PROBLEM STATEMENT
Gamma-hydroxybutyrate (GHB), an increasingly popular drug to abuse (1-3), is unfamiliar to many psychiatric professionals. Recent cases of severe GHB withdrawal delirium have occurred in psychiatric settings, making it necessary for psychiatric professionals to be informed about the management of these patients (4,5).
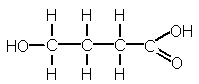
GHB, a naturally occurring metabolite of gamma-aminobutyric acid (GABA) (6), is an inhibitory neurotransmitter that mediates sleep cycles, cerebral metabolism, memory and emotional control (7). Synthetic GHB, originally used by body builders for its putative anabolic effects, has more recently been abused for its sedative, euphoriant and aphrodisiac effects and as a "rave" and "date rape" drug (8).
GHB was previously available in health food stores and gyms, and it was marketed for its purported muscle building and fat burning effects. In 1990, the Food and Drug Administration (FDA) banned the manufacture and distribution of GHB after receiving several reports of abuse leading to coma and seizures (4,6,9). Precursor compounds such as gamma-butyrolactone (GBL) and 1,4-butanediol (BD), which can be converted by the body or simple chemical processing into GHB, remained available over the Internet (5,6,10-12). GHB is easily manufactured by illicit laboratories or by "home brew" recipes that have been published in books and on the Internet (5,13). Despite the FDA's attempts to control distribution of these compounds, they remain widely available to body builders and to drug abusers (2). For the purpose of this paper, the abbreviation GHB will be used to refer to both GHB and its related precursors.
Although acute effects of GHB overdose have led to coma, seizure, respiratory arrest, and death (7), withdrawal syndromes from chronic GHB abuse were initially reported to be mild and without complications or sequelae (14). More recently, several cases of severe GHB withdrawal delirium that necessitated management in intensive care unit settings have been reported (5,15-17). The reasons for the increasing severity of GHB withdrawal are not known; however, one explanation could be that the use of precursors such as GBL and BD have become more popular since GHB was banned by the FDA. In comparison to GHB, GBL is more rapidly absorbed, reaches higher concentrations, and has a more prolonged duration of action (2). When combined with alcohol, BD demonstrates prolonged toxicity resulting from competition for alcohol dehydrogenase, which is involved in the metabolism of both these compounds (2). Alcohol is frequently used by GHB abusers in an attempt to detoxify themselves from GHB; in the case of BD, alcohol may actually exacerbate and extend BD's toxic effects (2).
Because the initial symptoms of GHB withdrawal delirium are often auditory and visual hallucinations, disorientation, and severe agitation, these symptoms may be presumed to be psychiatric in nature, and the patient may be transferred to a psychiatric unit (5,18). Although milder cases have been managed in this setting, more severely dependent cases may be at risk of physical decompensation and death if not transferred to a critical care setting. In this article, we will describe two patients in severe GHB withdrawal who were transferred to the inpatient psychiatric unit in our facility. Suggestion will be made for assessment, monitoring, and management of patients at risk of developing this severe GHB withdrawal delirium syndrome.
CASE #1
Mr. R., a 39-year-old male with no prior psychiatric history, was brought to the emergency department by the police for "bizarre behavior" at a local shopping mall, where he had attacked a couple walking by him. Now, in the emergency department, he was floridly psychotic and obviously experiencing terrifying multisensory hallucinations. His wife noted that he "hadn't slept in a week" and had been behaving strangely. She reported his escalating GHB use and his inability to cut down without experiencing tremors and diaphoresis. It was later learned that he had been dosing at least a "capful" of GHB every 90 minutes around the clock for many months.
Mr. R. was a retired body builder with a long history of polysubstance abuse that included alcohol, opioids, cocaine, and anabolic steroids. His urine drug screen was positive only for the opioids he used (and abused) for chronic back pain. Mr. R. currently worked as a salesman in an herbal supplement store, which provided him with access to GHB-related compounds. It was while working there that he had begun to use GHB, first for weight training, then for euphoria, and finally in a desperate attempt to avoid withdrawal.
