Background: Inhaled corticosteroids (ICSs) are an effective treatment of asthma even when administered at a low dose. Once asthma is controlled, current guidelines recommend that the dose of ICS be reduced to the lowest possible and effective dose. Although the most appropriate strategy for the stepping down has not yet been defined, quantification of sputum eosinophils and bronchial hyperresponsiveness (BHR) are indeed measures of asthma control.
Objective: To compare the efficacy of step-down and fixed-dose strategies in the control of BHR to methacholine and eosinophilic inflammation patients with mild-to-moderate asthma.
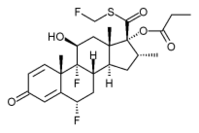
Methods: We performed a double-blind, randomized study to compare inhaled fluticasone propionate (FP), 1,000 [micro]g/d, then reduced to 200 [micro]g/d (group 1; n = 18) to a fixed dose of FP, 200 [micro]g/d (group 2; n = 17) administered for 6 weeks and then 8 weeks in reducing the provocative dose of methacholine causing a 20% fall in FE[V.sub.1] (P[D.sub.20]) and sputum eosinophils in 35 patients. The duration of the efficacy was also followed subsequently after 8 weeks of placebo treatment.
Results: P[D.sub.20] remarkably increased with both treatment strategies, but differences between groups were not significant. Sputum eosinophils (median values, percentage) at baseline and after each treatment period were not different (group 1, 16.4 to 1.0 to 2.7%; group 2, 16.7 to 2.8 to 2.8%, respectively). The percentages of patients in whom sputum eosinophilia was normalized ([less than or equal to] 3%) were as follows: group 1, 69% and 60%; group 2, 50% and 57%. After placebo treatment, sputum eosinophils were still "normalized" in approximately one third of patients.
Conclusion: Step-down and fixed-dose strategies with FP improved P[D.sub.20] and sputum eosinophilia to a similar degree. The effect on sputum eosinophils persisted longer than that on methacholine.
Key words: asthma; fluticasone propionate; inhaled steroids; sputum eosinophils
Abbreviations: BHR = bronchial hyperresponsiveness; CI = confidence interval; FP = fluticasone propionate; ICS = inhaled corticosteroid; IS = induced sputum; P[D.sub.20] = provocative dose of methacholine causing a 20% fall in FE[V.sub.1]; PEFR = peak expiratory flow rate
**********
According to current asthma management guidelines, (1) the adjustment of the inhaled corticosteroid (ICS) treatment should be guided by symptoms and lung function. However, the relationship between symptoms/lung function and markers of inflammation is complex, (2) the perception of symptoms may be impaired in some patients, (3) and lung function may be near to normal, whereas eosinophilic inflammation and bronchial hyperresponsiveness (BHR) are high. (4) During treatment with ICSs, sputum eosinophils and airway responsiveness provide a direct assessment of the degree of asthma control. (5) The eosinophil count in induced sputum (IS) has proved to be suitable method to assess the efficacy of ICS therapy and, combined with measurement of BHR, to titrate corticosteroid dose. (8)
In the management of mild-to-moderate asthma, uncertainty remains over starting with a high or low ICS dose.9 Changes in symptoms and peak expiratory flow rate (PEFR) induced by a low dose (200 [micro]g/d) and a high dose (800 [micro]g/d) of inhaled budesonide in steroid-naive patients with asthma appear to be similar, (10,11) whereas changes in BHR reach a borderline significance. (11) While changes in symptoms and lung function after ICS treatment are unlikely to be dose dependent in patients with mild-to-moderate asthma, a dose-dependent effect on methacholine hyperresponsiveness after fluticasone propionate (FP) has been demonstrated by some (7,13) but not all authors. (14) In addition, changes in sputum eosinophils may be used to demonstrate a dose-dependent effect of ICSs. (7)
Asthma management guidelines suggest either a step-up (1) or a step-down (15) strategy to gain initial control of asthma. However, it is not clearly known whether starting with a high dose and stepping down is a valid treatment strategy in the asthma management. (9,6) van der Molen et al (l0) suggest that a stepdown strategy with budesonide is not superior than a continuous maintenance treatment with a low dose in the control of symptoms and lung function. However, until now no comparison has been published to assess the efficacy of the step-down and fixed-dose strategies with inhaled FP in the control of eosinophilic inflammation and BHR in patients with asthma. In addition, the duration of the effect of the two treatment strategies has not been examined.
