Study objectives: Effects of chronic metabolic alkalosis and acidosis and their relation to central chemoregulation may differ between normocapnic and chronic hypercapnic patients with COPD. The relationship between responses of inspired ventilation (VI), mouth occlusion pressure ([P.sub.0.1]), and cerebral blood volume (CBV), to short-term changes in arterial PC[O.sub.2] was measured.
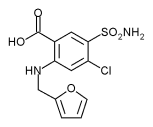
Patients and methods: Seventeen patients with chronic hypercapnia and COPD (PaC[O.sub.2] > 6.0 kPa) and 16 normocapnic patients with COPD (PaC[O.sub.2] [less than or equal to] 6.0 kPa) [FE[V.sub.1] 27% predicted] were studied under baseline metabolic conditions and after 1 week of treatment with oral furosemide, 40 mg/d, or acetazolamide, 500 mg/d. Hypercapnia (change in end-tidal carbon dioxide > 1 kPa) was induced by administering adequate amounts of carbon dioxide in the inspired air. CBV was measured using near-infrared spectroscopy.
Results: Compared with baseline metabolic condition, chronic metabolic acidosis and alkalosis did not change ventilatory ([DELTA]VI/[DELTA]PaC[O.sub.2]) and cerebrovascular ([DELTA]CBV/[DELTA]PaC[O.sub.2]) reactivity. Base excess (BE) decreased by 6.8 [+ o r -] 1.1 mEq/L and 6.9 [+ or -] 1.6 mEq/L, respectively, in the normocapnic and chronic hypercapnic COPD groups during metabolic acidosis, resulting in a not-quite-significant leftward shift of both the ventilatory and cerebrovascular carbon dioxide response curve. BE increased by 2.3 [+ or -] 1.2 mEq/L and 1.2 [+ or -] 1.3 mEq/L, respectively, during chronic metabolic alkalosis in both COPD groups, without concomitant shift. Poor correlations between ventilatory and cerebrovascular carbon dioxide responsiveness ([DELTA]CBV/[DELTA]PaC[O.sub.2] and [DELTA]VI/[DELTA]PaC[O.sub.2], [DELTA]CBV/[DELTA]PaC[O.sub.2] and [DELTA][P.sub.0.1]/[DELTA]PaC[O.sub.2], respectively) were found irrespective of baseline, respiratory condition, and induced metabolic state.
Conclusions: Normocapnic and chronic hypercapnic COPD patients have the same ventilatory and cerebrovascular carbon dioxide responsiveness irrespective of induced metabolic state.
Key words: acid-base; central chemosensitivity; cerebral blood volume; control of breathing; COPD; metabolic acidosis; metabolic alkalosis; mouth occlusion pressure; near-infrared spectroscopy
Abbreviations: BE = base excess; CBF = cerebral blood flow; CBV = cerebral blood volume; MAP = mean arterial pressure; MIP = maximal inspiratory pressure; NIRS = near-infrared spectroscopy; [P.sub.0.1] = mouth occlusion pressure; RR = respiratory rate; VD/VT = dead space ventilation; VI = inspired ventilation
**********
The contribution of cerebral blood flow (CBF) to ventilation has been studied in healthy humans (1-3) and laboratory animals. (4) Patients with COPD are of particular interest. It is poorly understood why there is a difference in carbon dioxide chemoresponsiveness between normocapnic patients with COPD and chronic hypercapnic patients with COPD. Despite similar degrees of airway obstruction, different measures of mouth occlusion pressure ([P.sub.0.1]) and electromyographic parameters of respiratory muscle activity are found, (5) suggesting different central control of carbon dioxide regulation in both COPD groups.
In healthy subjects, an increase in CBF and cerebral blood volume (CBV) lead to increased carbon dioxide washout and central hypocapnia. (6) In addition, as reviewed by Feihl and Perret, (7) both cerebral resistance vessels (arterioles) and capillaries/venules are dilated by hypercapnia. Chronic hypercapnia, however, is associated with a blunted cerebrovascular reactivity to short-term PC[O.sub.2] alterations. (8,9) As a result, only minor changes in CBF and CBV can be expected during the latter condition, an inability to attenuate the short-term hypercapnic stimulus to the central chemoreceptors, and a tendency toward an elevated PC[O.sub.2] in the cerebral interstitial fluid (see Appendix). Consequently, an elevated ventilatory drive could be expected during chronic hypercapnia; however, the opposite, a lowered ventilatory drive, is found. (5,10)
Cerebrovascular responses to hypercapnia, expressed as a [DELTA]CBV, were studied in their relationship to ventilatory responses in normocapnic and chronic hypercapnic patients with COPD, using the noninvasive technique of near-infrared spectroscopy (NIRS). We hypothesized an inverse relationship between cerebrovascular reactivity ([DELTA]CBV/[DELTA]PaC[O.sub.2]) and ventilatory reactivity (change in inspired ventilation [VI]/[DELTA]PaC[O.sub.2]). Patients with chronic hypercapnia are thought to have a high vasodilatory response to PC[O.sub.2]/pH, keeping the extracellular fluid of the brain less hypercapnic, thus keeping the central chemoreceptor-mediated ventilatory drive relatively low, and resulting in systemic hypercapnia. In the normocapnic group, the cerebrovascular response to carbon dioxide might be less, leading to a higher extracellular fluid PC[O.sub.2] and resulting in a normal (high) ventilatory drive.