Mr. R.'s hospital course was tumultuous. He went from the emergency department to the telemetry unit for observation. Delirious, he spent 5 days in four-point restraints. Initially the internal medicine service attempted to manage his increasing agitation with intramuscular (IM) haloperidol and fluphenazine, but this did little more than produce a dystonic reaction. As his temperature reached 103.5[degrees]F, neuroleptic malignant syndrome (NMS) became a concern and neuroleptic agents were discontinued. NMS was later ruled out. Because of his extreme level of agitation, increasing doses of phenobarbital and lorazepam were required.
On day 6, Mr. R. was considered "medically stable" and he was transferred to the inpatient psychiatric unit. At that time his Folstein Mini-Mental State Examination (MMSE) (19) score was 12/30. However, the next morning he was so disoriented that a repeat MMSE could not be performed. At this point his creatine phosphokinase level had increased to 3,317 and he was returned to the telemetry unit out of concern for potential rhabdomyolysis and renal failure. He spent another week in telemetry receiving high doses of intravenous (IV) lorazepam (up to 8 mg/hr) and phenobarbital (up to 150 mg IV twice a day) for severe agitation. During this time he developed pneumonia and diffuse ST interval changes on his electrocardiogram (ECG), and most medical subspecialties were involved in his care.
After Mr. R. was medically stable, he was returned to the inpatient psychiatric unit. As his mental status improved and his agitation decreased, the lorazepam and phenobarbital and were tapered. On day 18, he was discharged with a prescription for a tapering dose of lorazepam. During his stay he had received in total: 214mg of lorazepam, 2025 mg of phenobarbital, 94mg of fluphenazine, 109 mg of haloperidol, and 45 mg of risperidone. Mr. R. had little recall of his delirium, and at the time of discharge he had no insight into his need for drug rehabilitation. He insisted that this "incident" was due to head trauma sustained in a motor vehicle accident a year earlier rather than to this GHB use.
CASE #2
Mr. D., a 40-year-old white male with no previous psychiatric history, was brought to the emergency department by his girlfriend for his increasing disorganization, memory deficits, paranoid delusions, and multisensory hallucinations. He told staff that he was "desperate to get off the GHB." He had attempted to do so on his own, but had experienced severe withdrawal symptoms within 2hours of his last dose. This was not his first GHB detoxification. Sixteen months earlier he had spent a week in another hospital for GHB withdrawal. This time he had surpassed his previous level of usage. He later estimated that he had been using 50-75 mg of GHB per day, which he dosed at 30- to 90-minute intervals around the clock. Mr. D. was a competitive body builder with an extensive history of polysubstance abuse that included alcohol, cocaine, OxyContin (sustained-release oxycodone), and alprazolam. His current urine drug screen was positive for benzodiazepines and opioids. Although initially admitted to the inpatient detoxification unit, he was transferred to the inpatient psychiatric unit for increasing psychosis and agitation. There he was treated with clonidine for opioid withdrawal and lorazepam for agitation. Because the patient remained extremely psychotic and agitated, IM haloperidol was administered, but this produced a dystonic torticollis. His delirium worsened overnight, and the next morning he was transferred to the intensive care unit, where he was intubated, placed on mechanical ventilation, and sedated with lorazepam, 15 mg/hour IV drip; phenobarbital, 250mg via nasogastric tube every 12hours; and propofol, 50 [micro]g/kg/hr IV drip. As his creatine phosphokinase level reached 28,140, the decision was made to paralyze him with a Norcuron (vecuronium bromide) drip. He remained paralyzed for 3 days, during which time he developed a right lower lobe pneumonia and became uroseptic. On day 16 serial ECGs showed inferior wall ischemia, and an echodoppler confirmed inferior wall hypokinesis.