Thus, we compared the efficacy of inhaled FP administered in a dose of 1,000 [micro]g/d and then reduced to a dose of 200 [micro]g/d to a fixed dose of FP, 200 [micro]g/d, in reducing eosinophilic inflammation and BHR to methacholine in patients with mild-to-moderate asthma. In addition, we assessed the duration of the effect of the two treatment strategies.
MATERIALS AND METHODS
Population
Male and female nonsmoking patients with asthma, (17) 18 to 60 years of age, were eligible for the study. Criteria for inclusion were as follows: (1) baseline FE[V.sub.1] [greater than or equal to] 60% of predicted value, (2) sputum eosinophils [greater than or equal to] 5%, and (3) provocative dose of methacholine causing a 20% fall in FE[V.sub.1] (P[D.sub.20]) < 800 [micro]g. Screening exclusion criteria were as follows: recent use of ICSs, recent respiratory infections, hospital admission for asthma within the previous 6 months, seasonal asthma, hypersensitivity to corticosteroids, pregnancy, and lactation. Presence of atopy was not a prerequisite for selection. Skin sensitivity to seasonal pollens was studied outside exposure. The study was approved by local ethics committees, and all patients signed a consent form prior to enrolment.
Study Design
We conducted a randomized, double-blind, parallel-group study that included the following: a 3-week run-in; a 6-week period during which patients received FP, 500 [micro]g bid (group 1), or FP, 100 [micro]g bid (group 2); an 8-week period during which all patients received FP, 100 [micro]g bid; and an 8-week period during which all patients received single-blind placebo. Treatments were delivered by metered-dose inhalers and a spacer. The study design is summarized in Figure 1. The patients made eight clinic visits: at screening, at the end of run-in (baseline) and the end of each treatment period (visits 2, 4, and 6), and at the middle of each treatment period (visits 1, 3, and 5). At the screening visit, demographic, clinical, and physical details were recorded and lung function was assessed. During run-in, the asthma severity score was assessed. Asthma scores ranged from 0 to 12 and were based on symptoms (0 to 4), bronchodilator use (0 to 4), and daffy
[FIGURE 1 OMITTED]
Antonio Foresi, MD; Berardino, Mastropasqua, MD; Alfredo Chetta, MD, FCCP; Raffaele D'Ippolito, MD; Renato, Testi, MD; Dario Olivieri, MD, FCCP; and Andrea Pelucchi, MD PEFR variability (0 to 4). (3) Patients with 0 to 5 scores were classified as having mild disease, patients with 6 to 8 scores as having moderate disease, and patients with 9 to 12 scores as having severe disease. At the end of the run-in and of each treatment period, lung function testing (FVC and FE[V.sub.1]), methacholine challenge, and IS were performed (these were performed 2 to 3 days apart). At each intermediate visit, only lung function was performed. Throughout the study, morning and evening PEFRs were recorded (mini-Wright; Clement-Clarke International; Essex, UK).
During the three treatment periods, patients were allowed to use only albuterol/salbutamol on an as-needed basis. Long-acting bronchodilators, oral corticosteroids, xanthines, cromones, and antihistamines were not permitted. In case of an exacerbation (worsening of symptoms that requires an intervention by a physician and a PEFR value < 60% of baseline), patients were treated with prednisone, 25 mg/d, for 3 days. If they improved, oral steroids were stopped. If not, prednisone was administered for 3 additional days. Those patients who did not improve and patients experiencing more than two exacerbations were withdrawn from the study.
Measurements
Short-acting bronchodilators were withheld for 12 h before measuring lung function. FVC and FE[V.sub.1] were measured by a flow-sensing spirometer connected to a computer for data analysis (Vmax 22; SensorMedics; Yorba Linda, CA). The best value of three reproducible maneuvers was expressed as a percentage of predicted. Triplicate measurements of PEFR were recorded in the morning and evening, and the best values were considered. Mean PEFR recorded during the last 2 weeks of the run-in period were taken as baseline values, and mean values recorded during the last 2 weeks of each treatment period were considered for the analysis.