Because chronic respiratory acidosis is usually compensated via metabolic pathways, in the present study we investigated the effects of superimposed chronic metabolic acid-base changes on the control of cerebrovascular and ventilatory responses. Therefore, a chronic metabolic acidosis and alkalosis was induced by orally administrated acetazolamide and furosemide, respectively. [P.sub.0.1] and its response to changes of PC[O.sub.2] ([DELTA][P.sub.0.1]/[DELTA]PaC[O.sub.2]) were measured to approximate the ventilatory drive independent of airway resistance and related to CBV responsiveness.
MATERIALS AND METHODS
Subjects
The study was performed on 33 patients with COPD as defined by the American Thoracic Society. Ten men and 6 women, aged 60 [+ or -] 11 years, were normocapnic (PaC[O.sub.2] [less than or equal to] 6.0 kPa); 15 men and 2 women, aged 63 [+ or -] 8 years, were hypercapnic (PaC[O.sub.2] > 6.0 kPa). Patients were excluded if they: (1) had evidence of obstructive sleep disorders or restrictive pulmonary function, or had a history of cardiopulmonary, cerebrovascular, or other chronic diseases; (2) had an exacerbation in the 6 weeks before enrollment; and (3) received additional medications other than pulmonary bronchodilating agents, theophyllines, and (systemic) corticosteroids. Three normocapnic and two hypercapnic patients were current smokers; all other patients stopped smoking for > 6 months. A description of the patients is presented in Table 1.
At least 2 h before the experiments, all participants had to abstain from caffeinated drinks and cigarettes, but were allowed to continue their pulmonary medications. All volunteers gave informed consent. The study was approved by the ethical committee of the Department of Pulmonology Dekkerswald, University Medical Center Nijmegen, The Netherlands.
Patients were studied on 3 separate days, during induced-acidosis, induced-alkalosis, and baseline (control) conditions, respectively, in random order. Metabolic acidosis was induced by orally administrated acetazolamide, 250 mg q12h for 1 week. Metabolic alkalosis ;vas induced by orally administrated furosemide, 40 mg/d for 1 week.
Measurements
Ventilation Measurements: The subjects were positioned in a comfortable, reclining position. They were breathing through a face mask with low-resistance valves for inspiratory and expiratory gas mixture. First, dead space ventilation (VD/VT) was measured using the Bohr equation. Expired air was collected in a Douglas bag for 10 min for measurements of mean expiratory PC[O.sub.2] (Capnograph N1000; Nellcor Puritan Bennett; St. Louis, MO). Next, the inspiratory port of the mask was connected via a Fleisch No. 3 pneumotachograph to an inspiratory reservoir. The flow signal was electrically integrated into volume to calculate inspired ventilation (VI). End-tidal carbon dioxide (kilopascals) and respiratory rate (RR) [breaths per minute] were measured at the expiratory port of the mask. Changes in the inspiratory gas mixture of oxygen, nitrogen, and carbon dioxide were induced using a computer-controlled mass-flow system (Bronckhorst-Hitec; Veenendaal, The Netherlands). The fraction of inspired oxygen was monitored continuously using an oxygen analyzer (OM-11; Beckmann; Fullerton, CA). Fast changes in inspiratory gas mixture could be induced; the aimed changes were reached within one breath. Hypercapnia (change in end-tidal carbon dioxide > 1 kPa) was induced by administering adequate amounts of carbon dioxide (fraction of inspired carbon dioxide, 3 to 5%) in the inspired air.
CBV Measurements: NIRS has been developed to monitor brain oxygenation and dynamics. (11) The theory of NIRS has been described extensively. (12) The technique is based on oxygenation-dependent absorption changes in the blood caused by chromophores, mainly oxyhemoglobin and deoxyhemoglobin. Near-infrared light was carried to and from a pulsed continuous-wave NIRS instrument (Oxymon; Artinis Medical Systems; The Netherlands) through two fiberoptic bundles (optodes) on the left side of the forehead. One optode emits near-infrared light at three different wavelengths, which penetrates through the skull and brain. The receiving optode is positioned at a distance of 5.5 cm from the emitting optode. This distance ensures that most of the extracranial circulation is excluded from the detected signal. (13)
Calculation of CBV was described by Elwell et al (14) and Wyatt et al. (15) A slight change of saturation (approximately 5%) is necessary to quantify CBV. The change of saturation is related to the difference of concentration of hemoglobin chromophores at two levels of saturation. CBV can be calculated when the individual hemoglobin concentration and a fixed constant are taken into account. This constant accounts for the molecular weight of hemoglobin, the cerebral tissue density, and the cerebral vessel/large vessel hematocrit ratio.
