Abstract
Actinic keratoses (AKs) are traditionally treated with cryotherapy, curettage, and 5-fluorouracil (5-FU, Efudex[R], ICN Pharmaceuticals, Inc.), all of which are associated with adverse effects. Although photodynamic therapy (PDT) with topical 5-aminolevulinic acid (ALA) offers a treatment alternative, current protocols require 14 to 18 hours incubation with ALA and patients experience pain during light treatment. Fifteen patients with multiple and diffuse facial AKs applied 5-FU nightly for 5 days and underwent PDT with ALA (Levulan[R] Kerastick[R], Dusa Pharmaceuticals, Inc.) on the sixth day. ALA was applied to their entire faces and remained in contact with the skin for 30 to 45 minutes under low-intensity visible light. After removing ALA, faces received a single pass of 560- to 1200-nm intense pulsed light (VascuLight or Lumenis One, Lumenis). At 1 month and at 1 year post-treatment, 90% of treated AKs had resolved in all but one patient. Erythema resolved 7 to 10 days after treatment. Patients with multiple diffuse AKs may benefit from the application of 5-FU for 5 days followed by ALA-PDT with intense pulsed light activation.
**********
Introduction
Induced by sun exposure, actinic keratoses (AKs) are proliferating neoplastic keratinocytes found only in the epidermis. When AK lesions involve the deeper papillary and reticular dermis, they are known as squamous cell carcinoma (SCC) lesions. (1) The potential progression of AK to SCC is the basis for removing AK lesions.
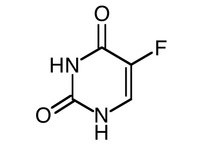
The most popular treatments of AK lesions have been cryotherapy, curettage, and 5-fluorouracil (5-FU). (2,3) Cryotherapy is associated with painful blisters and hypopigmentation while 5-FU treatment causes erythema, scaling, and crusting.
Photodynamic therapy (PDT) has emerged as a treatment modality in dermatology, (4,5) oncology, (6,7) and ophthalmology. (6) PDT requires activation of photosensitizer by light to produce singlet oxygen that selectively kills target cells. In 1990, Kennedy and colleagues (8) introduced 5-aminolevulinic acid (ALA) as a tissue-specific photosensitizing agent for the ALA-PDT treatment of AKs, squamous cell carcinoma, and superficial basal cell carcinoma. When topically applied, ALA enters abnormal tissue where it is converted to protoporphyrin IX (PpIX), a photosensitive compound easily activated by visible light. In 1999, the US Food and Drug Administration (FDA) cleared Levulan[R] Kerastick[R] ([delta]-aminolevulinic acid HCl, Dusa Pharmaceuticals, Inc., Wilmington, MA) for the treatment of multiple AKs on the scalp and head. A year later, the BLU-U[R] Blue Light Photodynamic Therapy Illuminator (Dusa Pharmaceuticals, Inc.) was cleared for the treatment of AK.
Though effective, traditional ALA-PDT calls for a 14- to 18-hour incubation with ALA prior to light treatment and patients experience discomfort during treatment with blue light. (9) These drawbacks have stimulated clinicians to experiment with shorter ALA incubation times and alternative light sources. (10-18)
Despite its temporary cosmetic disadvantages, topical treatment of AK with 5-FU is easy, inexpensive, and effective, especially for multiple, diffuse, and microscopic AK lesions. (19) The purpose of this report is to demonstrate the apparent synergistic effect of 5-FU and photodynamic therapy with ALA photosensitizing agent and intense pulsed light (IPL) for the treatment of mild to diffuse AK.
Materials and Methods
Fifteen patients (7 men and 8 women, Fitzpatrick skin types I-III) aged 30 to 80 years (median 55) with multiple and diffuse AKs gave informed consent to treatment. AKs were diagnosed by a dermatologist on the basis of medical history and clinical presentation. Patients had no prior treatments with liquid nitrogen 3 months before the study began and no treatments with 5-FU or similar topical medications during the previous year. Patients allergic to 5-FU were excluded, but no patients were excluded due to previous treatment of AKs. Results were evaluated by the treating physician and patients.
Although 5-FU is usually applied twice daily to AK lesions for 3 weeks, (12) we chose a 5-day regimen prior to ALA-PDT because our experience showed that patients who are not allergic to 5-FU could receive 5-FU for 5 days before adverse effects appeared. Patients were instructed to apply the 5-FU (Efudex[R], ICN Pharmaceuticals, Inc., Costa Mesa, CA) cream nightly for 5 nights. On the sixth day, patients presented at the clinic for ALA (Levulan[R] Kerastick[R])-PDT. Faces and chests were scrubbed briskly with acetone and gauze pads. ALA was applied to the entire face and patients were immediately placed in a room under low-intensity light. Areas treated with ALA were not covered. After 30 to 45 minutes, ALA was removed by gentle washing with soap. Areas were immediately patted dry.
