Study objective: To evaluate whether the discontinuation of furosemide treatment resulted in a decrease in PaC[O.sub.2] and an increase in daytime and nocturnal oxygenation.
Background: Furosemide is widely prescribed in patients with COPD for the treatment of peripheral edema. It is known that furosemide causes a metabolic alkalosis. A diminished chemoreceptor stimulation may cause a decreased alveolar ventilation.
Design: Randomized, double-blind, placebo-controlled, crossover trial.
Setting: Department of Pulmonology, Rijnstate Hospital Arnhem, the Netherlands.
Patients: Twenty patients with stable COPD (10 men; median age, 70 years [range, 58 to 81 years]; FE[V.sub.1] 35% predicted [range, 19 to 70% predicted]). Subjects were included if they had received furosemide, 40 mg/d, for the treatment of peripheral edema for at least a month and if they had a mean nocturnal arterial oxygen saturation (Sa[O.sub.2]) < 92%. Patients with cardiac left and/or right ventricular dysfunction, sleep apneas, and patients receiving other diuretics, angiotensin-converting enzyme inhibitors, potassium or chloride replacement therapy, or long-term oxygen treatment were excluded.
Intervention: Furosemide was discontinued for 1 week and replaced by placebo treatment in the first or the second week.
Measurements and results: Ventilation, daytime arterial blood gas levels, and nocturnal Sa[O.sub.2] were measured at baseline, after 1, and after 2 weeks. Sixteen subjects completed the study. Ventilation increased from 10.4 L/min (range, 6.7 to 15.4 L/min) at baseline to 11.6 L/min (range, 8.7 to 14.0 L/min) after discontinuation of furosemide (p < 0.05). PaC[O.sub.2] decreased from 45 mm Hg (range, 35 to 64 mm Hg) to 41 mm Hg (range, 32 to 61 mm Hg; p < 0.01). Daytime and nocturnal oxygenation did not improve.
Conclusions: Although it does not improve oxygenation, the discontinuation of furosemide decreases PaC[O.sub.2] in patients with COPD.
Key words: COPD; furosemide; hypercapnia; hypoventilation; metabolic alkalosis
Abbreviations: BE = base excess; EMG = electromyography; EOG = electro-oculography; KCO = transfer capacity for carbon monoxide corrected for alveolar volume; NS = not significant; PEmax = maximum expiratory mouth pressure; PImax = maximum inspiratory mouth pressure; REM = rapid eye movement; RVSP = right ventricular systolic pressure; Sa[O.sub.2] = arterial oxygen saturation; TLCO = transfer capacity for carbon monoxide
**********
Peripheral edema occurs in a substantial number of patients with COPD, especially in those with hypercapnia and hypoxemia. (1-3) Usually this is treated with loop diuretics. Loop diuretics induce a metabolic alkalosis by increasing urinary H+ loss due to secondary hyperaldosteronism and due to a contraction of the extracellular volume around a constant amount of extracellular bicarbonate. (4) The consequent metabolic alkalosis will cause a diminished chemoreceptor stimulation (5,6) and, as a result, reduced alveolar ventilation. (7,8) The clinical relevance of a metabolic alkalosis in patients with COPD was already reported by Bear et al. (9) In the described patients, blood gas levels and clinical symptoms benefited from the correction of metabolic alkalosis. However, this was an uncontrolled study and the initial metabolic alkalosis was due to several causes. The effect of loop diuretic-induced alkalosis has only been described in an animal study. Furosemide was found to decrease ventilation in young rabbits. (10) The effect of loop diuretic-induced alkalosis on ventilation in patients with COPD has not been studied yet. Moreover, no placebo-controlled studies have been performed to evaluate the benefit of the correction of alkalosis in COPD patients. A decreased ventilation caused by loop diuretics may increase PaC[O.sub.2]. It is of clinical relevance to evaluate the potential increase in PaC[O.sub.2] due to loop diuretics, as hypercapnia is believed to be an ominous sign for morbidity and mortality. (11-13) A decreased ventilation could also decrease the oxygenation. This may be more pronounced at night, since hypoventilation is often seen during sleep in patients with COPD. (14-18) Loop diuretics may progress the level of hypoventilation during sleep and cause a further deterioration of the nocturnal hypoxemia. Furosemide, prescribed for peripheral edema, was discontinued in COPD patients with nocturnal hypoxemia in a double-blind, placebo-controlled design. It was hypothesized that the discontinuation of loop diuretics would result in a decrease in PaC[O.sub.2] and an increase in daytime and nocturnal oxygenation.