Medically stabilized, Mr. D. returned to the inpatient psychiatric unit where his lorazepam was discontinued and clonazepam, 3 mg every 2 hours, was started. By the time his delirium had resolved, he had spent 14 days in restraints. On day 17 he was discharged with a prescription for a gradual clonazepam taper. During the course of his stay he had received propofol, Norcuron, 36 mg of haloperidol, 174 mg of lorazepam, 213 mg of clonazepam, and 4920 mg of phenobarbital. When Mr. D.'s mental status cleared, he believed the date to be 1 day after he had been admitted; he could not remember the past 2 weeks. The cost of his hospital stay, without doctors' fees, exceeded $60,000, and he was uninsured.
DISCUSSION
Although there have been multiple reports of intoxication and overdose from GHB and its related precursors (3,7,14), until recently withdrawal syndromes from these compounds have been reported as mild and without sequelae (14). In 1997, Galloway et al. (14) published a case series of several patients who experienced withdrawal syndrome after abrupt discontinuation of GHB. Symptoms reported included insomnia, anxiety, and tremors. The authors suggested that sedatives be used only for more severe symptoms, should they arise, and that patients should be reassured of the absence of dangerous withdrawal symptoms.
Since this initial report of GHB-related physical dependence in 1997, there have been several reports of much more severe withdrawal syndromes, including cases of severe delirium which required management in intensive care settings (15-17). Many of these patients were initially referred to psychiatric settings because of the emergence of psychotic symptoms including hallucinations, delirium, paranoia, disorientation, and severe agitation (4,5). In most cases patients did not respond to the usual doses of antipsychotics and sedative agents. They were subsequently transferred to intensive care units to treat the potentially life-threatening complications of withdrawal including increased creatine phosphokinase and the emerging risk of renal failure (16). The cases in this article are among the most severe reported. These patients suffered severe medical complications and required large doses of sedatives to calm their agitation and to prevent further medical complications.
A common feature of all reported cases of severe GHB related withdrawal delirium has been abrupt discontinuation of GHB after habitual use every 1 to 4hours around the clock (16,17). The severity of the delirium has been related more to frequency of use than to duration of use (17). The duration of use necessary for physical dependence is unknown but may be 2 months or less (16). Daily dosage necessary to produce this severe abstinence delirium is also unknown, but in the reported cases patients used 1 to 5 teaspoons (approximately 2.5 g per teaspoon) every one to four hours (15-17).
Accumulating evidence, including the cases in this report, suggests that withdrawal from GHB can in severe cases be life-threatening. All cases of GHB withdrawal delirium should be considered medical emergencies and should be managed in critical care settings rather than psychiatric settings. It is not uncommon for patients with acute mental status changes secondary to delirium to be transferred to psychiatric units because of the emergence of hallucinations, delusions, or agitation. By definition, delirium is a medical (not psychiatric) disorder (20) that requires close monitoring and aggressive treatment to prevent life-threatening sequelae.
In both of our cases, as well as several cases reported in the literature (5,18), patients were either inappropriately admitted to or subsequently transferred to psychiatric units during the course of severe GHB-related withdrawal delirium. This put these patients at risk of morbidity or mortality related to this critical condition. In one previously reported case (16), a 24-year-old patient died from cardiac arrhythmias on the thirteenth day of GHB withdrawal despite close medical monitoring and aggressive treatment with sedative agents. In this case the patient's condition appeared to be improving but he continued to exhibit symptoms of delirium.
In our case #2, the patient was transferred back to psychiatry as his medical condition "stabilized"; however, he remained delirious and agitated and he required four-point restraints. Fortunately, high doses of oral clonazepam were effective in calming his agitation while the delirium resolved. However, this patient was still at an increased risk of morbidity or mortality because his delirium had not fully resolved at the time of transfer to psychiatry. In fact, the patient showed significant ischemic ECG changes as late as the sixteenth day of withdrawal, 3 days after his transfer back to psychiatry.
