The National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents has issued its Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents. The full text, which appeared in the August 2, 2004, issue of Pediatrics, is available online at http://pediatrics.aappublications.org/cgi/content/full/114/2/S2/555.
It is now apparent that primary hypertension is detectable in the young and is common. The long-term health risks for children and adolescents who have hypertension can be substantial; therefore, it is important that clinical measures be taken to reduce these risks and optimize health outcomes.
Definition of Hypertension
The definition of hypertension in children and adolescents is based on the normative distribution of blood pressure in healthy children. Table 1 lists the classifications of hypertension in children and adolescents.
[TABLE 1 OMITTED]
Children younger than three years should have their blood pressure measured by auscultation when seen clinically; the physician should use a cuff appropriate to the size of the child's upper arm. Elevated blood pressure must be confirmed on repeated visits before diagnosing hypertension. Children who are three years of age or younger should have blood pressure measured only under certain conditions, including prematurity or other neonatal conditions requiring intensive care; presence of congenital heart disease, elevated intracranial pressure, recurrent urinary tract infections, or systemic illnesses (such as neurofibromatosis) associated with hypertension; transplant recipients; and presence of renal disease or urologic malformations.
The physician should then look up the normal range of blood pressure on newly revised and expanded tables based on gender, age, and height (available online). The child is normotensive if blood pressure is less than the 90th percentile. If an adolescent's blood pressure is greater than 120/80 mm Hg, the patient is prehypertensive, even if within the less than 90th percentile. If the blood pressure is in the 95th percentile or more, blood pressure should be assessed at least two more times before the child is diagnosed with hypertension.
Table 2 outlines the clinical evaluation of primary hypertension.
[TABLE 2 OMITTED]
Primary Hypertension
Primary hypertension in childhood usually is characterized by mild or stage 1 hyper-tension and often is associated with a family history of hypertension or cardiovascular disease. Frequently, children and adolescents with primary hypertension are overweight. The strong association of high blood pressure with obesity and the marked increase in the prevalence of childhood obesity indicate that hypertension and prehypertension are becoming a significant health issue in the young.
Primary hypertension often clusters with other risk factors. Medical history, physical examination, and laboratory evaluation should include a comprehensive assessment for additional cardiovascular risk. These risk factors, in addition to high blood pressure and being overweight, include low high-density lipoprotein cholesterol levels, elevated triglyceride levels, and abnormal glucose tolerance. Fasting plasma insulin concentration generally is elevated, but an elevated insulin concentration may be reflective only of obesity. To identify other cardiovascular risk factors, a fasting lipid panel and fasting glucose level should be obtained in children who are overweight and have blood pressure between the 90th and 94th percentile and in all children with blood pressure above the 95th percentile.
Because of the associations with hyper-tension and the frequency of occurrence of sleep disorders, particularly among over-weight children, a history of sleeping pat-terns should be obtained in a child with hypertension. One practical strategy for identifying children with a sleep problem or sleep disorder is to obtain a brief sleep history, using an instrument called BEARS, the components of which include Bedtime problems, Excessive daytime sleepiness, Awakenings during the night, Regularity and duration of sleep, and Snoring.
Secondary Hypertension
Secondary hypertension is more common in children than in adults. The possibility that some underlying disorder may be the cause of the hypertension should be considered in every child or adolescent who has elevated blood pressure. Very young children, children with stage 2 hypertension, and children or adolescents with clinical signs that suggest the presence of systemic conditions associated with hypertension should be evaluated more extensively than those with stage 1 hypertension.
Medical history should elicit information to focus the subsequent evaluation and to uncover definable causes of hypertension. Questions should be asked about previous hospitalizations, trauma, urinary tract infections, and snoring and other sleep problems. Questions should address family history of hypertension, diabetes, obesity, sleep apnea, renal disease, and other cardiovascular diseases. Many drugs can increase blood pres- sure, so physicians should ask directly about the use of over-the-counter and prescription medication, illicit drugs, and nutritional supplements (particularly those that aim to enhance athletic performance).