MATERIALS AND METHODS
Subjects
The study was performed in 20 patients with COPD (10 men; median age, 70 years [range, 58 to 81 years]; median FE[V.sub.1], 35% predicted [range, 19 to 70% predicted]). (19) Subjects were included if they had a stable course of the disease. COPD was defined according to the standards of the American Thoracic Society, (20) and a disease stability was defined as a fluctuation of FE[V.sub.1] of < 10% over the last 6 months and an absence of exacerbations for at least 8 weeks prior to the study. Moreover, subjects were only included if they had received furosemide for the treatment of peripheral edema for at least 1 month. Subjects also needed to have a mean nocturnal arterial oxygen saturation (Sa[O.sub.2]) < 92%, because a decrease in alveolar ventilation will cause a substantial fall in Sa[O.sub.2] if the Sa[O.sub.2]/Pa[O.sub.2] relationship lies on the shoulder or on the steep part of the oxygen saturation curve.
Subjects were excluded if they had a history of another pulmonary disease, left ventricular dysfunction, obstructive and/or central sleep apneas, or if they received long-term oxygen treatment, other types of diuretics, angiotensin-converting enzyme inhibitors, potassium, or chloride replacement therapy. Other exclusion criteria were hypokalemia or hypovolemia, in order to rule out other causes of metabolic alkalosis. A left ventricular dysfunction was defined as an echoscopic left ventricular end-diastolic diameter > 58 mm, and/or an end-systolic diameter > 44 mm. and/or a moderate-to-severe valvular disease. As withdrawing diuretics may worsen the general condition of patients with cor pulmonale, subjects were also excluded if they had a right ventricular systolic pressure (RVSP) > 35 mm Hg. Subjects with a borderline-increased RVSP between 30 mm Hg and 35 mm Hg were only included if they had no clinical signs of edema (n = 3). A sleep apnea or hypopnea syndrome was defined as an apnea/hypopnea index > 15/h. (21) The study protocol was approved by the local hospital ethical committee. A signed and dated informed consent was obtained from all subjects.
Study Design
Before the start of the study, all subjects received furosemide for the treatment of peripheral edema. This was then replaced by capsules containing furosemide (40 mg) or identical capsules containing placebo. A crossover design was used, with a total duration of 2 weeks: 1 week of furosemide and 1 week of placebo, in random order. Subjects visited the lung function laboratory at baseline, after 1 week, and after 2 weeks. Between visits, subjects measured their body weight daily at home. Subjects were instructed to contact the study investigator in case of an increase in body weight of > 0.5 kg/d or in case of worsening of dyspnea. Other medications remained unchanged during the study. Urine samples were obtained at each visit to check the compliance to study medication.