[P.sub.0.1] Measurements: Ventilatory effort during inspiration was determined by occlusion pressure at 0.1 s after the start of inspiration. A solenoid valve was positioned in the inspiratory line of the circuit. (16) Closure of the valve during expiration was manually controlled, and the valve automatically opened after the first 100 ms of the occluded inspiration. Five repeated measurements of [P.sub.0.1] were averaged during each carbon dioxide condition. [P.sub.0.1] was expressed both as an absolute value and as a percentage of maximal inspiratory pressure (MIP) to normalize [P.sub.0.1] for the individual differences in inspiratory muscle strength. (17)
Protocol
All patients underwent routine spirometry and analysis of hemoglobin, hematocrit, and resting arterial blood gases to assign the individual patients into the normocapnic and chronic hypercapnic COPD groups. On each of 3 study days, a cannula was introduced in the left brachial artery to collect arterial blood samples during normocapnia and to control the level of induced respiratory hypercapnia (Rapid Lab 855; Chiron Diagnostics Corporation; East Walpole, MA). Arterial oxygen saturation and heart rate were monitored with a pulse oximeter (N200; Nellcor Puritan Bennett), with the sensor attached to the right-frontal forehead.
Duplicate measurements of CBV and [P.sub.0.1] during normocapnia and hypercapnia were performed after a period of 10 min of equilibration. Arterial pressure was measured manually during each carbon dioxide condition. Mean arterial pressure (MAP) was calculated as follows: diastolic pressure + 1/3 x (systolic -- diastolic) pressure. All data (except MAP) were linked directly to the NIRS computer for real-time display and simultaneous storage with the NIRS data.
Statistical Analysis
During the whole experiment, time-averaged values of VI, arterial oxygen saturation, heart rate, and RR were recorded and expressed as mean [+ or -] SD during each carbon dioxide challenge. The latter parameters, anthropometric characteristics, pulmonary function, MAP, and arterial blood gas values under control condition were compared between the two COPD groups using the Mann-Whitney test for two independent samples. Within the COPD groups, values measured under control conditions were compared with values during chronic metabolic acidosis (acetazolamide) and during chronic metabolic alkalosis (furosemide) using the Wilcoxon matched-pair signed-ranks test. For each individual, CBV, VI, and [P.sub.0.1] were plotted against corresponding PaC[O.sub.2] values during each metabolic condition and were subjected to linear regression analysis. Because the statistical method of Kolmogorov and Smirnov, as described in the software (GraphPad Instat; GraphPad Software; San Diego, CA), showed a Gaussian distribution, a paired t test could be used to compare the slopes and intercepts of the linear regression equations during control conditions and both metabolic conditions. The level of statistical significance was set at p < 0.05. All tests should be regarded as explorative because of the multiplicity of tests.
RESULTS
Comparison Between the Normocapnic and Hypercapnic COPD Groups: Control Condition
The anthropometric characteristics and respiratory function data of the patients are summarized in Table 1. The degree of airway obstruction was the same in both COPD groups. Other ventilatory parameters (VI, RR, tidal volume, maximal voluntary ventilation, VD/VT) were similar in both groups (Table 2). Mean [+ or -] SD values of PaC[O.sub.2] were 5.26 [+ or -] 0.27 kPa and 6.27 [+ or -] 0.45 kPa in the normocapnic and chronic hypercapnic COPD groups, respectively, under baseline metabolic conditions. The hypercapnic COPD group showed significantly lower resting Pa[O.sub.2] values. Values of CBV were lower in the normocapnic patients relative to chronic hypercapnic patients (p < 0.01; Table 2).
An equal number of patients in both COPD groups were receiving inhaled salbutamol (5 of 16 normocapnic patients and 6 of 17 chronic hypercapnic patients). To account for medical intervention, average CBV and VI were recalculated after subdividing both COPD groups into users and nonusers of theophyllines and/or oral corticosteroids. Long-term theophylline was received by 9 of 16 normocapnic patients (56%) and by 11 of 17 hypercapnic patients (64%). Four of 16 normocapnic patients and 4 of 17 hypercapnic patients received systemic corticosteroids. In both COPD groups, VI values were not significantly different for users and nonusers of theophylline (10.3 mL/min and 8.9 mL/min in the normocapnic group and 8.5 mL/min and 9.8 mL/min in the chronic hypercapnic group, respectively). In addition, values of VI were not significantly different for users and nonusers of corticosteroids (11.2 mL/ min and 9.3 mL/min in the normocapnic group and 8.8 mL/min and 10.0 mL/min in the chronic hypercapnic group, respectively). CBV was not significantly different in our group of theophylline users, relative to the nonusers in both COPD groups. Furthermore, CBV values measured in corticosteroid users and nonusers were not different.
Both cerebrovascular and ventilatory responses to carbon dioxide ([DELTA]CBV/[DELTA]PaC[O.sub.2] and [DELTA]VI/[DELTA]PaC[O.sub.2] were the same for the chronic hypercapnic group as the normocapnic group (Table 3; Fig 1, 2). Both absolute values of [P.sub.0.1] (Table 2) and its reactivity ([DELTA][P.sub.0.1]/[DELTA]PaC[O.sub.2]; Table 3; Fig 1, 2) were the same in both COPD groups, even after correction for MIP. However, the x-intercept (PaC[O.sub.2] at zero [P.sub.0.1]) was higher (p < 0.05) in the hypercapnic COPD group.