Bronchial challenge with methacholine was performed between 8 AM and 10 AM, according to a standard procedure. (18) After three reproducible FE[V.sub.1] measurements were obtained, doubling concentrations of methacholine from 0.03 mg/mL were inhaled at 5-min intervals. Solutions were delivered by a nebulizer (model 646; DeVilbiss; Somerset, PA) attached to a dosimeter (Mefar MB3; Mefar; Brescia, Italy). Inhalations were continued until FE[V.sub.1] decreased by [greater than or equal to] 20% from post-saline solution measurements or when a cumulative dose of methacholine of 4,600 [mu]g was administered. Bronchial responsiveness was expressed as P[D.sub.20] and given in micrograms.
Sputum induction was performed between 8:00 and 10:00 AM according to a standardized method. (19) Prior to sputum induction, all patients inhaled salbutamol, 200 [mu]g, and 10 min later they underwent spirometry. Patients were then asked to inhale nebulized, sterile, 3% saline solution from an ultrasonic nebulizer (output, 2 mL/min) [Mistogen EN143; Mistogen Equipment; Oakland, CA]. Patients expectorated into a glass container, sputum samples were homogenized with dithiothreitol, and 10 [mu]L was used to determine the total cell count. The suspension was cytocentrifuged at 700 revolutions per minute for 5 min, and slides were stored at -80[degrees]C. The differential cell count based on 300 cells was obtained by staining (Diff-Quik stain; Baxter Scientific Products; Miami, FL) and expressed as the percentage of total nucleated cells excluding squamous cells. Cell viability (trypan blue exclusion) was always > 80%. Slides were coded, and counts were performed on at least two slides by two expert observers who were blind to the clinical characteristics of patients. Between-observer coefficient of variation for eosinophil count was 4.2%.
Statistical Analysis
Normality of distributions was assessed using the Kolmogorov-Smirnov test. Values were reported as mean ([+ or -] SD or range) or median (25th to 75th percentiles), or geometric means (95% confidence intervals). The unpaired t test and [chi square] test were used for comparison between the two groups at baseline. Since a reduction in sputum eosinophils was selected as the primary indicator for the comparative effect of different FP doses, we selected patients showing a > 5% eosinophil count at baseline. Changes in sputum cells at each visit were examined by the Wilcoxon test. Comparison between treatments was also estimated by analyzing the percentage of patients in whom sputum eosinophils was normalized ([less than or equal to] 3%) (29) by means of the Fisher exact test. Changes in FVC, FE[V.sub.1], PEFR, and P[D.sub.20] were analyzed with the analysis of covariance (baseline values as covariate). Statistical differences within treatment comparisons were not calculated since changes during the study might be due to the effect of regression toward the means. All the analyses were conducted on the intention-to-treat population (missing data were estimated by the last-observation-carried-forward method) and on all available data. Statistical significance tests were two tailed and performed at the 5% level.
RESULTS
The baseline characteristics of intention-to-treat population are shown in Table 1. The two treatment groups were not different with regard to age, sex distribution, atopy, duration of the disease, and baseline lung function. According to the asthma severity score assessed during the 3-week run-in period, 40% of patients had mild asthma and 60% of patients had moderate asthma. The distribution of asthma severity score in the two groups was not different. During the study, seven patients were withdrawn: four patients from group 1 (three due to poor asthma control, and one due to an adverse event) and three patients from group 2 (all due to poor asthma control). No asthmatic exacerbation requiring oral corticosteroid was recorded.
Lung Function
Although there was a tendency for both FVC and FE[V.sub.1] to increase more in group 1 during the first period, no statistically significant difference between treatments was found at any scheduled visit. After the first, second, and third periods, the mean difference in FVC between groups was as follows: 240 mL (95% confidence interval [CI], - 2 to 520 mL), 120 mL (95% CI, 14 to 370 mL), and -7 mL (95% CI, -340 to 200 mL), respectively. The corresponding mean difference in FE[V.sub.1] was as follows: 130 mL (95% CI, - 13 to 390 mL), 1 mL (95% CI, - 330 to 3,200 mL), and - 5 mL (95% CI, - 350 to 250 mL), respectively.