Selection Phase
Nocturnal Sa[O.sub.2] was measured initially at home by pulse oximetry (8500M; Nonin Medical; Plymouth, MN) by using a finger probe. Sa[O.sub.2] values were stored in memory and processed afterwards (software version NN856 03/95; PROFOX Associates; Escondido, CA). Echocardiography was evaluated by the Power Vision apparatus (Toshiba Corporation Medical Systems Company; Tokyo, Japan). The consecutive polysomnography in the hospital (Voyageur; Nicolet Biomedical; Madison, WI) consisted of EEG, electromyography (EMG), and electro-oculography (EOG) measurements, airflow thermistor (Infinity sensor 1450; New Life Technologies; Midlothian, VA), thoracoabdominal movements (1482; Pro-Tech Services; Woodinville WA), and nocturnal Sa[O.sub.2]. The sleep states were assessed manually. (22)
Study Phase
Measurements performed at baseline, after 1 week, and after 2 weeks consisted of lung function tests; arterial blood gas sampling; nocturnal oximetry with measurements of EEG, EMG, and EOG; measurements of body fluid homeostasis; and collection of urine samples. Tidal volume, breathing frequency, and minute ventilation were measured by spirometry (Pulmonet III; SensorMedics; Yorba Linda, CA). Variables were measured over 5 min at the same time each day, in a quiet room, in supine position, after 15 min of rest, and without consumption of coffee. The ventilatory response to hypercapnia was tested under normoxic conditions by the steady-state method. (23,24) Subjects were connected to a closed spirometry circuit, in which the carbon dioxide level could be increased by adjusting a three-way valve, partially short-circuiting a carbon dioxide absorber in the inspiratory limb of the circuit. The increase in end-tidal carbon dioxide tensions was measured with a sampling capnograph (Multicap; Datex Instrumentarium; Helsinki, Finland). Minute ventilation was measured simultaneously (Pulmonet III; SensorMedics). The total transfer capacity for carbon monoxide (TLCO) and the TLCO corrected for alveolar volume (KCO) were measured by the single-breath method (2450; SensorMedics). (25) The respiratory muscle function was evaluated by measurements of maximal inspiratory mouth pressure (PImax) and maximal expiratory mouth pressure (PEmax) [microMPM; SensorMedics].
Arterial blood gas samples were obtained under the same circumstances as during measurements of resting ventilation (IL 1620; Instruments Laboratory; Milano, Italy). The method for measuring bicarbonate was independent from that for PaC[O.sub.2]. The alveolar-arterial oxygen gradient was calculated using the alveolar gas equation, assuming an r value of 0.8.
Nocturnal oximetry was performed at home during the night preceding the visit, by means of the same portable pulse oximeter as during the selection phase. Subjects were instructed to switch the oximeter on and off at the same time each night to match the recorded time during the nights. EEG, EMG, and EOG (Oxford Medical 9000; Oxford Instruments Medical Systems; Abingdon, Oxfordshire, UK) were recorded to assess the quality of sleep. The level of nocturnal hypoxemia was evaluated by the mean Sa[O.sub.2, the time in hypoxemia (Sa[O.sub.2] < 90%), and the time in desaturation (Sa[O.sub.2] > 4% below baseline awake, defined as the first 5 min of the recording). The variables were calculated for the entire night, for actual sleep, and for actual rapid eye movement (REM) sleep, providing a standardization for the stage of sleep.
Body weight was measured after voiding at the same time each visit (Seca 761; Vogel Halke; Hamburg, Germany). The volume of the lower legs was calculated from the displacement of water after immersion of the feet in a standardized water bath (26) This method provides an accurate evaluation of differences in peripheral edema. Urinary furosemide analysis was done qualitatively using high-performance liquid chromatography and diode array detection.
Statistical Analysis
Stratistical software (SPSS version 9.0; SPSS; Chicago, IL) was used for statistical analysis. The Wilcoxon signed rank test was used to test differences between variables before and after discontinuation of furosemide. The Spearman correlation was used to perform bivariate correlation analysis.
The decrease in PaC[O.sub.2] after discontinuation of furosemide was correlated to several baseline variables to determine if the outcome of correcting alkalosis could be predicted. The next variables were chosen: blood gas values, the ventilatory response to hypercapnia, FE[V.sub.1], respiratory muscle function, and minute ventilation as a fraction of the maximal voluntary ventilation. A p value < 0.05 was considered significant. All results are expressed as median (range).
RESULTS
Sixteen subjects completed the study. Urine analysis showed a full compliance with respect to the study medication. Of the four subjects who did not complete the study, one patient had a weight gain of 3.5 kg after 4 days without furosemide, associated with an increase in peripheral edema and worsening of dyspnea; two patients were not willing to continue the study; and one patient became unstable during the study: terminal respiratory failure (FE[V.sub.1], 29% predicted; PaC[O.sub.2], 62 mm Hg) aggravated by a pulmonary tract infection developed in this patient, and she died shortly after the study. The death was unlikely associated with the withdrawal of furosemide.
Of the subjects who had a borderline-increased RVSP, one patient did not complete the study (the subject with terminal respiratory failure). The other two patients continued the study without complications. The mean potassium level of the subjects who entered the study was 4.2 mmol/L (3.5 to 4.8 mmol/L) at baseline.