[FIGURES 1-2 OMITTED]
Effects of Chronic Metabolic Acidosis
The degree of metabolic acidosis was reflected in a mean decrease of base excess (BE) of -6.8 [+ or -] 1.1 mEq/L in the normocapnic COPD group and -5.9 [+ or -] 1.6 mEq/L in the chronic hypercapnic COPD group (both p < 0.001). Oral acetazolamide administration induced significant changes of PaC[O.sub.2] compared with the control condition in both COPD groups despite unchanged ventilation in the hypercapnic COPD group. In addition, only the normocapnic COPD group showed a simultaneously significant increased Pa[O.sub.2] value (p < 0.05). Ventilatory ([DELTA]VI/[DELTA]PaC[O.sub.2]), mouth pressure ([DELTA][P.sub.0.1]/[DELTA]PaC[O.sub.2]), and cerebrovascular ([DELTA]CBV/[DELTA]PaC[O.sub.2]) reactivity and corresponding intercepts did not change significantly during metabolic acidosis (Table 3; Fig 1, 2) in both COPD groups.
Effects of Chronic Metabolic Alkalosis
Orally administrated furosemide induced a chronic metabolic alkalosis, with a mean increased [DELTA]BE of 2.3 [+ or -] 1.2 mEq/L (p < 0.001) in the normocapnic COPD group and mean increased [DELTA]BE of 1.2 [+ or -] 1.3 mEq/L (p < 0.05) in the chronic hypercapnic COPD group (Table 2). The mean value of PaC[O.sub.2] increased (p < 0.01) in the normocapnic group despite unchanged ventilation. Furosemide administration lowered Pa[O.sub.2] (p < 0.05) in the hypercapnic COPD group. Normocapnic COPD patients showed the same reactivity of both [DELTA]VI/ [DELTA]PaC[O.sub.2] and [DELTA]CBV/[DELTA]PaC[O.sub.2] as the chronic hypercapnic group (Table 3; Fig 1, 2). Absolute values of [P.sub.0.1] did not differ between both the control condition and metabolic alkalosis, however, its reactivity ([DELTA][P.sub.0.2]/[DELTA]PaC[O.sub.2]) was significantly higher (p < 0.05) during metabolic alkalosis in the chronic hypercapnic COPD group.
Correlation Between the Different Reactivity Parameters
Poor, not significantly different correlations were found between the individual CBV and VI responses to acute hypercapnia ([DELTA]CBV/[DELTA]PaC[O.sub.2] and VI/[DELTA]PaC[O.sub.2]; r [less than or equal to] 0.44, p > 0.1) for both COPD patients (Fig 3) under control condition and during metabolic acidosis; a weak but significant correlation was found during metabolic alkalosis in both COPD groups (r = 0.58; p < 0.05). Correlations between the individual CBV and [P.sub.0.1] slopes ([DELTA]CBV/[DELTA]PaC[O.sub.2] and [DELTA][P.sub.0.1]/[DELTA]PaC[O.sub.2]) were poor and not significant in both COPD groups in three metabolic conditions (Fig 4).
[FIGURES 3-4 OMITTED]
DISCUSSION
Cerebrovascular responses were studied and correlated with ventilatory reactivity in normocapnic and chronic hypercapnic COPD patients. Chronic hypercapnic patients showed the same CBV and VI reactivities to short-term carbon dioxide changes under baseline metabolic conditions as did normocapnic patients. [P.sub.0.1] was the same in both COPD groups, even after correction for MIP. The influence of superimposed chronic metabolic acidosis on CBV reactivity, VI reactivity, and [P.sub.0.1] reactivity was not significantly different in both COPD groups. However, effects of superimposed chronic metabolic alkalosis were more pronounced in the normocapnic COPD group, with (tendency to) lower ventilatory and cerebrovascular carbon dioxide responses in the latter group. In addition, [P.sub.0.1] reactivity was significantly increased in the chronic hypercapnic group. Ventilatory and cerebrovascular carbon dioxide responsiveness were correlated and showed a wide interindividual variability of cerebrovascular and ventilatory reactivity to short-term changes in PC[O.sub.2], thus refuting the hypothesis of an inverse relationship between [DELTA]CBV/[DELTA]PaC[O.sub.2] and [DELTA]VI/[DELTA]PaC[O.sub.2] in patients with COPD.
