issued with the Ohmeda PAC . The test lung at the patient port of the non-rebreathing valve allowed recoil of the delivered tidal volume to the scavenger tubing at the outlet valve of the non-return valve. The scavenged gases were delivered to a passive scavenging system to prevent any effects on the volume of the gas drawn through the vaporizer. Measurements of vaporizer output were made with the Ohmeda RGM which was zeroed and calibrated as per the operations manual prior to each set of data points collected. Stabilization at each data point to approximately one to two minutes. Output at each data point was observed for an additional three to five minutes; no change in output at any data point occurred after initial stabilization. Data points were obtained in series with minutes ventilations kept constant. The system was allowed to reach zero output for at least five minutes prior to the subsequent series of data points at the new minute ventilation. The room temperature was regulated to + or - 0.3[degrees] C and results are given for 20[degrees] C and 25[degrees] C.
The Ohmeda PAC vaporizer delivered concentrations of sevoflurane in stepwise equal volume percent increases with each subsequent dial position change. Dial positions at the lower end of the scale (A thru D) produced outputs of similar volume's percent within + or - 0.1 volume percent. At position E the range of output was still very narrow 3.2 - 3.7 volumes percent. The highest output dial position resulted in a range of 0.8 volumes percent from lowest to highest output. The higher minute ventilations were associated with the lower outputs at a given dial position. Vaporization of liquid agent probably reduced the temperature of the anesthetic liquid and subsequent amount of vapor produced at the higher minute ventilations. It is interesting to note that the stabilized and recorded output points described in the graphs did not decrease with time for any given data point.
The amount of sevoflurane produced by the Ohmeda PAC is clinically usable. With appropriate dosing of fixed agents, i.e. narcotics, this range of inhaled sevoflurane should allow for more than adequate anesthesia for patients undergoing surgery. Given that most battlefield generated casualties will be dehydrated and somewhat volume deficient from blood loss, the range of sevoflurane available seems appropriate for most scenarios. The rapidity of change of anesthetic depth allowable with a low-solubility agent like sevoflurane would be most suitable for surgical cases conducted in far forward locations. The rate of decline of sevoflurane concentrations after discontinuation would be the quickest available in an austere environment where until now halothane, trichloroethylene and isoflurane have been the agents of choice.
A forward surgical team of twenty to twenty-two people, attached to the trailing end of a maneuver brigade or an airborne task force, will be pushed to the limits of endurance just at the time when lives are at stake. Sevoflurane should allow for speedy return to consciousness in an austere environment characterized by limited monitoring equipment and minimal personnel available to observe post-operative patients. Even small differences in recovery rate in battlefield circumstances might make significant differences in outcomes. Fewer post-operative patients requiring monitoring among the wounded awaiting evacuation will free health-care personnel for other duties. Less post-operative sedation may equate to greater safety from unobserved hypoventilation or apnea.
During a recent MEDRETE to Nepal one of the authors was able to use sevoflurane in conjunction with the Ohmeda PAC. Adult patients were induced using inhaled sevoflurane. Second stage anesthesia was deepened with the use of intravenous lidocaine (1mg/kg). Relaxants were used to facilitate intubation in some cases. We feel that sevoflurane's use as a sole agent for inhaled anesthesia in austere circumstances may be ideal. Further clinical study of this agent using austere or battlefield anesthetic techniques is clearly indicated, especially regarding its use in pediatrics, so often cared for on humanitarian missions.
Paul C. Reynolds, M.D.
Kenneth T. Furukawa, M.D.
To the Editor:
I enjoyed the November Case Report (Military Medicine, 167:956) on possible systemic reaction to topical application of fluorescein dye. However, given the unprecedented nature of Dr. Anderson's claim, greater diligence is due.
I estimate that fluorescein is applied to eyes at least 10 million times per year in the US alone, and has been used at this rate for decades. For Dr. Anderson's case to make medical history, it must meet extraordinarily high standards of scientific rigor. It does not. There are perhaps hundreds of other explanations of equal or greater statistical probability for his patient's symptom complex and examination findings. How do we assure ourselves that this was not merely a chronological coincidence, but actual cause and effect?
I congratulate the author on calling our attention to a theoretical risk, but I remain unconvinced that we have our first reported case of systemic reaction to topical fluorescein.
Col Stephen G. Waller, USAF, MC, FS
To the Editor:
Explosive outbreaks of gastroenteritis in the shipboard environment attributed to Norovirus (formerly Norwalk-Like Virus) have been prominent in the lay literature, with reports of a large outbreak on an aircraft carrier as well as numerous reports involving the cruise ship industry. The Centers for Disease Control and Prevention has been actively engaged responding to the civilian cruise ships. Since last August, routine Navy medical surveillance activities have identified outbreaks on five large deck Navy vessels, with over 2000 personnel seen in the medical departments for symptomatic care. One ship had over 700 total cases, while another had 180 patients present for medical care in one day. Ships' locations spanned the globe, with outbreaks in the Indian Ocean, Pacific, Mediterranean, and U.S. coastal Atlantic waters. These outbreaks have generated significant medical response efforts within Navy medicine. These reports continue to be consistent with previous findings related to shipboard outbreaks from Norovirus agents, with one recent outbreak so far having confirmed Norovirus from stools. While no mortality from these outbreaks has been reported, the associated discomfort has reduced readiness in the affected Navy vessels, especially if they occur in high operational areas, and adversely affected the passengers and crew on the cruise ships.