Mean morning PEFRs recorded during the last 2 weeks prior to randomization and during the treatment period are shown in Figure 2. Results of the morning and evening PEFRs did not differ between the treatment groups at any study period.
Methacholine Challenge
At baseline, geometric mean P[D.sub.20] value in group 1 was lower, although not significantly, than in group 2 (91 [mu]g vs 209 [mu]g) [Table 2, Fig 3]. At the end of the first treatment period, P[D.sub.20] values increased more in group 1 than in group 2 (Table 2, Fig 3). However, the difference was not significant. The mean ratio change between treatments was 2.01 (95% CI, 0.75 to 5.4; p = 0.16). At the end of the second period, when all patients were treated with FP, 200 [mu]g/d, the P[D.sub.20] value in group 1 remained stable, whereas it tended to slightly increase in group 2 (Table 2, Fig 3). Again the difference was not significant. The mean ratio change between treatments was 1.14 (95% CI, 0.36 to 3.63). At the end of the placebo period, mean P[D.sub.20] values returned to pretreatment in both groups (111 vs 166 [mu]g) [Table 2, Fig 3].
[FIGURE 3 OMITTED]
Induced Sputum
At baseline, total and differential cell counts in IS were similar (Table 2). Total cells, macrophages, lymphocytes, and neutrophils in IS did not change during the study. At the end of the first treatment period (FP, 1,000 [mu]g or 200 [mu]g), sputum eosinophils remarkably decreased in both groups (Table 2, Fig 4). The difference between treatment groups was not statistically significant (Table 2, Fig 4). The percentages of patients in whom sputum eosinophilia was normalized (eosinophils [less than or equal to] 3%), were 69% in group 1, and 50% in group 2 (p = 0.46, Fisher exact test). At the end of the second treatment period (fixed-dose FP, 200 median eosinophils were lower than baseline and approximately similar in both groups, with no difference between groups (Table 2, Fig 4). The percentages of patients in whom sputum eosinophilia was normalized were 60% in group 1, and 57% in group 2. The percentages of sputum eosinophils measured at the end of the placebo period tended to be similar to that measured at baseline and without statistically significant differences between groups (Table 2, Fig 4). However, sputum eosinophils were < 3% in approximately one third of patients from both groups (36% and 38%, respectively), with no obvious difference between treatments.
DISCUSSION
This study showed that starting with a high FP dose and then stepping down to a low dose is not more effective than a low FP dose in reducing sputum eosinophilia and the degree of methacholine hyperresponsiveness in patients with mild-to-moderate asthma. In particular, sputum eosinophilia was normalized in approximately 60% of treated patients. When stepping down from the high to the low FP dose, no apparent worsening of eosinophilia occurred. In addition, this study confirmed that low-dose FP is quite effective and that the improvements reversed within few weeks. However, it was noteworthy that sputum eosinophilia was still within the normal range in approximately 30% of patients in both groups after 8 weeks off treatment.
To our knowledge, this is the first study comparing a step-down to a constant fixed low FP dose in asthma, having sputum eosinophilia as a primary outcome. Despite a fivefold difference between high-dose and low-dose FP, both treatments remarkably reduced sputum eosinophils, without any difference between the two treatment approaches. After switching to the low-dose FP, no significant deterioration in sputum eosinophils was detectable in patients with mild-to-moderate asthma. It is noteworthy that the sputum eosinophilia was "normalized" ([less than or equal to] 3%) in approximately 50% and 60%, respectively, of patients after the first and second treatment periods. Gershman et al, (7) examining the effect on sputum eosinophils of 100 and 1,000 [mu]g of FP administered for 6 weeks, also found no difference in the two groups. However, they selected patients with a rather low percentage of sputum eosinophils (< 2%). As they correctly pointed out, this could have remarkably influenced their findings (7) as well as those reported by others. (21-23) Thus, we recruited only patients showing a percentage sputum eosinophils > 5%. A high baseline percentage of sputum eosinophils should be recommended since it allows a consistent room for improvement and sputum eosinophils above a given percentage would tend to reduce between-group variability.