Critique of Methods
Before this study, the reproducibility of CBV measurements during resting conditions using NIRS was evaluated, and an intraindividual coefficient of variation of [+ or -] 10% was found. (18) These results are in agreement with others. (14,15) CBV values of the present study under baseline metabolic conditions in both COPD groups (2.41 [+ or -] 0.66 mL/100 g and 2.90 [+ or -] 0.60 mL/100 g, respectively) are consistent with other investigators using NIRS in healthy subjects (2.85 [+ or -] 0.97 mL/100 g). (14)
It is important to consider the advantages of measurements of CBV over measurements of CBF. First, there is a close relationship (r = 0.9) between CBV and CBF that has been extensively investigated by Grubb et al (19) and by van Zijl et al. (20) Second, the use of CBV instead of CBF eliminates the problems related to the mean cerebral transit time. (21) Finally, near-infrared absorption changes reflect changes in the oxygenation of the microvasculature, and thus the CBV of the brain tissue. (22) Changes of CBV reflect capillary recruitment, which is considered, by some, a better reflection of cerebrovascular responses than CBF responses to acid-base stimuli. (21) We measured CBV in the frontal cortex region because present techniques do not allow measures of CBV or CBF in the brainstem of conscious humans. Moreover, Hida et al (23) could not find any differences in carbon dioxide responses between the brainstem artery and the middle cerebral artery, supporting the assumption that our frontal lobe CBV measurements may be a good reflection of overall CBV changes in the brain.
Baseline Metabolic Control Conditions
Absolute values of CBV were lower in the normocapnic COPD group. Age, (24) hematocrit, (25) MAP, and heart rate (26) are established factors that affect CBV. However, both COPD groups were age matched, and all other parameters were not significantly different. The influence of medication was evaluated to find an explanation for the differences of CBV values between the COPD groups. Theophylline and corticosteroids are known to lower CBV. (27,28) To account for medical intervention, average CBV and VI was recalculated after subdividing both COPD groups in users and nonusers of theophyllines and/or oral corticosteroids. In contrast to others, (27,28) CBV was not significantly different in our group of theophylline users, relative to the nonusers in both COPD groups. In addition, no differences were seen in ventilation. Furthermore, CBV values and VI values measured in corticosteroid users and nonusers were not different. Buchweitz and Weiss (29) described that IV salbutamol (1 [micro]g/kg) leads to an increased CBV in rats. In addition, the influence of inhaled salbutamol is likely to be less important on CBV regulation. An equal number of patients in both COPD groups received inhaled salbutamol. This study did not show any significant effect of inhaled salbutamol in both COPD groups on both CBV and VI.
CBV responsiveness to carbon dioxide was not reduced in the chronic hypercapnic COPD group compared with the normocapnic group. This is probably because of the power of the study. A reduced cerebral vascular responsiveness to a carbon dioxide challenge is in line with the findings of others, (8,9) and is suggested to be the resultant of several factors, including: (1) a reduced increase in tissue hydrogen ion concentration secondary to an increased buffering capacity of the brain substance; (2) changes in the chemical composition of the CSF bathing the cerebral vessels (arterioles), involving an adjustment in the concentration of bicarbonate ions (8); (3) changes in neurotransmitter production secondary to chronic hypercapnia; (4) a chronic increase in interstitial fluid; (5) increased venous resistance to venous return; and (6) an inability to increase cardiac output.
Ventilatory responsiveness to carbon dioxide administration was highest in normocapnic COPD patients compared with chronic hypercapnic COPD patients. This result was expected and is in agreement with results of others. (5,10,30,31) Because serum bicarbonate levels are higher in patients with chronic hypercapnia than patients with normocapnia, pH changes at the central chemoreceptor, caused by acute respiratory hypercapnia, are lower for a given increment in PaC[O.sub.2]. This could explain the lower ventilatory responses in the first group. (32) The lack of statistical significance may be explained by the relatively small size of the group.
Similar to the findings of Gelb et al (30) and Montes de Oca and Celli, (10) but in contrast to others, (5,32) the present study found the same values of [P.sub.0.1] responsiveness in the hypercapnic group relative to the normocapnic group. The present study agreed with the results of Scano et al, (5) that even after normalization of [P.sub.0.1] for individual differences in muscle strength was performed ([P.sub.0.1] as percentage of MIP), no differences between both COPD groups were seen.
Effects of Chronic Metabolic Acidosis
Acetazolamide is used in patients with COPD to improve blood gas values, especially in cases with a metabolic alkalosis related to the use of steroids and diuretics. (33) The beneficial effect of acetazolamide in these patients is probably primarily caused by an increase in ventilatory drive, secondary to a metabolic acidosis induced by effective inhibition of renal carbonic anhydrase. (34) A clinical dose of acetazolamide (250 mg po q8h for 3 days) leads to increased ventilation, resulting in a lowered PaC[O.sub.2]. (35) However, in the present study, results of ventilation after acetazolamide administration differed in normocapnic patients relative to chronic hypercapnic patients. This might be caused by the relatively flat carbon dioxide response curve, which is a common observation in the latter group. A change in BE would shift the carbon dioxide response curve leftward, without much measurable change in ventilation and in ventilatory responsiveness ([DELTA]VI/[DELTA]PaC[O.sub.2]). (35) Earlier studies found different effects of acetazolamide administration on the ventilatory carbon dioxide sensitivity in humans, with variations from no change (35,36) to an increase (37) after long-term application. It is suggested that differences in drug regimens and methodology to determine slopes of carbon dioxide responses curves (eg, steady-state methods vs rebreathing) may account for these variable study outcomes. (35)
The increase in ventilation caused a rise in Pa[O.sub.2] in the normocapnic group. The presence of many lung regions with low ventilation/perfusion ratios may have mainly contributed to the lack of increase of ventilation and increase of Pa[O.sub.2] in the chronic hypercapnic group. (35) However, the degree of ventilation-perfusion mismatch was only slightly higher in the latter group.
