Monday
Competitive sports can bring out the best in people, but once in a while, athletics also bring to light something unexpected. "This is going to sound weird, but my heart's not right," Hailey disclosed in a previous visit. She began having episodes of rapid heart-pounding lasting two to three minutes while she was participating in sporting events as a senior in high school. In college, the 20-year-old no longer played softball or volleyball, but she continued to have the same symptoms during strenuous activities. Hailey's resting heart rate was in the low 90s, and her blood pressure was 116/78 mm Hg. Her electrocardiogram was unremarkable. Results of a metabolic profile, thyroid function tests, and complete blood count were normal. An event recorder documented supraventricular tachycardia and episodes of atrial flutter with a rate around 250 beats per minute. Exercise was linked to the arrhythmia. I referred Hailey to a cardiologist, and she had electrophysiologic testing, which showed uncommon atrioventricular node reentry. Hailey chose to undergo intracardiac mapping with radiofrequency catheter ablation. Since the radiofrequency ablation was performed, she has been asymptomatic. Hailey was pleased that she doesn't require long-term treatment with medication. "Isn't technology wonderful!" she exclaimed at her visit today. "I'm really thankful that everything turned out okay." Hailey's relief and gratitude were nearly as heartwarming as the procedure.
Tuesday
"It's hard to believe that I was 200 lb of pure muscle," reflected Warren at his last visit. "Nowadays, I'm just 200-plus lb of muscle aches and pains," the 52-year-old coal miner lamented. He was particularly bothered by constant soreness of the muscles in his arms and legs. In light of the more than 30 years he had logged in the mines, Warren had already formulated a diagnosis. "I think my job has ruined me." The examination I performed at that visit revealed some arthritic changes of his knees, hands, and shoulders. No muscle tenderness, atrophy, or weakness was present, so myopathy seemed unlikely. One laboratory test showed intriguing results--an abnormal creatine kinase level of 632 U per L. His MB isoenzyme of creatine kinase (1.95 ng per mL), erythrocyte sedimentation rate (11 mm per hour), and white blood cell count (6,000 cells per mm3) were normal. I asked Warren to have some additional blood work done, but I wanted him to wait until he had been off work for a day or two. The new results arrived today. Warren's creatine kinase level remained elevated--324 U per L--but it was better. The results of the aldolase (4.9 U per L) and other tests including uric acid, antinuclear antibodies, and rheumatoid factor were normal. I knew strenuous activity could cause an elevation of creatine kinase, but was that the reason for Warren's problem? If it was, then what practical remedy could I offer him? I spent so much time reviewing the literature and thinking about the case that I gave myself tired eyes and a headache. For now, the diagnosis that makes the most sense is the one he came up with himself: work hurts.
Wednesday
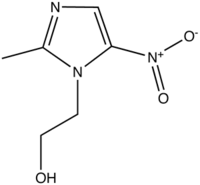
Mrs. Mendell loved her peas. The 71 year old relished the vegetables grown in her garden. Today, I had my doubts that the affection was mutual. Mrs. Mendell had been eating lots of tomatoes and nuts lately, and for the past few days, she had experienced lower abdominal cramping and mild constipation. On examination, I found Mrs. Mendell had left lower quadrant abdominal tenderness and a low-grade fever. Bowel sounds were normal, a stool for occult blood was negative, and the results of a urinalysis were normal, but her white blood cell count was slightly elevated.
"You have a case of diverticulitis," I informed her. The diagnosis didn't faze her. "Don't all older people have that?" she inquired. I explained to her the difference between diverticulosis and diverticulitis. "I don't want that 'itis'," Mrs. Mendell said while wagging her finger at me. Outpatient treatment seemed appropriate, so I started her on ciprofloxacin (Cipro) and metronidazole (Flagyl). I asked her to alter her diet and return in a couple of days to be reexamined. "What am I going to do with all those vegetables I can't eat?" she thought aloud. The solution suddenly surfaced. "I bet you and your staff love tomatoes. I'll have my husband drop off a shopping bag of them later today."