Within 5 minutes, faces (except for protected eyelids) received a single pass of 560-1200-nm IPL (VascuLight or Lumenis One, Lumenis, Israel). Double pulses (30 joules/[cm.sup.2]) were given at 2.4 msec and 4.0 msec with a 20-msec delay between pulses. A chilled gel protected the epidermis and aided in delivering light evenly onto the skin surface. A 560-nm cutoff filter was kept parallel to the skin to ensure even treatment. Faces received an average of 95 pulses during the single treatment session. Patients experienced minimal to mild discomfort during IPL treatment. After treatment, patients were sent home with strict instructions to avoid direct or indirect sunlight for 48 hours.
Results
Patients were followed-up at 3 to 4 days, 7 days, 1 month, and 1 year. Diffuse erythema and scaling developed in all patients at 3 to 4 days. Erythema had resolved by 7 to 10 days. At 1 month and at 1 year post-treatment, 90% of treated AKs had resolved in all but one patient who had 50% resolution. Recurrent AKs were treated with ALA-PDT with blue light activation (BLU-U[R] Blue Light Photodynamic Therapy Illuminator). Skin texture was clinically improved in the treated facial areas of all patients. Scars were not observed and adverse effects were limited to redness, scaling, crusting, and itching. No patient withdrew from the study due to adverse effects. Patients were very pleased with skin color, skin texture, and overall outcomes.
Discussion
To our knowledge this is the first study to evaluate the sequential combination of 5-FU and ALA-PDT with IPL for the treatment of AK. When patients undergo ALA-PDT with IPL activation after applying 5-FU for 5 days, they avoid the adverse effects of 5-FU and obtain 90% resolution of AKs in less than 1 week compared to 3 or more weeks with 5-FU alone.
The effectiveness of 5-FU alone in AK removal is attributed to its inhibition of thymidylate synthetase activity--and therefore DNA synthesis--in hyperproliferative keratinocytes without damaging normal skin. (20,21) The mechanism of 5-FU's selectivity is not understood. (22) It has been suggested that 5-FU enters actively dividing cells by simple diffusion or carrier-mediated transport. (23,24)
Photodamaged skin has been rejuvenated with IPL alone. (25,26) When AKs are also present on the face and scalp, ALA-PDT, with IPL has allowed simultaneous photorejuvenation and AK removal with a single procedure. (27) More recently, Avram et al (16) obtained resolution of 68% of AKs with a single treatment of ALA-PDT with IPL activation.
Our 90% resolution of AKs suggests that pretreatment with 5-FU may (1) enhance the absorption of ALA by keratinocytes or (2) activate keratotic cells to a level that increases their absorption of ALA. The sequential combination of pretreatment with 5-FU and ALA-PDT with IPL activation maximizes selectivity for AK because ALA penetrates abnormal keratin more rapidly than normal keratin (8) and 5-FU destroys hyperproliferative keratinocytes without damaging normal skin.
Further studies are warranted to determine if the enhancing effect of 5-FU is due to epidermal turnover or to increased blood flow to the AK tissue, making more oxygen available for conversion to cytotoxic singlet oxygen. (The increased concentration of oxygen would then enhance the PDT destruction AK tissue cells.)
Our results justify a split-face study comparing the combination of 5-FU and ALA-PDT with ALA-PDT alone and mechanistic studies to determine the effect of 5-FU on the stratum corneum and blood flow to AK tissue.
Conclusion
Patients with multiple diffuse AKs may benefit from the application of 5-FU for 5 days followed by ALA-PDT with IPL activation.
Disclosure: Dr. Gilbert owns stock in DUSA Pharmaceuticals, Inc.
References
1. Cockerell CJ. Histopathology of incipient intraepidermal squamous cell carcinoma ("actinic keratosis"). J Am Acad Dermatol. 2000;42:11-17.
2. Dinehart SM. The treatment of actinic keratoses. J Am Acad Dermatol. 2000;42(1 Pt 2):S25-S28.
3. Fowler JF Jr., Zax RH. Aminolevulinic acid hydrochloride with photodynamic therapy: efficacy outcomes and recurrence 4 years after treatment. Cutis. 2002;69(6 Suppl):2-7.