Lung Function Tests
Discontinuation of furosemide caused an increase in minute ventilation from 10.4 L/min (6.7 to 15.4 L/min) to 11.6 L/min (8.7 to 14.0 L/min) [p < 0.05]. This could not be derived from a significant increase in tidal volume or breathing frequency (Table 1). The TLCO and the KCO could be measured in nine subjects (53%). The other subjects were not able to perform the breath-holding procedure. No significant differences were found in the ventilatory response to hypercapnia, FE[V.sub.1], TLCO, and KCO, or PImax and PEmax (Table 1).
Blood Gases and Nocturnal Oxygen Saturation
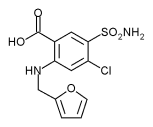
An increased BE and a pH within normal limits were found at baseline, as a reflection of a respiratory-compensated metabolic alkalosis. Correction of the alkalosis was confirmed by a significant decrease in the median BE and bicarbonate levels (Table 2). The median PaC[O.sub.2] value decreased from 45 mm Hg (35 to 64 mm Hg) to 41 mm Hg (32 to 61 mm Hg) [p < 0.01]. The individual values are presented in Figure 1.
[FIGURE 1 OMITTED]
The effect of a 1-week reintroduction of furosemide could be evaluated in the subjects who randomly received placebo in the first week and furosemide in the second week (n = 10). The PaC[O.sub.2] after a 1-week reintroduction was 42 mm Hg (39 to 64 mm Hg), as compared to 44 mm Hg (39 to 63 mm Hg) at baseline (not significant [NS], p = 0.08) and 41 mm Hg (37 to 61 mm Hg) after 1 week of placebo (NS, p = 0.15). This was associated by a BE of 3.7 mmol/L (0.2 to 7.9 mmol/L) after reintroduction, as compared to 3.7 mmol/L (0.1 to 7.9 mmol/L) at baseline (NS) and 1.8 mmol/L (0.5 to 8.3 mmol/L) after placebo treatment (p < 0.05).
No improvement in oxygenation was found. The alveolar-arterial oxygen gradient increased significantly from 26 mm Hg (10 to 37 mm Hg) to 32 mm Hg (13 to 38 mm Hg) [p < 0.05]. The quality of sleep during the different nights was comparable (Table 3), allowing a reliable comparison of nocturnal [Sa[O.sub.2] values during the different nights. No differences in the variables of nocturnal Sa[O.sub.2] during the entire night were found (Table 3). The same Sa[O.sub.2] variables, determined for the actual sleep and for REM sleep specifically, were also not statistically significant with and without furosemide treatment.
Body Fluid Homeostasis
The body weight increased from 74.0 to 74.5 kg (0 to 3.0 kg; p < 0.05). The increase could be attributed to 5 of the 16 subjects (31%) in whom an increase in body weight was found with a range of 1.0 to 3.0 kg. The median leg volume increased from 2,609 mL (2,067 to 2,948 mL) to 2,632 mL (2,037 to 3,036 mL) [p < 0.01].
Predictors for Response to Correction of Alkalosis
No significant correlation was found between the decrease in PaC[O.sub.2] and baseline variables, including blood gas values, ventilatory response to hypercapnia, FE[V.sub.1], ventilation/maximal voluntary ventilation, PImax, or PEmax.
DISCUSSION
The discontinuation of furosemide, prescribed for peripheral edema in patients with stable COPD with a mean nocturnal Sa[O.sub.2] < 92%, resulted in an increased minute ventilation and a decrease in PaC[O.sub.2]. This was not associated with an increase in daytime or nocturnal oxygenation.
The increased BE, accompanied by a normal pH, confirms a respiratory-compensated metabolic alkalosis at baseline. The correction of the alkalosis, due to the withdrawal of furosemide, resulted in decreased BE and bicarbonate levels and a decrease in the median PaC[O.sub.2] of 4 mm Hg. Because no significant correlations were found between the baseline blood gas values or between other variables, reflecting respiratory failure, chemoreceptor sensitivity, the ability to generate ventilatory reserve, and the decrease in PaC[O.sub.2], baseline characteristics predicting the benefit of correction of alkalosis could not be determined.