Thursday
Bernadette mistrusts any doctor except her own and has misgivings about prescription drugs. The 60-year-old woman is a human matchstick--tall and lean with closely cropped red hair and a temper that is easily ignited. Not long ago, Bernadette developed a deep, aching pain in her left shin. She had not injured her lower leg and denied any other bone pain. Grudgingly, she consented to an x-ray of the tibia and a blood test. The radiologist reported changes consistent with Paget's disease of the bone. Further supporting the diagnosis were an elevated alkaline phosphatase level and normal serum calcium. Not surprisingly, Bernadette refused to see an endocrinologist or orthopedist. Because she had no kidney disease or esophageal problems, I asked her to consider treatment with a bisphosphonate agent: alendronate (Fosamax) for six months or risedronate (Actonel) for two months. "No thanks," she said. "If it ain't broke, don't go trying to fix it." To no avail, I explained how the changes associated with Paget's disease make the affected bone weaker and more likely to fracture. There was no way I was going to change this woman's mind. "You don't have to decide today," I said. "I'll be happy to discuss the problem again any time you like." It's hard to light a fire under some people. In Bernadette's case, gentleness may prove to be more effective than coercion.
Friday
Seven months ago, Joe awoke from a sound sleep with an awful pain in his big toe. "Tell me this isn't gout," he entreated. I wasn't able to oblige him. The first metatarsophalangeal joint of his right foot was swollen, warm, reddened, and exquisitely tender to light touch. His uric acid was 9.4 mg per dL and serum creatinine was normal. Treatment with indomethacin (Indocin) quickly stamped out his first episode of gout. Joe failed to follow my recommendations of a low purine diet, weight reduction, and limitation of alcohol intake. Three months later, his gout was back, and so was Joe. Another round of indomethacin provided rapid relief. Today, Joe returned with his third episode of gout. After this last flare is resolved, he will begin treatment for recurrent gout with allopurinol (Zyloprim) 100 mg a day and colchicine 0.6 mg twice a day. The dose of allopurinol will be increased gradually until his uric acid level falls below 6.0 mg per dL. "Is it safe to have a beer now and then with these medicines?" he asked sheepishly. Disappointed and frustrated, I let out a sigh. "Gotcha!" he laughed. Joe had seen the light; I hoped that we had seen the end of his gout.
Saturday/Sunday
"Look in my ear," Leah instructed me. "It's been hurting off and on for the past few months." I examined her ears and found nothing wrong with them. The 36-year-old elementary school teacher vigorously rubbed the skin in front of her right ear, which tipped me off to a possible diagnosis. Mild tenderness was present over the temporo-mandibular joint (TMJ). "Open wide and say 'Aah'," I directed her. A popping noise emanated from her right jaw. "That doesn't sound too good," she remarked. I noticed Leah had a limited ability to open her mouth wide. In addition, she had a crossbite. "You can blame your earache on TMJ disorder," I informed her. She began filling in some blanks about problems at work, occasional teeth grinding, and a fondness for chewing gum. I asked Leah to take ibuprofen as needed for her pain, apply moist heat to the TMJ, and gently massage the area. She would contact her dentist about a mouth splint, and we talked about ways to reduce stress. Before Leah left the office, I gave her a final assignment, "No clenching your teeth or chewing gum at school."
Tony Miksanek, M.D., has been a family physician for more than 20 years. Most of that time has been in solo private practice in Benton, a town with a population of about 7,000 in rural southern Illinois.
Address correspondence to Tony Miksanek, M.D., 712 Old Orchard Dr., Benton, IL 62812.
To preserve patient confidentiality, the patients' names and identifying characteristics have been changed in each scenario. Any resemblance to actual persons is coincidental.
COPYRIGHT 2005 American Academy of Family Physicians
COPYRIGHT 2005 Gale Group