Let's face it, at one time or another we've all had a blemish or two -- or more. Acne is a common skin condition that usually affects teenagers, although it sometimes continues into adulthood. Most people manage minor pimple outbreaks on their own, but as many as 40% of teenagers have acne severe enough to warrant medical attention.
Acne pimples and scarring can compromise the self-esteem of a teenager. Fortunately, treatments can reduce the appearance and long-term effects of acne. Read on for important tips for getting and keeping clear skin.
Intro to Acne
When a child reaches adolescence, usually between 11 and 14 years of age, his/her body starts producing larger quantities of hormones and the skin glands secrete more oil. These glands and hair follicles can clog with oil, dust, and dirt. Bacteria can grow in the pores, resulting in blackheads, whiteheads, and
pimples. Most teens notice acne on their face and neck, though it can also appear on the back, chest, and upper arms.
The myths that surround acne can add to the embarrassment. In reality, people will get acne even with the best hygiene practices. Don't blame your children for eating chocolate and pizza -- there's no proven link between diet and acne. And while pimples seem to surface on the morning of a big exam or the night of a big date, stress rarely results in an outbreak.
Doctors believe that three factors contribute to acne -- genes, cosmetics, and the environment. Research has shown that family members often share the same type of acne, so if a parent, brother, or sister has acne, chances are other children will too. In addition, some make-up and skin care products clog pores, making acne worse. If your teens are susceptible to acne, look for "noncomedogenic" beauty and skin care products. Environmental factors such as airborne grease at fast food restaurants or any materials that contact your face or other areas may aggravate acne.
To help prevent acne from forming, your children should keep their skin clean and avoid touching the pimples. Your teen should gently wash his/her face and acne-prone areas two to three times a day using any good soap or cleanser. Hard scrubbing can actually make acne worse. Keep hair away from the face. If pimples do form, let them heal naturally. Avoid the temptation to pick or squeeze -- this can aggravate the infection and result in deeper, longer-lasting scars.
See a doctor or dermatologist to discuss your acne treatment options. Treatment can minimize acne before it causes damage and reduce the chance of scarring.
Over-the-Counter Acne Care
Americans spend more than $100 million each year on over-the-counter acne medications. If your teens have mild acne, these products may be enough. It can take several weeks to see an improvement and you may need to try several products to find one that works for them.
Most over-the-counter acne products contain benzoyl peroxide or salicylic acid. They help open clogged pores and may reduce bacterial growth. If the acne doesn't improve within several weeks, consider products with sulfur and resorcinol, such as Clearasil Adult Care. These products have a noticeable color and odor and may cause dry skin.
Some people treat their acne naturally with the herbal products tea tree oil or arnica. Tea tree oil is thought to have antibacterial properties. A study found tea tree oil is less effective -- but less irritating -- than benzoyl peroxide. Arnica has anti-inflammatory properties, but its effectiveness for treating acne has not been confirmed.
Prescription for Clear Skin
Is it time for your teen to see a dermatologist? If he/she is concerned and over-the-counter products don't work, then it's time to talk to a doctor about prescription acne medicines. Doctors recommend medical care for people with deep, painful, or swollen blemishes or with 10 or more blemishes on one side of the face.
Your child's doctor may prescribe an antibiotic solution or gel to apply directly to the skin. Some common prescription antibiotic medicines include clindamycin solution (brand name Cleocin-T) and erythromycin (T-Stat, Emgel). These antibiotics are equally effective and generally well tolerated. Possible side effects include mild skin irritation or dryness.
Other medicines that can reduce acne blemishes include tretinoin (Retin-A), adapalene (Differin), azelaic acid (Azelex), or tazarotene (Tazorac). Tretinoin, adapalene, and azelaic acid reduce blemishes by about 65-70 percent. Tazarotene reduces blemishes by 45-55 percent. Side effects of these products include dry, red, or irritated skin.
If topical creams are not effective, your child's doctor may prescribe oral antibiotics such as tetracycline (Sumycin), minocycline (Minocin), or erythromycin (Eryc, Ery-Tab). Alone, these oral antibiotics reduce lesions by 50 percent. Used in combination with other products, such as benzoyl peroxide, they are up to 88 percent effective. Possible side effects of oral antibiotics include stomach upset and mild diarrhea.
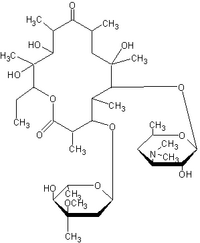
If your teen has severe acne and antibiotics don't help, another option is the oral medicine isotretinoin (Accutane). Accutane reduces the skin's oil production. Blemishes may get worse during the first three weeks, but most cases begin to improve in the first month with full effects in three to five months.
Accutane can have severe side effects and should only be used under the close supervision of a doctor. Women who are pregnant or may become pregnant should never use Accutane since it may cause birth defects.
Many medicines can significantly reduce the appearance and effects of acne. Helping your teen find the right treatment so he/she put his/ her best face forward.
Holly Vance, a clinical pharmacy specialist, has been a member of the drugstore.com team since June, 1999.
COPYRIGHT 2001 Pediatrics for Parents, Inc.
COPYRIGHT 2002 Gale Group