Apart from the effect on the metabolic acid-base status, furosemide treatment also lowers plasma potassium levels. Some investigators (27) hypothesized that potassium will also stimulate ventilation via peripheral chemoreceptors. Consequently, stopping furosemide treatment might increase serum plasma levels and thus stimulate ventilation. However, our group has brought forward experimental evidence that serum potassium levels are not very relevant in the control of breathing of COPD patients, (28) confirming the work of others in resting normal subjects. (29) At the start of the study, we had established that serum potassium levels were within the normal range. Thus, it is not really possible to separate supposed effects of changes in fixed acid or in potassium on the control of breathing in our patient group. Irrespective of the mechanism, ventilation increases and PaC[O.sub.2] decreases after stopping furosemide treatment in patients with COPD.
The daytime and nocturnal oxygenation did not improve after the discontinuation of furosemide. The oxygen diffusion capacity may have decreased, due to retention of pulmonary interstitial fluid in the absence of diuretic therapy. If so, this is interesting because patients with cardiac failure were excluded explicitly in our study. A decrease in diffusion capacity was not apparent from the transfer capacity for carbon monoxide, but these measurements could only be performed in 53% of the subjects. A worsened ventilation-perfusion mismatch may also have occurred, for example, due to a lower functional residual capacity, reduced airway clearance, or bronchial wall thickening. Results of lung function tests, however, showed no significant changes. A combination of factors was probably present in the individual subjects. The ventilatory response to hypercapnia was low in these subjects, implying a low chemoreceptor sensitivity. This could explain why the differences in ventilation and in PaC[O.sub.2] were rather low in some of the subjects. Therefore, only a marginal advantageous effect on the oxygenation may have occurred in some subjects, which was easily counteracted by a worsening in diffusion capacity and/or ventilation-perfusion mismatch. The increase in alveolar-arterial oxygen gradient suggests a worsened diffusion capacity for oxygen and/or a worsened ventilation-perfusion mismatch. However, it needs to be noted that the used equation has a major shortcoming because a fixed r value of 0.8 was assumed. In fact, the r value may have changed, as the level of PaC[O.sub.2] was unequal in both situations.
The discontinuation of furosemide had no statistically significant effect on the ventilatory response to hypercapnia or the respiratory muscle function, but it needs to be remarked that the sample size (n = 16) may have been too small to detect small effect. Subjects were cardiac screened before selected to enter the study, to rule out the risk of heart failure in absence of furosemide. The study can therefore not be used to estimate the safety of discontinuing loop diuretics in patients with COPD in general. An increase in peripheral edema was found, which was not surprising, as furosemide was prescribed for the treatment of peripheral edema. However, it is interesting to note that only a marginal increase in peripheral edema was found, suggesting that the increase was of statistical but not of clinical relevance. The extra vascular fluid retention, shown by the increase in the lower leg volume, was not necessarily accompanied by an increase in body weight. In a previous study, (26) we found a poor correlation between peripheral edema and body weight. A shift between the intravascular and the extravascular compartment may have occurred, accompanied by a total amount of body fluid that remained equal.
The results are in agreement with previous studies (7,8) demonstrating hypoventilation in response to metabolic alkalosis. No relationship between metabolic alkalosis and hypoventilation was found in other studies, (30) but this can probably be explained by an inappropriate induction of the alkalosis, or to a higher degree of ventilation due to stress, fever, infection, or pre-existing tachypnea. (8) A clear ventilatory benefit after correction of alkalosis was found in our group of COPD patients. This was reported earlier, but only in an uncontrolled study, evaluating alkalosis of various origins. (9) The present results showed no statistically significant correlations between baseline blood gas values and the decrease in PaC[O.sub.2]. Earlier studies in humans already showed a wide 95% confidence interval in PC[O.sub.2] in response to increased bicarbonate levels. (31) Moreover, the ventilatory response to metabolic alkalosis may be even harder to examine in disorders associated with hyperventilation. (8) It seems that patients who will benefit from the correction of alkalosis are difficult to recognize.
