Invasive aspergillosis (IA) used to be regarded as a curiosity-a case of interest to be presented at Grand Rounds. The rising frequency of IA with its associated high mortality has placed it center stage among pulmonary complications in immunocompromised patients. A review of insurance-based diagnoses in the United Slates in 1996 identified 10,000 cases at an overall treatment cost of $633 million (1). The actual number of cases is likely to be far greater, because the diagnosis of IA is difficult and culture has a sensitivity of approximately 30% (2).
In the current issue of the Journal, Meersseman and colleagues (pp. 621-625) describe 89 cases of IA in patients in a medical intensive care unit without leukemia or cancer (3), a rate of about 4.0%. In another report from Belgium, disseminated aspergillosis was documented in six patients who underwent autopsy, five of whom had COPD, a rate of 2.7% (4). Invasive pulmonary aspergillosis, which is much more common than disseminated disease, was not accounted for in that study. Thus, IA appears to be gaining a foothold in the ICU in patients without classical risk factors.
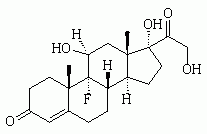
Two at-risk patient groups stand out for IA-COPD (usually treated with corticosteroids) and severe hepatic failure. Corticosteroicls are problematic in this context. It is well recognized that neutropenia and corticosteroid use are the most important antecedents for IA (5). Corticosteroids induce complex immune dysregulation impairing neutrophil and macrophage function as well as directly increasing the growth rate of Aspergillus fumigatus and Aspergillus flavus in vitro (6). The recent data suggesting benefit from a short course of corticosteroids in exacerbations of COPD will undoubtedly magnify this problem (7), as may the increasing use of hydrocortisone for septic shock with adrenal hyporesponse (8).
Diagnosing IA with confidence is usually difficult. Confirmation of the diagnosis requires demonstration of hyphae in tissue and/or the culture of Aspergillus species from sterile specimens (9). In patients requiring artificial or noninvasive ventilation, biopsy or percutaneous needle aspiration is usually not possible (although diagnostically desirable) because of critical oxygen requirements. Several authors, in trying to achieve a provisional diagnosis, have required multiple cultures from respiratory specimens as an alternative (1, 10). Interestingly, when the number of positive samples was examined in a hospital-based survey of aspergillosis, 61 % of those with confirmed IA had a single positive culture result and only 18% had three positive culture results (2). This suggests that requiring multiple positive results as a criterion for a diagnosis underestimates the size of the problem.
Application of molecular methods, including polymerase chain reactions (PCR), to respiratory secretions in patients in the ICU and in other critically ill patients may improve the sensitivity, allowing earlier diagnosis to be made (11). In the study by Meersseman and coworkers, galactomannan assays on blood were used to contribute to the diagnosis in a large proportion of patients. This is an important finding, and one that requires confirmation given that false positive results may be obtained with antibiotics, notably certain batches of piperacillin-tazobactam and amoxicillin-clavulanate. Nonetheless, two strongly positive results from blood are highly suggestive of invasive disease. It may be that antigen detection in BAL specimens would also be useful, but has not been systematically studied as yet. Antibody detection or seroconversion in patients with chronic obstructive airways disease with new cavitary infiltrates is highly suggestive of chronic pulmonary aspergillosis, but may also reflect subacute IA (chronic necrotising pulmonary aspergillosis) (12), both of which require systemic antifungal therapy.
There are numerous sources of Aspergillus for patients in intensive care. Patients may bring the isolate into the hospital themselves, being colonized in the upper or lower respiratory tract, or they may acquire the infection in general wards or in the ICU. Aerosolized organisms are a potential source of infection, through outdoor air with open windows, improperly cleaned ventilation systems, or locally from computer consoles and other dust traps. Contaminated water has also been identified as a source of infection, although this may differ very substantially from place to place and may depend upon the source of the water (13). Several water-containing machines located in patient areas have been suggested to be sources of infection, and include ice-making machines, nebulizers, and ultrasonic humidifiers. A systematic study of ventilators as a source of infection has not been undertaken. Infection may arise not simply in the respiratory tract but also from contamination of surgical wounds (14, 15). In 2004, the CDC Guidelines for the Prevention of Health Care Associated Pneumonia were published (16). The focus of these guidelines is on highly immunocompromised patients, such as those undergoing stem cell transplantation. No specific guidance is provided with respect to the prevention of IA in critical care unit patients other than a high index of suspicion, especially in patients on corticosteroids or after transplantation.
Successful management of IA is difficult. IA carries a high mortality (> 50%) (17). The options for therapy have substantially improved in the last two years with the introduction of caspofungin and voriconazole. Voriconazole is clearly the drug of choice if there are no contraindications to its use (18). Unfortunately, approximately 50% of patients in intensive care with IA are in acute renal failure, which is a contraindication to voriconazole therapy and also complicates treatment with amphotericin B. In patients on renal support, caspofungin may be appropriate even though it is not approved and there are no published data on its utility as first line therapy for IA (19).
References
1. Dasbach EJ, Davies GM, Teutsch SM. Burden of aspergillosis-related hospitalizations in the United States. Clin Infect Dis 2000;31:1524-1528.