Because of its physical/chemical properties, acetazolamide does not easily cross the blood brain barrier, (38) even at higher doses. However, even after one low dose of acetazolamide (4 mg/kg), a decrease of carbon dioxide sensitivity of the central chemoreflex loop was found in carotid body denervated cats, which the investigators (39) thought to be an altered relationship between brain blood flow and brain tissue PC[O.sub.2]. However, the present study could not support differences in cerebrovascular reactivity and, thus, altered relationships between cerebral blood volume and PaC[O.sub.2] after long-term acetazolamide administration in both COPD groups.
Effect of Chronic Metabolic Alkalosis
It is interesting to note the different effects of furosemide administration in both COPD groups, with reduced effects on [DELTA]BE in the hypercapnic COPD group. This may be caused by the preexisting metabolic compensated alkalosis in the latter group, relative to the normocapnic group (mean control value of BE, 2.4 mEq/L vs 0.8 mEq/L) and, therefore, difficulties to induce a further metabolic alkalosis. Ventilatory and cerebrovascular slopes were not different in the normocapnic group after the induction of metabolic alkalosis. Values of PaC[O.sub.2] (despite unchanged ventilation) are only significantly elevated in the normocapnic group. Despite minor BE changes, Pa[O.sub.2] deteriorated significantly in the chronic hypercapnic group. The higher [P.sub.0.1] slope with a concomitant unchanged ventilation slope in chronic hypercapnic COPD patients is probably caused by an ensuing increased airway resistance as seen during alkalosis. (40)
Mean values of CBV did not alter during metabolic alkalosis. Earlier studies (41) suggest lower cerebral blood flows during maintained steady chronic metabolic alkalosis in healthy humans. Assuming similarities in CBF between healthy subjects and normocapnic patients with COPD, the present study suggest only a tendency to a lower CBV reactivity in normocapnic patients with COPD.
Correlation Between the Different Reactivity Parameters
Other investigators pointed out the importance of measuring ventilation and cerebrovascular reactivity simultaneously. (34,42) The present study showed a wide variety in ventilatory and cerebrovascular carbon dioxide responsiveness, albeit showing some positive correlation and thereby refuting the hypothesized inverse relationship.
In conclusion, chronic hypercapnic patients showed the same CBV and VI reactivities under baseline metabolic conditions compared with patients with normocapnia. The effect of superimposed chronic metabolic acidosis on mean CBV reactivity and VI reactivity was not significantly different in both COPD groups. However, different effects on arterial blood gas values were seen between the COPD groups. In addition, superimposed chronic metabolic alkalosis was more obvious in the normocapnic COPD group and led to some tendency to lower ventilatory and cerebrovascular carbon dioxide responses in the latter group. [P.sub.0.1] was similar in both COPD groups, even after correction for MIP during control condition and metabolic acidosis. The increased [P.sub.0.1] reactivity during superimposed chronic metabolic alkalosis in the chronic hypercapnic group was probably caused by increased airway resistance. The poor, but positive correlation between ventilatory and cerebrovascular carbon dioxide responsiveness ([DELTA]CBV/[DELTA]PaC[O.sub.2] and [DELTA]VI/[DELTA]PaC[O.sub.2]) during all metabolic conditions argued against our hypothesis concerning an inverse relationship between cerebrovascular and ventilatory responses to PaC[O.sub.2], and differences in neuroventilatory reactivity between normocapnic and hypercapnic COPD groups.
ACKNOWLEDGMENT: We thank Mrs. B. T. P. Kersten and Mrs. G. Pletting for their assistance during the experiments.
APPENDIX
We describe a simple linearized static model of the interaction between CBF and ventilation (V) in response to changes in PaC[O.sub.2]. Consider a certain volume of brain tissue with a metabolic rate of M (liters [standard temperature and pressure, dry] of carbon dioxide per minute) and perfused by Q (liters per minute) of blood entering the tissue with a PaC[O.sub.2].
According to Fick's law, the venous partial carbon dioxide pressure (PVC[O.sub.2]) in steady state then is,
(1) PVC[O.sub.2] = PaC[O.sub.2] + M/(c x Q)
where c is solubility.