It should be noted that, in both of our cases, the patients were abusing other substances in addition to GHB. In case #1, the patient was abusing opioid analgesics; in case #2, the patient was abusing both opioids and benzodiazepines. Some of the symptoms in both of the cases could have been due to opioid withdrawal; however, severe withdrawal deliriums of this magnitude have not been associated with opioid withdrawal. And, in case #2, the patient received benzodiazepines to treat his withdrawal syndrome; therefore, benzodiazepine withdrawal syndrome can be ruled out.
Time Course of GHB Withdrawal Delirium
Early symptoms of withdrawal occur within 1 to 6 hours after the last dose and include anxiety, restlessness, insomnia, tremors, tachycardia, hypertension, nausea, vomiting, and diaphoresis (17). Progressive symptoms occur between day 1 and day 6 and include increasing severity of the early symptoms, as well as confusion; delirium; auditory, visual and tactile hallucinations; and extreme agitation (17). Patients typically need large doses of sedative hypnotic drugs and four-point restraints during this stage (17). Symptoms usually begin to wane between days 7 and 14 (17); however, as in our cases, acute symptoms may continue for more than 2 weeks.
Recommendations for Management
1. GHB should be suspected in cases of coma, seizures, or withdrawal when no other etiology can be found; urine drug screen is negative for other drugs; and demographic factors point toward this type of substance abuse. These demographic factors include adolescents and young adults with a history of drug abuse, and body builders. Although GHB is detectable in plasma and urine, these assays are usually impractical because levels can only be detected for up to 12hours after last use, few medical labs are equipped to do these assays, and they are costly.
2. If GHB is known or suspected to be involved in overdose or withdrawal, patients should be monitored in an emergency department or critical care unit setting until symptoms resolve or delirium clears. Management includes tapering doses of sedative drugs as indicated and use of restraints as long as severe agitation persists. Patients should remain in a monitored setting until delirium resolves, because ECG changes and at least one death (16) have occurred.
3. Sedative-hypnotic drugs should be continued and gradually tapered over several weeks after the resolution of acute withdrawal. Long-acting agents such as clonazepam or phenobarbital may be preferable during this stage to decrease the likelihood of interdose symptoms of a prolonged withdrawal syndrome.
4. If the condition progresses to severe delirium and agitation, high-dose IV benzodiazepines, phenobarbital, general anesthetics, or neuromuscular blocking agents should be used in an attempt to minimize the medical complications associated with this severe withdrawal syndrome.
5. Neuroleptic agents have been generally ineffective in treating psychosis and agitation and they may predispose the patients to additional complications such as dystonic reactions (5,16). Dystonias occurred in both our patients when treated with neuroleptics.
6. Most patients are unable to remember the experience of severe GHB withdrawal (7) related to their delirious state and the amnesia-inducing effects of both GHB and the drugs used to treat the withdrawal. Patients may be at increased risk of relapse because they cannot remember the aversive experience of withdrawal. Also, cases of severe depression with suicidal ideation have been reported after detoxification (21). For these reasons intensive substance abuse rehabilitation and psychiatric follow-up are critical after detoxification from GHB.
Psychiatric, emergency, and critical care professionals need to be aware of the signs of GHB withdrawal and should coordinate their care to provide safe management of these patients. Cases of delirium should be treated in critical care settings to avoid potential morbidity or mortality. Further studies are needed to determine the most effective treatment for this syndrome.
ACKNOWLEDGMENT
The authors would like to thank Catherine Locke Rosenberg, BA, for her invaluable assistance in the preparation of this manuscript.
REFERENCES
(1.) Miglani JS, Kim KY, Chahil R. Gamma-hydroxy butyrate withdrawal delirium: a case report. Gen Hosp Psychiatry 2000; 22(3):213-215.
(2.) Shannon M, Quang LS. Gamma-hydroxybutyrate, gamma-butyrolactone, and 1,4-butanediol: a case report and review of the literature. Pediatr Emerg Care 2000; 16(6):435-440.
(3.) Kam PCA, Yoong FFY. Gamma-hydroxybutyric acid: an emerging recreational drug. Anaesthesia 1998; 53(12): 1195-1198.
