INTRODUCTION: Follicular dendritic cell (FDC) tumor is a rare neoplasm displaying immunophenotypic and morphological features of follicular dendritic cells (1). Approximately 70 cases of FDC tumors have been reported usually in young adults with a 16% morality rate. FDC tumors occur mainly in lymph nodes but also in extranodal locations such as the oral cavity and tonsils, soft palate, hypopharynx, and in the gastrointestinal tract and liver. FDC tumors are often mistaken for other neoplasms. To our knowledge, we report the first case of FDC tumor involving the paratracheal region causing airway obstruction and management dilemmas in the ICU.
CASE PRESENTATION: A previously healthy 29-year-old woman presented to an outside hospital with a month-long progression of neck swelling and dyspnea. The dyspnea rapidly progressed to stridor necessitating orotracheal intubation. CT confirmed a large, lobulated subglottic mass (5.1 x 6.0 cm), replacing the right posterolateral wall of the trachea. There was intraluminal airway involvement and encasement of the right proximal common carotid artery by tumor. Biopsy of the mass revealed a FDC tumor. She was transferred on mechanical ventilation (MV) to our ICU. On ICU day 6, three expandable covered metal stents (in tandem) were placed in the trachea extending 1 cm from the subglottic region to 2 cm above the carina (Figure 1, arrow 1 shows mass, arrow 2, stent). Postoperatively, she was jet ventilated through a 14-French catheter inserted into me proximal tracheal stent. Because of worsening respiratory failure and retained secretions, she was intubated with a 7.5 mm endotracheal tube on ICU day 8. Subsequently, cancer therapy was implemented with 5 weekly cycles of Gemcitabine and external beam radiotherapy. Follow-up CT on ICU day 20 showed significant decrease in the size of the tumor. Improved access to the trachea allowed for tracheostomy on ICU day 22. Post-tracheostomy, the stent intermittently migrated into the right mainstem bronchus with resultant collapse of the left lung. Frequent bronchoscopies (14) were necessary for stent repositioning and pulmonary toilet. The patient was subsequently., liberated from MV. On ICU day 42, the stents were extracted uneventfully. On ICU day 45, she was discharged to the ward for physical therapy and ongoing chemoradiation. On hospital day 49, she was decannulated. Follow-up neck CT revealed near-complete resolution of the tumor. The patient was discharged home and is completing chemotherapy.
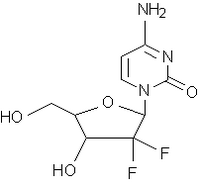
DISCUSSIONS: This case demonstrates several unique challenges in the diagnosis and management of a rare paratracheal FDC tumor. Biopsy of the tumor demonstrates a pleomorphic population of large oval to spindle-shaped tumor cells against a background of small mature lymphocytes and plasma cells (Figure 2a). Diagnosis is confirmed by immunohistochemistry staining for CD21 and/or CD35 antibodies (Figure 2b) and for clusterin. Poor prognostic factors include tumor size > 6 cm, nuclear pleomorphism,necrosis, high mitotic rate, intra-abdominal location and lack of efficacious adjuvant therapy. Complete surgical resection i's the treatment of choice. Neoadjuvant therapy with radiation and chemotherapy is recommended for tumors with poor prognostic factors and for incomplete excision. Our patient was not a surgical candidate because of tumor size and extent; thus, she was treated with combined chemoradiation. During her ICU stay, several critical issues were encountered: unstable airway, intubation through the stent, timing of tracheostomy, intrahospital transport, stent migration, excessive secretions, lung collapse, and administration of chemotherapy in the ICU.
CONCLUSION: Although rare, FDC tumors involving the paratracheal region may cause life-threatening airway obstruction and unique management issues. Intensive care support combined with primary chemoradiation can result in a favorable outcome.
DISCLOSURE: Ali Hmidi, None.
[FIGURE OMITTED]
REFERENCE:
(1) Chan JK, Fletcher CD, Nayler SJ, Cooper K. Follicular dendritic cell sarcoma: clinicopathologic analysis of 17 cases suggesting a malignant potential higher than currently recognized. Cancer 1997: 79:294-313.
Ali Hmidi MD * Louis Voigt MD Stephen M. Pastores MD Diane L. Carlson MD Neil A. Halpern MD Memorial Sloan-Kettering Cancer Center, New York, NY
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group