Flagyl
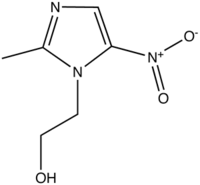
Metronidazole (INN) (IPA: ) is an nitroimidazole antibiotic drug used in the treamtent of infections caused by susceptible organisms, particularly anaerobic bacteria and protozoa. It is marketed by Sanofi-Aventis under the trade name Flagyl, and also by various generic manufacturers. Metronidazole is also used in the treament of the dermatological condition rosacea, where it is marketed by Galderma under the trade name Rozex. more...
Mode of action
Within anaerobic bacteria and sensitive protozoal cells, the nitro group of metronidazole is chemically reduced by ferredoxin (or ferredoxin-linked metabolic process). The reduction products appear to be responsible for killing the organisms by reacting with various intracellular macromolecules by interfering with DNA synthesis.
Indications
Systemic metronidazole is indicated for the treatment of:
- Gram-positive and Gram-negative anaerobic bacterial infections, e.g. Bacillus fragilis
- Protozoal infections, e.g. giardiasis, trichomoniasis
- Pseudomembranous colitis (Clostridium difficile)
- Dental infections, including acute gingivitis
- Intra-abdominal infections
- Aspiration pneumonia
- Lung abscess
- Bacterial vaginosis
- Pelvic inflammatory disease
- Amoebiasis (intestinal and extra-intestinal)
- Surgical prophylaxis
- Eradication of Helicobacter pylori (as part of a multi-drug regimen)
(Rossi, 2006)
Topical metronidazole is indicated for the treatment of rosacea, and has been used in the treatment of malodorous fungating wounds. (Rossi, 2006)
Prevention of preterm births
Metronidazole has also been used in women to prevent preterm birth associated with bacterial vaginosis, amongst other risk factors including the presence of cervicovaginal fetal fibronectin (fFN). A randomised controlled trial demonstrated that metronidazole was ineffective in preventing preterm delivery in high-risk pregnant women and, conversely, the incidence of preterm delivery was actually higher in women treated with metronidazole. (Shennan et al., 2006)
Adverse effects
Common adverse drug reactions (ADRs) associated with systemic metronidazole therapy include: nausea, diarrhoea, and/or metallic taste. Intravenous administration is commonly associated with thrombophlebitis. Infrequent ADRs include: hypersensitivity reactions (rash, itch, flushing, fever), headache, dizziness, vomiting, glossitis, stomatitis, dark urine, and/or paraesthesia. (Rossi, 2006)
High doses and/or long-term systemic treatment with metronidazole is associated with the development of furry black tongue, leukopenia, neutropenia, increased risk of peripheral neuropathy and/or CNS toxicity. (Rossi, 2006)
Common ADRs associated with topical metronidazole therapy include local redness, dryness, and/or skin irritation; and eye watering (if applied near eyes). (Rossi, 2006)
Interaction with ethanol
Co-administration of metronidazole and ethanol (alcohol) results, rarely, in a disulfiram-like reaction (nausea, vomiting, flushing, tachycardia). Consumption of alcohol should be avoided by patients during systemic metronidazole therapy and for at least 24 hours after completion of treatment. (Rossi, 2006) However, the occurrence of this reaction in the clinical setting has recently been questioned by some authors. (Williams & Woodcock, 2000; Visapaa et al., 2002)
Read more at Wikipedia.org