The physical examination should assess the child's height, weight, and body mass index. Poor growth may indicate an under-lying chronic illness. When hypertension is confirmed, blood pressure should be measured in both arms and in a leg. Normally, blood pressure is 10 to 20 mm Hg higher in the legs than in the arms. If the leg blood pressure is lower than the arm blood pres-sure or if femoral pulses are weak or absent, coarctation of the aorta may be present. Obesity alone is an insufficient explanation for diminished femoral pulses in the presence of high blood pressure.
Target-Organ Abnormalities
Target-organ abnormalities are commonly associated with hypertension in children and adolescents, with left ventricular hypertrophy (LVH) providing the most prominent evidence of target-organ damage. The presence of LVH is an indication to initiate or intensify antihypertensive therapy. LVH is assessed by echocardiography, and the cut-point is 51 g/m, which is above the 99th percentile in children and adolescents. Pediatric patients with established hypertension should have left ventricular mass assessed (using a formula) at diagnosis and periodically there-after. Ascertainment of left ventricular mass index is helpful in clinical decision-making.
Lifestyle Changes to Lower Blood Pressure
Because hypertension has been linked to obesity, the first line of treatment should be family-based diet and behavior modification. Children should: lose weight; eat more vegetables, fruit, and low-fat dairy products; cut down on salt intake; and reduce their intake of high-calorie food and drinks. Children also should reduce the amount of time spent in sedentary activities, such as playing video games, to less than two hours a day, and they should try to be physically active for 30 to 60 minutes a day. Consultation with a nutritionist may be helpful. Weight control can make treatment with drugs unnecessary, but if drug use is indicated, it should not be delayed.
Drugs to Treat Hypertension
In children, the long-term consequences of untreated hypertension are unknown, and data are unavailable on the long- term effects of antihypertensive drugs on growth, development, or mortality. A definite indication for initiating pharmacologic therapy should therefore be ascertained before a drug is prescribed. The goal for antihypertensive treatment in children should be reduction of blood pressure to less than the 95th percentile. Indications for antihypertensive drug therapy in children include secondary hyper-tension and insufficient response to lifestyle modifications. Pharmacologic therapy should be started with a single drug. Acceptable drug classes for use in children include angiotensin-converting enzyme (ACE) inhibitors, angiotensin- receptor blockers, beta blockers, calcium channel blockers, and diuretics. Hypertensive emergencies can be treated with intravenous antihypertensive drugs.
The child should be started on the lowest recommended dosage, which is increased until the desired blood pressure is reached. Once the highest recommended dosage is reached, or if the child experiences side effects, a second drug from a different class should be added. Ongoing monitoring for target-organ damage should be performed. If possible, in selected patients (such as obese patients who lose weight), the drug should be stepped down and, if possible, withdrawn, although ongoing blood pres-sure monitoring should be performed to determine a recurrence.
Use of the following drugs to treat hyper-tension in children is supported by research:
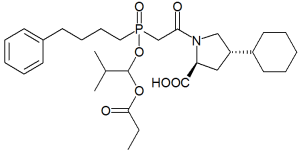
* ACE inhibitors: benazepril, captopril, enalapril, fosinopril, lisinopril, quinapril.
* Angiotensin-receptor blockers: irbesartan, losartan.
* Alpha and beta blocker: labetalol.
* Beta blockers: atenolol, bisoprolol/hydrochlorothiazide (HCTZ), metoprolol, propranolol.
* Calcium-channel blockers: amlodipine, felodipine, isradipine, extended-release nifedipine.
* Central alpha-agonists: clonidine.
* Diuretics: HCTZ, chlorthalidone, furosemide, spironolactone, triamterene, amiloride.
* Peripheral alpha antagonists: doxazosin, prazosin, terazosin.
* Vasodilators: hydralazine, minoxidil.
For severe hypertension, the most useful drugs are esmolol, hydralazine, labetalol, nicardipine, and sodium nitroprusside. Occasionally, useful drugs, mostly used in urgent situations, are clonidine, enalaprilat, fenoldopam, isradipine, and minoxidil. However, most of these must be administered intravenously.
COPYRIGHT 2005 American Academy of Family Physicians
COPYRIGHT 2005 Gale Group