Our study confirms that sputum eosinophil count was reduced to 3% within a few weeks in many, but not all, patients with mild-to-moderate asthma. (7) The persistence of eosinophilic inflammation despite 8 weeks of treatment with low-dose FP in asthmatic patients with near-normal lung function suggests that individual dose titration of ICS is necessary to achieve complete control. Indeed, minimizing eosinophilic inflammation is a cardinal component of asthma management for at least two reasons: eosinophilic inflammation may lead to irreversible airway damage, (24) and it increases the risk of clinical exacerbation. (8,25-27)
We confirmed that geometric mean of P[D.sub.20] improved by approximately 2.38 doubling dose during high-dose FP and by 1.02 doubling dose during low-dose FP treatment. (7,14) Changes from baseline in the two groups were similar at the end of the fixed-dose period (2.17 and 1.86 doubling doses, respectively). It is possible that the lack of difference between doses was caused by a too-short duration of treatment (13) or due to a type II error. However, it is unlikely that a dose-response effect may become evident by further increasing the difference in dosing schedules, since FP, 2,000 [mu]g, administered to asthmatic patients for 6 weeks increased P[D.sub.20] by 1.9 doubling doses. (28)
The absence of any significant improvement in lung function following FP treatment was not unexpected and may likely be due to the rather normal mean baseline levels of FVC, FE[V.sub.1], and PEFR in our study population and to the sample size. (10) Similar findings have been reported by others. (14,21) Indeed, changes in lung function are detectable when pretreatment values are approximately < 70% of predicted. (6,7,29,30) Thus, monitoring asthma during treatment with ICSs to assess its control cannot be solely based on symptoms and lung function but should include a marker inflammation.
In keeping with previous studies, (7,28) we found that regardless of the treatment approach, when ICS are stopped, P[D.sub.20] values completely reversed to baseline. In mild-to-moderate asthma, sputum eosinophils increased to pretreatment values after few days (31) or weeks (6,7) after stopping ICSs. In contrast, a rapid flare-up of eosinophilic inflammation has been demonstrated in severe asthma when tapering the FP dose, which was associated with clinical exacerbation. (32) Although the effect of FP treatment on eosinophilic inflammation is clearly temporary, (7) it is interest that 8 weeks after FP withdrawal, eosinophils in sputum were still < 3% in approximately 30% of asthmatic patients from both treatment groups.
Although we administered a fivefold difference in the dose of inhaled FP in the first 6 weeks and selected patients on the basis of the presence of sputum eosinophils count > 5%, a dose-dependent effect on the reduction of sputum eosinophilia could not have been demonstrated. Previous studies (7,21-23,33) also failed to find a "clear" dose-response to ICSs by assessing changes in sputum eosinophils This was likely due to the low baseline eosinophil count, to its high degree of variability, and to the ability of low doses to produce a remarkable reduction. It is possible that by studying a larger population for a longer period of time, the number patients in different treatment groups reaching the cutoff point of 3% would also be different. However, since minimal clinically or biologically relevant change in sputum eosinophil has not yet been identified, sample size is difficult to calculate. (5,7) It is noteworthy that a dose-dependent effect of FP has been demonstrated by assessing the number of exacerbations in asthmatic children (34) and vascular remodeling in bronchial biopsy samples from patients with asthma. (35) We cannot exclude from consideration that the failure to detect a real intergroup difference at the end of first treatment period might be due to a type II error.
Our results together with previous findings, (7) strongly suggest that the step-down or "hit-hard" approach may not be necessary in patients with mild-to-moderate asthma to obtain control of eosinophilic inflammation. Since stepping down is critical for the individual optimal long-term management, several possible indicators could be considered, such as symptoms-free days, time to first exacerbations, exacerbation rate, BHR, and direct (sputum eosinophils) and indirect (adenosine, nitric oxide) markers of inflammation. It appears that monitoring sputum eosinophils during ICS treatment could shape the treatment approach in individual patients with asthma for the following reasons: (1) it is a direct assessment of important pathogenetic mechanisms, (2) it could identify poor responders to inhaled steroids and loss of control, and (3) it is helpful to adjust the ICS dose and to select the best drug combination.