(4.) Hernandez M, McDaniel CH, Costanza CD, Hernandez OJ. GHB-induced delirium: a case report and review of the literature on gamma hydroxybutyric acid. Am J Drug Alcohol Abuse 1998; 24(1):179-183.
(5.) Catalano MC, Glass JM, Catalano G, Burrows SL, Lynn WA, Weitzner BS. Gamma butyrolactone (GBL) withdrawal syndromes. Psychosomatics 2001; 42(1):83-88.
(6.) Bowles TM, Sommi RW, Amiri M. Successful management of prolonged gamma-hydroxybutyrate and alcohol withdrawal. Pharmacotherapy 2001; 21(2):254-257.
(7.) Doyon S. The many faces of ecstasy. Curr Opin Pediatr 2001; 13(6):170-176.
(8.) GHB: its use and misuse. Harvard Mental Health Lett 2001; 17(9):7-8.
(9.) Schneir AB, Ly BT, Clark RF. A case of withdrawal from the GHB precursors gamma-butyrolactone and 1,4-butanediol. J Emerg Med 2001; 21(1):31-33.
(10.) Chin RL. A case of severe withdrawal from gamma-hydroxybutyrate. Ann Emerg Med 2001; 37(5):561-562.
(11.) Leshner AI. A club drug alert, http://165.112.78.61/NIDA_Notes/ NNVo114N6/DirRepVo114N6.html (accessed November 2001).
(12.) Sanguineti VR, Angelo A, Frank MR. GHB: a home brew. Am J Drug Alcohol Abuse 1997; 23(4):637-642.
(13.) Li J, Stokes SA, Woeckener A. A tale of novel intoxication: a review of the effects of gamma-hydroxybutyric acid with recommendations for management. Ann Emerg Med 1998; 31(6):729-736.
(14.) Galloway GP, Frederick SL, Staggers FE Jr, Gonzales M, Stalcup SA, Smith DE. Gamma-hydroxybutyrate: an emerging drug of abuse that causes physical dependence. Addiction 1997; 92(1): 89-96.
(15.) Craig K, Gomez HF, McManus JL, Bania TC. Severe gamma-hydroxybutyrate withdrawal: a case report and literature review. J Emerg Med 2000; 18(1):65-70.
(16.) Dyer JE, Roth B, Hyma BA. Gamma-hydroxybutyrate withdrawal syndrome. Ann Emerg Med 2001; 37(2):147-153.
(17.) Miotto K, Roth B. Gamma hydroxybutyrate detoxification. www.projectghb.org (accessed November 2001).
(18.) Hutto B, Fairchild A, Bright R. Gamma-hydroxybutyrate withdrawal and chloral hydrate. Am J Psychiatry 2000; 157(10): 1706.
(19.) Folstein MF, Folstein S, McHugh PR. Mini-mental state: a practical method for grading the cognitive state of patients for the clinician. J Psychiatry Res 1975; 12(3):189.
(20.) Kaplan HI, Sadock BJ. Synopsis of Psychiatry: Behavioral Sciences/Clinical Psychiatry. 8th ed. Philadelphia: Lippincott, Williams and Wilkins, 1998.
(21.) Porrata TD. GHB and its analogs: the hidden curse of addiction, http:// www.projectghb.org/addiction/rpt062400.htm (accessed November 2001).
Mark H. Rosenberg, M.S.N., R.N., C.S., * Laurie J. Deerfield, D.O., Psy.D., and Edward M. Baruch, M.D.
Department of Psychiatry, School of Osteopathic Medicine, University of Medicine and Dentistry of New Jersey, Cherry Hill, New Jersey, USA
* Correspondence: Mark H. Rosenberg, University of Medicine and Dentistry of New Jersey, School of Osteopathic Medicine, Department of Psychiatry, 2250 Chapel Avenue West, Suite 100, Cherry Hill, NJ 08002-2000, USA; Fax: 856-482-1159; E-mail: markrosenberg@bigfoot.com.
COPYRIGHT 2003 Marcel Dekker, Inc.
COPYRIGHT 2003 Gale Group