What are the options?
Recent findings about the drawbacks to estrogen (ET) and estrogen/progestin therapy (Combined Hormone Therapy - CHT) make it more difficult than ever to make a rational choice.
When menopause is viewed as a deficiency disease or condition, as it is by some medical practitioners, then it follows that some kind of treatment will be viewed as beneficial to all women approaching menopause. If menopause is seen as a natural stage of biological development, however, hormone therapy will be seen as medication useful only for those most seriously affected (that is, those who have had an artificial menopause, those at serious risk of osteoporosis, and those few women who suffer from intolerable hot flashes). Some people feel that drugs were invented to cushion us from discomfort and stress, and that to spurn such relief is silly. Others feel that we swallow too many drugs without thinking of the consequences, and that sound nutrition and other changes in daily routine should be adopted before resorting to drugs. These differing attitudes influence many decisions about hormone therapy.
ET (or CHT) should be prescribed for a woman only after she has had a thorough medical examination, including not only blood pressure, a pelvic exam, and a Pap test, but also measurement of blood lipids, a clinical breast examination (CBE) and mammogram, and, ideally, a bone density scan. Her doctor will usually insist on a checkup in three months, and every six months thereafter. This means that women on ET or CHT are more likely to have regular medical checkups than women not receiving hormones. Because of this consistent surveillance, including endometrial biopsies, Pap tests, and breast exams, if these women do develop signs of a disease, it is more likely to be caught early.
Thus, if a woman no longer has functioning ovaries, and particularly if the loss of ovaries takes place before the normal age of menopause, ET is probably a sound decision. If loss of sex drive results from oophorectomy, ET with added testosterone may be the only effective therapy. When the ovaries are removed, the uterus is usually removed as well; where mere is no uterus, there is no worry about endometrial cancer. Given the enormously increased risk of osteoporosis to women who go through early menopause as a result of surgery, ET is probably a wise move for at least a few years. (It is also worth noting that oophorectomy significantly reduces the risk of breast cancer.) Similarly, because any form of premature menopause increases the risk of osteoporosis, women who go through an early menopause for any reason might also consider ET or CHT. On the other hand, we have little to no information about the protective effects of a healthy lifestyle - regular vigorous exercise, no smoking, little or no alcohol, a low-fat, high-fiber diet. It is quite possible that these pluses more than make up for the loss of ovarian function. We just don't know.
Women who go through natural menopause but who find hot flashes, night sweats, or associated discomforts absolutely intolerable may choose to take CHT. This is a quality-of-life choice and it should be respected. There is no evidence that taking CHT for a period of less than two years (and perhaps for as long as four years) increases the risk of breast cancer, although it must be borne in mind that the risk of a blood clot, stroke, or heart attack will escalate over that first year of treatment. Some women find that a short course of ET or CHT allows them to overcome the fatigue and emotional stress that makes decision making impossible. Once they are back on their feet, they are in better shape to make other changes in their lives that may help them withstand the stresses of menopause.
The Osteoporosis Risk Profile (see Chapter 6) is a rough guide to bone loss, but this should be verified by a bone scan. If results indicate minimal bone loss, regular vigorous exercise may avert the need for medication. If you prefer not to take estrogen, there are alternatives: three bisphosphonates, alendronate (Fosamax and Novoalendronate), etidronate (Dodrocal) and risedronate (Actonel); and an anti-estrogen (selective estrogen receptor modifier, or SERM) raloxifene (Evista). You can assess the situation using the Risk Profile and confirm this with results from a bone scan. You may decide to try vigorous exercise and be tested again. The decision will vary from woman to woman but the important thing is not to be browbeaten into anything, but to make the decision from a position of informed choice. Women who have a family history of heart attack or stroke, or who suffer from chronic high levels of cholesterol (hypercholesterolemia) may decide to see a cardiologist who may prescribe a statin - Zocor (simvastatin), Mevacor (luvastatin), Pravachol (pravastatin), etc. - to lower cholesterol levels. Bear in mind, however, that cholesterol levels mean less and less as a predictor of heart disease as a woman ages. Recognize that there are other preventive strategies to reduce the risks of stroke, heart attack, and blood clots and explore these with your doctor.
Future Prospects
Now that we have a better understanding of the real drawbacks of hormone therapy, it is time to look forward to new medications that may provide the benefits of hormones (alleviating hot flashes and vaginal dryness, halting bone loss) without the terrible drawbacks (heightened risks of endometrial and breast cancer, blood clots, stroke, and heart attack). The pharmaceutical companies, facing plunging sales and dissatisfied shareholders, are renewing efforts to develop these elusive products. At the same time, new low-dose hormone products are appearing on the market, although there is absolutely no evidence that lower doses will avoid the problems demonstrated with higher doses.
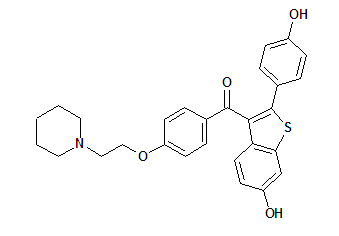
Some pin their hopes on selective estrogen receptor modifiers (SERMs), products developed over the last few decades that mimic some, but not all, of estrogen's effects. Tamoxifen was the first SERM approved by the U.S. Food and Drug Administration (FDA) and Health Canada, and it has been widely prescribed for breast cancer survivors although it is effective for only five years or so. During that time span, it can decrease the risk of a recurrence of breast cancer, but it can cause hot flashes and it significantly increases risks of blood clots, stroke, and uterine cancer. In my view, it is too risky for most healthy women to use. Raloxifene (Evista) is another SERM approved to prevent osteoporosis. In one study, it reduced the number of breast cancer cases in low-risk women but it also increased hot flashes and leg cramps (a potential harbinger of blood clots). Toremifene (Fareston) has properties and side effects similar to tamoxifen but does not seem to increase the risk of endometrial cancer. The FDA restricts the use of this SERM to postmenopausal women with metastatic breast cancer.
The bottom line is that hormone therapy is there to relieve the worst hot flashes and/or night sweats, but that it can reasonably be used only for a very few years. My hope is that, as younger women realize what menopause may mean for them, they will prepare for it by eating well, and exercising regularly and vigorously and that, in the end, they may not need the kind of blockbuster treatments that were so freely administered to their big sisters and mothers.
This excerpt is taken from the 6th edition of Understanding Menopause, by Janine O'Leary Cobb (Key Porter Books, Ltd., 2005) and appears with the permission of the author and publisher.
Janine O'Leary Cobb founded A Friend Indeed in 1984. Four years later, she wrote the groundbreaking book Understanding Menopause (Key Porter), which has been a source of well-researched information and comfort for thousands of women. Following the release of the Women's Health Initiative Study in 2002 regarding the serious health consequences of hormone replacement therapy, Janine has written a sixth edition of her book, which will be coming out in April. Here is an excerpt from the chapter entitled, The Big Question: Hormones.
Copyright Initiatives for Women's Health, Inc. Mar/Apr 2005
Provided by ProQuest Information and Learning Company. All rights Reserved