In conclusion, we showed that treatment of mild-to-moderate asthmatic patients with normal lung function and high sputum eosinophils counts, with two different dosing schedules of FP (starting high and stepping down, and fixed dose) reduced BHR and sputum eosinophilia to a similar degree. In approximately one third of patients, the effect of both treatment strategies on sputum eosinophilia persisted longer than that on BHR.
REFERENCES
(1) British Thoracic Society. British guideline on the management of asthma. Thorax 2003; 58:1-94
(2) Postma DS, Kerstjens HA. Characteristics of airway hyperresponsiveness in asthma and in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 1998; 158:S187-S192
(3) Chetta A, Gerra G, Foresi A, et al. Personality profiles and breathlessness perception in outpatients with different gradings of asthma. Am J Respir Crit Care Med 1998; 157: 116-122
(4) Rosi E, Ronchi MC, Grazzini M, et al. Sputum analysis, bronchial hyperresponsiveness, and airway function in asthma: results of a factor analysis. J Allergy Clin Immunol 1999; 103:232-237
(5) Parameswaran K, Hargreave FE. The use of sputum cell counts to evaluate asthma medications. Br J Clin Pharmacol 2001; 52:121-128
(6) Fahy JV, Boushey HA. Effect of low-dose beclomethasone dipropionate on asthma control and airway inflammation. Eur Respir J 1998; 11:1240-1247
(7) Gershman NH, Wong HH, Liu JT, et al. Low- and high-dose fluticasone propionate in asthma; effects during and after treatment. Eur Respir J 2000; 15:11-18
(8) Leuppi JD, Salome CM, Jenkins CR, et al. Predictive markers of asthma exacerbation during stepwise dose reduction of inhaled corticosteroids. Am J Respir Crit Care Med 2001; 163:406-412
(9) van der Molen T, Kerstjens HA. Starting inhaled corticosteroids in asthma: when, how high, and how long. Eur Respir J 2000; 15:3-4
(10) van der Molen T, Meyboom-De Jong B, Mulder HH, et al. Starting with a higher dose of inhaled corticosteroids in primary care asthma treatment. Am J Respir Crit Care Med 1998; 158:121-125
(11) Tukiainen H, Taivainen A, Majander R, et al. Comparison of high and low dose of the inhaled steroid, budesonide, as an initial treatment in newly detected asthma. Respir Med 2000; 94:678-683
(12) Nathan RA, Li JTC, Finn A, et al. A dose-ranging study of fluticasone propionate administered once daily via multidose powder inhaler to patients with moderate asthma. Chest 2000; 118:296-302
(13) Hofstra WB, Neijens HJ, Duiverman EJ, et al. Dose-responses over time to inhaled fluticasone propionate treatment of exercise- and methacholine-induced bronchoconstriction in children with asthma. Pediatr Pneumol 2000; 29:415-423
(14) Visser MJ, Postma DS, Arends LR, et al. One-year treatment with different dosing schedules of fluticasone propionate in childhood asthma: effects on hyperresponsiveness, lung function, and height. Am J Respir Crit Care Med 2001; 164:2073-2077
(15) Global strategy for asthma management and prevention, updated April, 2002. Bethesda, MD: National Institutes of Health, 2002; publication No. 02-3659
(16) Bacharier L. "Step-down" therapy for asthma: why, when, and how? J Allergy Clin Immunol 2002; 109:916-919
(17) American Thoracic Society. Standards for the diagnosis and care of patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 1995; 153:S77-121
(18) Chai H, Farr RS, Froehlich LA, et al. Standardization of bronchial inhalation challenge procedures. J Allergy Clin Immunol 1975; 56:323-327
(19) Fahy JV, Liu J, Boushey HA. Cellular and biochemical analysis of induced sputum from asthmatic and from healthy subjects. Am Rev Respir Dis 1993; 147:1126-1131
(20) Belda J, Leigh R, Parameswaran K, et al. Induced sputum cell counts in healthy adults. Am J Respir Crit Care Med 2000; 161:475-478