While perhaps less appreciated than other potential infectious disease threats, these reports document the importance of ongoing research into acute gastroenteritis associated with Norovirus in the shipboard environment, both within the Navy and on large civilian vessels. Since 1999, the DoD Global Emerging Infections System (DoD-GEIS) has supported NEPMU-5 and NEPMU-6 to conduct laboratory-based studies into the causes, frequency, and individual risk factors during viral gastroenteritis outbreaks on large decks. Eleven such outbreaks have been documented and studied to various degrees. This research continues to be important for maintaining readiness of the Navy-Marine Corps team.
CAPT Bruce K. Bohnker, MC, USN(FS)
LCDR Scott Thornton, MSC, USN
To the Editor:
I recently participated in a MEDRET in a Central American country for two weeks as part of my annual training. I had previously participated in two other MEDRETs in South American countries. I was told during my last tour that a surgical MEDRET is being planned for the future. This would involve a surgical team that will be doing operations not requiring an overnight stay. I had the opportunity to be a member of a Forward Surgical Team (FST) in Afghanistan last year.
Based upon my interactions with other members of the FST, I feel that a surgical MEDRET to a third worldcountry is the best annual training a FST can have. The equipment and personnel(20 members) can be transported on two C130 planes or one C141 plane. The mission of an FST is to operate close to the battlefield, under austere circumstances and hold the patients for six hours before transferring them to a higher echelon of care. Each FST has three general surgeons, one orthopedic surgeon and two nurse anesthetists.
The surgical MEDRET could be combined with a medical MEDRET. The medical MEDRET generally spends three to four days in one location and on average sees 1000 patients a day. On the first day in each location, the FST would set up its operating room with one or two operating tables and select patients for operations on the last two days. The team has the capability of doing at least six operations a day. This could consist of hernia repairs and removal of superficial masses. No intra-abdominal operations will be done.
In the present international atmosphere, I believe that the FSTs are going to play an important role in the battlefield in saving the lives and limbs of our soldiers. Therefore, a realistic annual training, by participating in a surgical MEDRET, is the best thing we can do to get the FSTs ready for their wartime mission.
COL Narayan Deshmukh, MC, USAR
To the Editor:
We read with interest the paper of Hirota et al, published in a recent issue of Military Medicine. In this study the authors have determined the prevalence of previous hepatitis A virus (HAV) infection in U.S. Army recruits and concluded, via a cost analysis, that all U.S. military recruits should be vaccinated without evaluation of previous HAV immunity. We would therefore like to present the findings from previous studies carried out in Greece, and contribute further to the discussion of this important subject.
In our seroepidemiological study among 285 males (mean age 24.4 + or - 4.4 years) of a Greek warship, none of the 263 serum samples tested for total (overall subtypes) antibodies to HAV (anti-HAV) were found to be positive. In a study of 200 healthy female recruits serving in the Greek Navy, aged between 17-23 years, 17.5% had evidence of a previous infection of HAV.3
These findings document the remarkable decline in the age prevalence of anti-HAV in the Greek general population which has taken place over the last few decades and indicate that the military personnel of the Greek armed forces are vulnerable to HAV infection. It is widely recognized that not only military warship personnel, but in general, members of the armed forces have an increased risk of exposure to HAV since this population is often faced with situations where satisfactory levels of personal hygiene and sanitation cannot be maintained. Moreover, clinically apparent HAV disease, with both serious health and economic implications, becomes more likely with the increase of age at exposure.2
Therefore, the need to design cost-effective intervention strategies against hepatitis A is obvious and urgent. Until now, prevention of hepatitis A infection for the Greek armed forces was achieved by precautionary measures and passive immunization, and a selective vaccination of military personnel was undertaken before or during operations and visits to foreign countries in which the disease was endemic.
On the basis of the available literature it is unclear whether the early vaccination for children or adolescents, and not the selective vaccination of military personnel, would be a more effective strategy for the elimination of the HAV infection. Further research is needed before a final decision and a universal HAV inoculation program could be recommended. Perhaps this could be accomplished together with the hepatitis B immunization program, which has been implemented for all 12-year-old children from early 1998.
Lt. J.G. (M.C.) Elias E. Mazokopakis, Emmanuel S. Ganotakis, M.D. Christos D. Lionis, M.D.
References are available from Lt. Mazokopakis at the Department of Internal Medicine, University Hospital of Heraklion Crete, P.O. Box 1352, Voutes, 71 110 Heraklion, Crete, Greece
Copyright Association of Military Surgeons of the United States May 2003
Provided by ProQuest Information and Learning Company. All rights Reserved