It was already noted that hypoventilation in response to metabolic alkalosis has serious implications in patients with high PaC[O.sub.2] and low Pa[O.sub.2]. (8,9) COPD patients with a tendency toward hypercapnia require extra attention, as hypercapnia is believed to be an ominous sign for morbidity and mortality. (11-13) Moreover, the increased level of PaC[O.sub.2] due to furosemide treatment may cause an increased tendency toward fluid retention, which may counteract the diuretic effects of furosemide. The increase in PaC[O.sub.2] is of clinical relevance, especially if it is taken into consideration that loop diuretics are prescribed in a substantial number of COPD patients and usually for a long period of time. If there is an indication for diuretic therapy in a COPD patient, other types of diuretics need to be considered. Spironolactone, causing no acid/base shift, or acetazolamide, causing a metabolic acidosis, could be better alternatives. It needs to be emphasized that loop diuretics are often beneficial in patients with cor pulmonale. In these patients, acetazolamide could be added to loop diuretics to counteract the metabolic alkalosis. (32)
The effect of reintroduction of furosemide for 1 week could be evaluated in the 10 subjects who randomly received placebo in the first week and furosemide in the second week. As expected, the PaC[O.sub.2] increased after reintroduction, but it did not reach the baseline level. Although this difference did not reach statistical significance, it could suggest that if given longer even higher increases in PaC[O.sub.2] could be seen. However, it needs to be remarked that this was observed in only a small number of subjects. In conclusion, this study shows that the discontinuation of furosemide, prescribed for the treatment of peripheral edema, lowers PaC[O.sub.2] in patients with COPD.
REFERENCES
(1) Anand IS, Chandrashekhar Y, Ferrari R, et al. Pathogenesis of congestive state in chronic obstructive pulmonary disease: studies of body water and sodium, renal function, hemodynamics, and plasma hormones during edema and after recovery. Circulation 1992; 86:12-21
(2) MacNee W. Pathophysiology of cor pulmonale in chronic obstructive pulmonary disease: part two. Am J Respir Crit Care Med 1994; 150:1158-1168
(3) MacNee W. Pathophysiology of cor pulmonale in chronic obstructive pulmonary disease: part one. Am J Respir Crit Care Med 1994; 150:833-852
(4) Rose BD. Diuretics. Kidney Int 1991; 39:336-352
(5) Pokorski M, Lahiri S. Inhibition of aortic chemoreceptor responses by metabolic alkalosis in the cat. J Appl Physiol 1982; 53:75-80
(6) Pokorski M, Lahiri S. Relative peripheral and central chemosensory responses to metabolic alkalosis. Am J Physiol 1983; 245:873-880
(7) Javaheri S, Shore NS, Rose B, et al. Compensatory hypoventilation in metabolic alkalosis. Chest 1982; 81:296-301
(8) Javaheri S, Kazemi H. Metabolic alkalosis and hypoventilation in humans. Am Rev Respir Dis 1987; 136:1011-1016
(9) Bear R, Goldstein M, Phillipson E, et al. Effect of metabolic alkalosis on respiratory function in patients with chronic obstructive lung disease. Can Med Assoc J 1977; 117:900-903
(10) Hazinski TA. Furosemide decreases ventilation in young rabbits. J Pediatr 1985; 106:81-85
(11) Cooper CB. Life expectancy in severe COPD. Chest 1994; 105:335-337
(12) Costello R, Deegan P, Fitzpatrick M, et al. Reversible hypercapnia in chronic obstructive pulmonary disease: a distinct pattern of respiratory failure with a favorable prognosis. Am J Med 1997; 102:239-244
(13) Foucher P, Baudouin N, Merati M, et al. Relative survival analysis of 252 patients with COPD receiving long-term oxygen therapy. Chest 1998; 113:1580-1587