For reasons of simplicity, the index carbon dioxide will now be dropped. We now make the simplifying assumption that during normoxia, perfusion around the operating point is linearly dependent on arterial pressure (Pa); therefore,
(2) Q = [Q.sub.0] + a x Pa
Next, we assume that the normoxic central ventilatory drive is a simple linear combination of arterial pressure and venous pressure (Pv),
(3) V = [V.sub.0]+ [alpha] x Pa+ [beta] x Pv
Substituting equations 1 and 2 in equation 3 yields,
(4) V = [V.sub.0] + ([alpha] + [beta]) x Pa + [beta]M/(c[[Q.sub.0] + (a x Pa)])
Equation 4 consists of three terms. Because the ventilatory drive V = 0 at some non-zero, positive value of arterial pressure, term 1 must be a negative constant. Term 2 increases linearly with arterial pressure. Term 3 represents the larger part of the interaction between CBF and ventilatory drive and has an inverse response ([DELTA]V/[DELTA]Pa < 0). It decreases with increasing arterial pressure, thus damping the ventilatory response to an increase in arterial pressure. At lower arterial pressure values, this term is the more important one, increasing with decreasing values of arterial pressure. Depending on the balance of terms 2 and 3, term 3 may even induce hyperventilation. The blunted response of patients with COPD can be modeled here with relative small values for [alpha] and [beta] in equation 3, making term 3 more important.
REFERENCES
(1) Steinbrook RA, Javaheri S, Gabel RA, et al, Respiration of chemodenervated goats in acute metabolic acidosis. Respir Physiol 1984; 56:51-60
(2) Tuteur P, Reivich M, Goldberg HI, et al. Transient responses of cerebral blood flow and ventilation to changes in PaC[O.sub.2] in normal subjects and patients with cerebrovascular disease. Stroke 1976; 7:584-590
(3) Poulin MJ, Robbins PA. Influence of cerebral blood flow on the ventilatory response to hypoxia in humans. Exp Physiol 1998; 83:95-106
(4) Teppema L, Berkenbosch A, DeGoede J, et al. Carbonic anhydrase and control of breathing: different effects of benzolamide and methazolamide in the anaesthetized cat. J Physiol 1995; 488:767-777
(5) Scano G, Spinelli A, Duranti R, et al. Carbon dioxide responsiveness in COPD patients with and without chronic hypercapnia. Eur Respir J 1995; 8:78-85
(6) Neubauer JA, Melton JE, Edelman NH. Modulation of respiration during brain hypoxia. J Appl Physiol 1990; 68:441-451
(7) Feihl F, Perret C. Permissive hypercapnia. How permissive should we be? Am J Respir Crit Care Med 1994; 150:1722-1737
(8) Levasseur JE, Wei EP, Kontos HA, et al. Responses of pial arterioles after prolonged hypercapnia and hypoxia in the awake rabbit. J Appl Physiol 1979; 46:89-95
(9) Clivati A, Ciofetti M, Cavestri R, et al. Cerebral vascular responsiveness in chronic hypercapnia. Chest 1992; 102:135-138
(10) Montes de Oca M, Celli BR. Mouth occlusion pressure, C[O.sub.2] response and hypercapnia in severe chronic obstructive pulmonary disease. Eur Respir J 1998; 12:666-671
(11) Jobsis FF. Noninvasive, infrared monitoring of cerebral and myocardial oxygen sufficiency and circulatory parameters. Science 1977; 198:1264-1267
(12) Delpy DT, Cope M. Quantitation in tissue near-infrared spectroscopy. Philos Trans R Soc Lond B Biol Sci 1997; 261:649-659
(13) Harris DN, Cowans FM, Wertheim DA, et al. NIRS in adults: effects of increasing optode separation. Adv Exp Med Biol 1994; 345:837-840
(14) Elwell CE, Cope M, Edwards AD, et al. Quantification of adult cerebral hemodynamics by near-infrared spectroscopy. J Appl Physiol 1994; 77:2753-2760
(15) Wyatt JS, Cope M, Delpy DT, et al. Quantitation of cerebral blood volume in human infants by near-infrared spectroscopy. J Appl Physiol 1990; 68:1086-1091
(16) Whitelaw WA, Derenne JP, Milic-Emili J. Occlusion pressure as a measure of respiratory center output in conscious man. Respir Physiol 1975; 23:181-199
(17) Gorini M, Spinelli A, Ginanni R, et al. Neural respiratory drive and neuromuscular coupling in patients with chronic obstructive pulmonary disease (COPD). Chest 1990; 98: 1179-1186
(18) Van de Ven MJ, Colier WN, van der Sluijs MC, et al. Can cerebral blood volume be measured reproducibly with an improved near infrared spectroscopy system? J Cereb Blood Flow Metab 2001; 21:110-113
(19) Grubb RL, Raichle ME, Eichling JO, et al. The effects of changes in PaC[O.sub.2] on cerebral blood volume, blood flow, and vascular mean transit time. Stroke 1974; 5:630-639
(20) van Zijl PC, Eleff SM, Ulatowski JA, et al. Quantitative assessment of blood flow, blood volume and blood oxygenation effects in functional magnetic resonance imaging. Nat Med 1998; 4:159-167