(21) Taylor DA, Jensen MW, Kanabar V, et al. A dose-dependent effect of the novel inhaled corticosteroid ciclesonide on airway responsiveness to adenosine-5'-monophosphate in asthmatic patients. Am J Respir Crit Care Med 1999; 160: 237-243
(22) Jatakanon A, Kharitonov S, Lim S, et al. Effect of differing doses of inhaled budesonide on markers of airway inflammation in patients with mild asthma. Thorax 1999; 54:108-114
(23) Kips JC, O'Connor BJ, Inman MD, et al. A long-term study of the antiinflammatory effect of low-dose budesonide plus formoterol versus high-dose budesonide in asthma. Am J Respir Crit Care Med 2000; 161:996-1001
(24) Chetta A, Foresi A, Del Donno M, et al. Airways remodeling is a distinctive feature of asthma and is related to severity of disease. Chest 1997; 111:852-857
(25) Jatakanon A, Lim S, Barnes PJ. Changes in sputum eosinophils predict loss of asthma control. Am J Respir Crit Care Med 2000; 161:64-72
(26) Belda J, Giner J, Casan P, et al. Mild exacerbations and eosinophilic inflammation in patients with stable, well-controlled asthma after 1 year of follow-up. Chest 2001; 119:1011-1017
(27) Green RH, Brighting CE, McKenna S, et al. Asthma exacerbations and sputum eosinophil counts: a randomised controlled trial. Lancet 2002; 360:1715-1721
(28) Convery RP, Leitch DN, Bromly C, et al. Effect of inhaled fluticasone propionate on airway responsiveness in treatmentnaive individuals: a lesser benefit in females. Eur Respir J 2000; 15:19-24
(29) Chervinsky P, van As A, Bronsky E, et al. Fhiticasone propionate aerosol for the treatment of adults with mild to moderate asthma. J Allergy Clin Immunol 1994; 94:676-683
(30) Busse W, Chervinsky P, Condemi J, et al. Budesonide delivered by Turbuhaler is effective in a dose-dependent fashion when used in the treatment of adult patients with chronic asthma. J Allergy Clin Immunol 1998; 101:457-461
(31) Giannini D, Di Franco A, Cianchetti S, et al. Analysis of induced sputum before and after withdrawal of treatment with inhaled corticosteroids in asthmatic patients. Clin Exp Allergy 2000; 30:1777-1784
(32) in't Veen JC, Smits HH, Hiemstra PS, et al. Lung function and sputum characteristics of patients with severe asthma during an induced exacerbation by double-blind steroid withdrawal. Am J Respir Crit Care Med 1999; 160:93-99
(33) Szefler S, Martin R, King T, et al. Significant variability in response to inhaled corticosteroids for persistent asthma. J Allergy Clin Immunol 2002; 109:410-418
(34) Bisgaard H, Gillies J, Groenewald M, et al. The effect of inhaled fluticasone propionate in the treatment of young asthmatic children: a dose comparison study. Am J Respir Crit Care Med 1999; 160:126-131
(35) Chetta A, Zanini A, Foresi A, et al. Vascular component of airway remodeling in asthma is reduced by high dose of fluticasone. Am J Respir Crit Care Med 2003; 167:751-757
* From the Respiratory Pathophysiology Unit (Drs. Foresi Mastropasqua, and Pelucchi), Sesto San Giovanni Hospital, Sesto San Giovanni; Department of Clinical Sciences (Drs. Chetta, D'Ippolito, and Olivieri), Section of Respiratory Diseases, University of Parma, Parma; and Research & Development Unit (Dr. Testi), Glaxo-Smith-Kline, Verona, Italy.
Dr. Foresi and Professor Olivieri have received financial support for research and attending meetings and have received fees for speaking by Glaxo-Smith-Kline Italy. Dr. Testi is employed by Glaxo-Smith-Kline Italy.
The study was supported by a grant from Glaxo-Smith-Kline Italy.
Manuscript received September 4, 2003; revision accepted August 16, 2004.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (e-mail: permissions@chestnet.org).
Correspondence to: Antonio Foresi, MD, Servizio di Pneumologia e Fisiopatologia Respiratoria, Viale Matteotti 83, 20099 Sesto San Giovanni, Italy; e-mail: antonio.foresi@aovimercate.org
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group