2. Perfect JR, Cox GM, Lee JY, Kauffman CA, de Repentigny L, Chapman SW, Morrison VA, Pappas P, Hiemenz JW, Stevens DA. Mycoses Study Group. The impact of culture isolation of Aspergillus species: a hospital-based survey of aspergillosis. Clin Infect Dis 2001;33:1824-1833.
3. Meersseman W, Vandecasteele SJ, Wilmer A, Verbeken E, Peetermans WE, Van Wijngaerden E. Invasive aspergillosis in critically ill patients without malignancy. Am J Respir Crit Care Med 2004;170:621-625.
4. Dimopoulos G, Piagnerelli M, Berre J, Eddafali B, Salmon I, Vincent JL. Disseminated aspergillosis in intensive care unit patients: an autopsy study. J Chemother 2003;15:71-75.
5. Lionakis MS, Kontoyiannis DP. Glucocorticoids and invasive fungal infections. Lancet 2003;362:1828-1838.
6. Ng TTC, Robson GD, Denning DW. Hydrocortisone-enhanced growth of Aspergillus spp.: implications for pathogenesis. Microbiol 1994;140:2475-2480.
7. Aaron SD, Vandemheen KL, Hebert P, Dales R, Stiell IG, Ahuja J, Dickinson G, Brison R, Rowe BH, Dreyer J, et al. Outpatient oral prednisone after emergency treatment of chronic obstructive pulmonary disease. N Engl J Med 2003;348:2618-2625.
8. Annane D, Sebille V, Charpentier C, Bollaert PE, Francois B, Korach JM, Capellier G, Cohen Y, Azoulay E, Troche G, et al. Effect of treatment with low doses of hydrocortisone and fludrocortisone on mortality in patients with septic shock. JAMA 2002;288:862-871.
9. Ascioglu S, Rex JH, de Pauw B, Bennett JE, Bille J, Crokaert F, Denning DW, Donnelly JP, Edwards JE, Erjavec Z, et al. Defining opportunistic invasive fungal infections in immunocompromised patients with cancer: an international consensus. Clin Infect Dis 2002;34:7-14.
10. Bulpa PA, Dive AM, Garrino MG, Delos MA, Gonzalez MR, Evrard PA, Glupczynski Y, Installe EJ. Chronic obstructive pulmonary disease patients with invasive pulmonary aspergillosis: benefits of intensive care? Intensive Care Med 2001;27:59-67.
11. Buchheidt D, Baust C, Skladny H, Baldus M, Brauninger S, Hehlmann R. Clinical evaluation of a polymerase chain reaction assay to detect Aspergillus species in bronchoalveolar lavage samples of neutropenic patients. Br J Haematol 2002;116:803-811.
12. Denning DW, Riniotis K, Dobrashian R, Sambatakou H. Chronic cavitary and fibrosing pulmonary and pleural aspergillosis: case series, proposed nomenclature and review. Clin Infect Dis 2003;37:S265-S280.
13. Warris A, Voss A, Verweij PE. Hospital sources of Aspergillus: new routes of transmission? Rev Iberoam Micol 2001;18:156-162.
14. Birch M, Nolard N, Shankland G, Denning DW. DNA typing of epidemiologically-related isolates of Aspergillus fumigatus. Infect Epidemiol 1995;114:161-168.
15. Lutz BD, Jin J, Rinaldi MG, Wickes BL, Huycke MM. Outbreak of invasive Aspergillus infection in surgical patients, associated with a contaminated air-handling system. Clin Infect Dis 2003;37:786-793.
16. Tablan OC, Anderson LJ, Besser R, Bridges C, Hajjeh R. CDC; Healthcare Infection Control Practices Advisory Committee. Guidelines for preventing health-care-associated pneumonia, 2003: recommendations of CDC and the Healthcare Infection Control Practices Advisory Committee. MMWR Recomm Rep 2004;53:1-36.
17. Denning DW. Therapeutic outcome of invasive aspergillosis. Clin Infect Dis 1996;23:608-615.
18. Herbrecht R, Denning DW, Patterson TF, Bennett JE, Greene RE, Oestmann JW, Kern W, Marr KA, Ribaud P, Lortholary O, et al. Randomised comparison of voriconazole and amphotericin B in primary therapy of invasive aspergillosis. N Engl J Med 2002;347:408-415.
19. Denning DW. Echinocandin antifungal drugs. Lanect 2003;362:1142-1151.
DOI: 10.1164/rccm.2407004
Conflict of Interest Statement: D.W.D. has received grant support from Fujisawa, Merck, Pfizer, Oxford Glycosciences, F2G, Valeant, Basilea, and OrthoBiotech, as well as the NIAID, Wellcome Trust, European Union and Fungal Research Trust. He has been a consultant to Merck, Fujisawa, Vicuron, AstraZeneca, Oxford Glycosciences, and Basilea. He has given paid talks on behalf of Gilead, Merck, Fujisawa, Pfizer, and Janssen (Japan). He is a founder shareholder of F2G, Ltd, a company focusing on fungal genomics of Aspergillus and antifungal development.
DAVID W. DENNING
Wythenshawe Hospital
Manchester, United Kingdom
Copyright American Thoracic Society Sep 15, 2004
Provided by ProQuest Information and Learning Company. All rights Reserved