(21) Shockley RP, LaManna JC. Determination of rat cerebral cortical blood volume changes by capillary mean transit time analysis during hypoxia, hypercapnia and hyperventilation. Brain Res 1988; 454:170-178
(22) Mancini DM, Bolinger L, Li H, et al. Validation of near-infrared spectroscopy in humans. J Appl Physiol 1994; 77: 2740-2747
(23) Hida W, Kikuchi Y, Okabe S, et al. C[O.sub.2] response for the brain stem artery blood flow velocity in man. Respir Physiol 1996; 104:71-75
(24) Dorfler P, Puls I, Schliesser M, et al. Measurement of cerebral blood flow volume by extracranial sonography. J Cereb Blood Flow Metab 2000; 20:269-271
(25) York EL, Jones RL, Menon D, et al. Effects of secondary polycythemia on cerebral blood flow in chronic obstructive pulmonary disease. Am Rev Respir Dis 1980; 121:813-818
(26) MacKenzie ET, McGeorge AP, Graham DI, et al. Effects of increasing arterial pressure on cerebral blood flow in the baboon: influence of the sympathetic nervous system. Pflugers Arch 1979; 378:189-195
(27) Nishimura M, Yoshioka A, Yamamoto M, et al. Effect of theophylline on brain tissue oxygenation during normoxia and hypoxia in humans. J Appl Physiol 1993; 74:2724-2728
(28) Schraa JC, Dirks JF. The influence of corticosteroids and theophylline on cerebral function: a review. Chest 1982; 82:181-185
(29) Buchweitz ME, Weiss HR. Effect of salbutamol on regional cerebral oxygen consumption, flow and capillary and arteriolar perfusion. Neurol Res 1990; 12:169-175
(30) Gelb AF, Klein E, Schiffman P, et al. Ventilatory response and drive in acute and chronic obstructive pulmonary disease. Am Rev Respir Dis 1977; 116:9-16
(31) Fahey PJ, Hyde RW. "Won't breathe" vs "can't breathe". Detection of depressed ventilatory drive in patients with obstructive pulmonary disease. Chest 1983; 84:19-25
(32) Altose MD, McCauley WC, Kelsen SG, et al. Effects of hypercapnia and inspiratory flow-resistive loading on respiratory activity in chronic airways obstruction. J Clin Invest 1977; 59:500-507
(33) Vos PJ, Folgering HT, de Boo TM, et al. Effects of chlormadinone acetate, acetazolamide and oxygen on awake and asleep gas exchange in patients with chronic obstructive pulmonary disease (COPD). Eur Respir J 1994; 7:850-855
(34) Swenson ER. Carbonic anhydrase inhibitors and ventilation: a complex interplay of stimulation and suppression. Eur Respir J 1998; 12:1242-1247
(35) Teppema LJ, Dahan A. Acetazolamide and breathing: does a clinical dose alter peripheral and central C[O.sub.2] sensitivity? Am J Respir Crit Care Med 1999; 160:1592-1597
(36) Lerche D, Katsaros B, Lerche G, et al. Vergleich der Wirkung verschiedener Acidosen (N[H.sub.4[Cl, Ca[Cl.sub.2], Acetazolamid) auf die Lungenbeluftung beim Menschen. Pflugers Arch 1960; 270:450-460
(37) Tojima H, Kunitomo F, Okita S, et al. Difference in the effects of acetazolamide and ammonium chloride acidosis on ventilatory responses to C[O.sub.2] and hypoxia in humans. Jpn j Physiol 1986; 36:511-521
(38) March TH. Carbonic anhydrase: chemistry, physiology and inhibition. Physiol Rev 1967; 47:595-781
(39) Wagenaar M, Teppema L, Berkenbosch A, et al. The effect of low-dose acetazolamide on the ventilatory C[O.sub.2] response curve in the anaesthetized cat. J Physiol 1996; 495:227-237
(40) Brijker F, van den Elshout FJ, Heijdra YF, et al. Effect of acute metabolic acid/base shifts on the human airway calibre. Respir Physiol 2001; 124:151-158
(41) Fencl V, Vale JR, Broch JA. Respiration and cerebral blood flow in metabolic acidosis and alkalosis in humans. J Appl Physiol 1969; 27:67-76
(42) Berkenbosch A, de Goede J, Olievier CN, et al. Influence of the CSF bicarbonate concentration on the ventilatory response to C[O.sub.2] in relation to the location of the central chemoreceptors. Respir Physiol 1978; 35:215-236
* From the Department of Pulmonology Dekkerswald (Drs. van de Ven and Folgering) and the Department of Physiology (Drs. Colier, Oeseburg, and Vis and Mr. van der Sluijs), Faculty of Medical Sciences, University Medical Center Nijmegen, The Netherlands.
This study was supported by the Dutch Asthma Foundation (96.09).
Manuscript received March 7, 2001; revision accepted August 6, 2001.
Correspondence to: Marjo J. T. van de Ven, MD, Department of Pulmonology Dekkerswald, University Medical Center Nijmegen, PO Box 9001, 6560 GB Groesbeek, The Netherlands; e-mail: m_vandeven60@hotmail.com
COPYRIGHT 2002 American College of Chest Physicians
COPYRIGHT 2002 Gale Group