4. Taub AF. Photodynamic therapy in dermatology: history and horizons. J Drugs Dermatol. 2004;3:S8-S25.
5. Gold MH, Goldman MP. 5-aminolevulinic acid photodynamic therapy: where we have been and where we are going. Dermatol Surg. 2004;30:1077-1083; discussion 1083-1084.
6. Marcus SL, McIntire WR. Photodynamic therapy systems and applications. Expert Opin Emerging Drugs. 2002;7:319-331.
7. Dolmans DE, Fukumura D, Jain RK. Photodynamic therapy for cancer. Nat Rev Cancer. 2003;3:380-387.
8. Kennedy JC, Pottier RH, Pross DC. Photodynamic therapy with endogenous protoporphyrin IX: basic principles and present clinical experience. J Photochem Photobiol B. 1990;6:143-148.
9. Jeffes EW, et al. Photodynamic therapy of actinic keratoses with topical aminolevulinic acid hydrochloride and fluorescent blue light. J Am Acad Dermatol. 2001;45:96-104.
10. Morton CA, et al. Development of an alternative light source to lasers for photodynamic therapy. 1. Clinical evaluation in the treatment of pre-malignant non-melanoma skin cancer. Lasers Med Sci. 1995;10:165-171.
11. Calzavara-Pinton PG. Repetitive photodynamic therapy with topical delta-aminolaevulinic acid as an appropriate approach to the routine treatment of superficial non-melanoma skin tumours. J Photochem Photobiol B. 1995;29:53-57.
12. Kurwa HA, et al. A randomized paired comparison of photodynamic therapy and topical 5-fluorouracil in the treatment of actinic keratoses. J Am Acad Dermatol. 1999;41(3 Pt 1):414-418.
13. Touma D, et al. A trial of short incubation, broad-area photodynamic therapy for facial actinic keratoses and diffuse photodamage. Arch Dermatol. 2004;140:33-40.
14. Gold MH. Intense pulsed light therapy for photorejuvenation enhanced with 20% aminolevulinic acid photodynamic therapy. J Laser Med Surg. 2003;15(Suppl):47.
15. Goldman MP, Atkin D, Kincad S. PDT/ALA in the treatment of actinic damage: real world experience. J Laser Med Surg. 2002;14(S):24.
16. Avram DK, Goldman MP. Effectiveness and safety of ALA-IPL in treating actinic keratoses and photodamage. J Drugs Dermatol. 2004;3(1 Suppl):S36-39.
17. Alexiades-Armenakas M, Geronemus R. Laser mediated photodynamic therapy of actinic keratoses. Arch Dermatol. 2003;139:1313-1320.
18. Alexiades-Armenakas MR, Geronemus RG. Laser-mediated photodynamic therapy of actinic cheilitis. J Drugs Dermatol. 2004;3:548-551.
19. Goette DK. Topical chemotherapy with 5-fluorouracil. A review. J Am Acad Dermatol. 1981;4:633-649.
20. Dillaha CJ, et al. Selective cytotoxic effect of topical 5-fluorouracil. Arch Dermatol. 1963;88:247-256.
21. Lawrence N, et al. A comparison of the efficacy and safety of Jessner's solution and 35% trichloroacetic acid vs 5% fluorouracil in the treatment of widespread facial actinic keratoses. Arch Dermatol. 1995;131:176-181.
22. Robins P, Gupta AK. The use of topical fluorouracil to treat actinic keratosis. Cutis. 2002;70(2 Suppl):4-7.
23. Kessel D, Hall TC. Studies on drug transport by normal human leukocytes. Biochem Pharmacol. 1967;16:2395-2403.
24. Diasio RB, Harris BE. Clinical pharmacology of 5-fluorouracil. Clin Pharmacokinet. 1989;16:215-237.
25. Bitter PH. Noninvasive rejuvenation of photodamaged skin using serial, full-face intense pulsed light treatments. Dermatol Surg. 2000;26:835-842.
26. Negishi K, et al. Photorejuvenation for Asian skin by intense pulsed light. Dermatol Surg. 2001;27:627-631.
27. Ruiz-Rodriguez R, et al. Photodynamic photorejuvenation. Dermatol Surg. 2002;28:742-744.
Dore J. Gilbert MD
Newport Dermatology & Laser Associates, Newport Beach, CA
Address for Correspondence
Dore J. Gilbert MD
Newport Dermatology & Laser Associates
1441 Avacado, Suite #806
Newport Beach, CA 92660
Phone: 949-718-1222
Fax: 949-718-1220
e-mail: lazrdoc@pacbell.net
COPYRIGHT 2005 Journal of Drugs in Dermatology, Inc.
COPYRIGHT 2005 Gale Group