(14) Becker HF, Piper AJ, Flynn WE, et al. Breathing during sleep in patients with nocturnal desaturation. Am J Respir Crit Care Med 1999; 159:112-118
(15) Fletcher EC, Gray BA, Levin DC. Nonapneic mechanisms of arterial oxygen desaturation during rapid-eye-movement sleep. J Appl Physiol 1983; 54:632-639
(16) Fletcher EC, Scott D, Qian W, et al. Evolution of nocturnal oxyhemoglobin desaturation in patients with chronic obstructive pulmonary disease and a daytime Pa[O.sub.2] above 60 mm Hg. Am Rev Respir Dis 1991; 144:401-405
(17) Hudgel DW, Martin RJ, Capehart M, et al. Contribution of hypoventilation to sleep oxygen desaturation in chronic obstructive pulmonary disease. J Appl Physiol 1983; 55:669-677
(18) Stradling JR, Lane DJ. Nocturnal hypoxaemia in chronic obstructive pulmonary disease. Clin Sci 1983; 64:213-222
(19) Quanjer PH, Tammeling GJ, Cotes JE, et al. Lung volumes and forced ventilatory flows. Work Group on Standardization of Respiratory Function Tests. European Community for Coal and Steel. Official position of the European Respiratory Society. Rev Mal Respir 1994; 11:5-40
(20) Standards. for the diagnosis and care of patients with chronic obstructive pulmonary disease (COPD) and asthma. Am Rev Respir Dis 1987; 136:225-244
(21) Collard P, Dury M, Delguste P, et al. Movement arousals and sleep-related disordered breathing in adults. Am J Respir Crit Care Med 1996; 154:454-459
(22) Stradling JR. Sleep studies for sleep-related breathing disorders. J Sleep Res 1992; 1:265-273
(23) Folgering HT, Bernards JA, Biesta JH, et al. Mathematical analysis of the response of lung ventilation to C[O.sub.2] in normoxia and hyperoxia. Pflugers Arch 1974; 347:347-350
(24) Smolders FD, Folgering HT, Bernards JA. Capnostat and Oxystat: electronic devices to automatically maintain the end-tidal PC[O.sub.2] and P[O.sub.2] of a subject connected to a closed respiratory circuit at adjustable levels. Pflugers Arch 1977; 372:289-290
(25) Cotes JE, Chinn DJ, Quanjer PH, et al. Standardization of the measurement of transfer factor (diffusing capacity). Rev Mal Respir 1994; 11:41-52
(26) Brijker F, Heijdra YF, Van Den Elshout FJ, et al. Volumetric measurements of peripheral oedema in clinical conditions. Clin Physiol 2000; 20:56-61
(27) Paterson DJ. Potassium and ventilation in exercise. J Appl Physiol 1992; 72:811-820
(28) Rooijackers JM, Dekhuijzen PN, van Herwaarden CL, et al. Potassium and ventilation during positive and negative work in patients with COPD. Clin Physiol 1997; 17:475-485
(29) Qayyum MS, Barlow CW, O'Connor CF, et al. Effect of raised potassium on ventilation in euoxia, hypoxia and hyperoxia at rest and during exercise in man. J Physiol 1994; 476:365-372
(30) Miller PD, Berns AS. Acute metabolic alkalosis perpetuating hypercarbia: a role for acetazolamide in chronic obstructive pulmonary disease. JAMA 1977; 238:2400-2401
(31) Arbus GS. An in vivo acid-base nomogram for clinical use. Can Med Assoc J 1973; 109:291-293
(32) Dickinson GE, Myers ML, Goldbach M, et al. Acetazolamide in the treatment of ventilatory failure complicating acute metabolic alkalosis. Anesth Analg 1981; 60:608-610
* From the Department of Pulmonary Diseases (Drs. Brijker and van den Elshout), Rijnstate Hospital Arnhem; and Department of Pulmonology Dekkerswald (Drs. Heijdra and Folgering), University of Nijmegen, Nijmegen, the Netherlands.
The study was supported by GlaxoWellcome, Zeist, the Netherlands.
Manuscript received October 25, 2000; revision accepted July 27, 2001.
Correspondence to: Folkert Brijker, MD, PhD, Department of Pulmonary Diseases, Rijnstate Hospital, PO Box 9555, 6800 TA Arnhem, the Netherlands; e-mail: zonnebloem@compuserve.com
COPYRIGHT 2002 American College of Chest Physicians
COPYRIGHT 2002 Gale Group