Definition
Antimalarial drugs are medicines that prevent or treat malaria.
Purpose
Antimalarial drugs treat or prevent malaria, a disease that occurs in tropical, subtropical, and some temperate regions of the world. The disease is caused by a parasite, Plasmodium, which belongs to a group of one-celled organisms known as protozoa. The only way to get malaria is to be bitten by a certain type of mosquito that has bitten someone who has the disease.Thanks to mosquito control programs, malaria has been eliminated in the United States, almost all of Europe, and large parts of Central and South America. However, mosquito control has not worked well in other parts of the world, and malaria continues to be a major health problem in parts of Africa, Southeast Asia, Latin America, Haiti, the Dominican Republic, and some Pacific Islands. Every year, some 30,000 Americans and Europeans who travel to these areas get malaria. People planning to travel to the tropics are often advised to take antimalarial drugs before, during, and after their trips, to help them avoid getting the disease and bringing it home with them. These drugs kill Plasmodium or prevent its growth.
In recent years, some strains of Plasmodium have become resistant to antimalarial drugs, and medical researchers have stepped up efforts to develop a malaria vaccine. In early1997, researchers reported encouraging results from a small study of one vaccine and planned to test the vaccine in Africa.
Description
Antimalarial drugs are available only with a physician's prescription. They come in tablet, capsule, and injectable forms. Among the commonly used antimalarial drugs are chloroquine (Aralen), mefloquine (Lariam), primaquine, pyrimethamine (Daraprim), and quinine.
Recommended dosage
Recommended dosage depends on the type of antimalarial drug, its strength, and the form in which it is being used (such as tablet or injection). The dosage may also be different for different people. Check with the physician who prescribed the drug or the pharmacist who filled the prescription for the correct dosage. Always take this medicine exactly as directed, and keep taking it for the full time of treatment. If the drug is being taken to treat malaria, do not stop taking it just because symptoms begin to improve. Symptoms may return if the drug is stopped too soon. Never take larger or more frequent doses than the physician has ordered, and do not take the drug for longer than directed.
Travelers taking this medicine to prevent malaria may be told to take it for 1-2 weeks before their trip and for 4 weeks afterward, as well as for the whole time they are away. It is important to follow these directions.
Antimalarial drugs work best when they are taken on a regular schedule. When taken once a week to prevent malaria, they should be taken on the same day every week. When taken daily or several times a day to treat malaria, they should be taken at the same time every day. Doses should not be missed or skipped.
Some antimalarial drugs should be taken with meals or with milk to prevent upset stomach. Others must be taken with a full glass of water. Be sure to follow directions for the best way to take the drug that is prescribed.
Precautions
Antimalarial drugs may cause lightheadedness, dizziness, blurred vision and other vision changes. Anyone who takes these drugs should not drive, use machines or do anything else thatmight be dangerous until they have found out how the drugs affect them.
The antimalarial drug mefloquine (Lariam) has received attention because of reports that it causes panic attacks, hallucinations, anxiety, depression, paranoia, and other mental and mood changes, sometimes lasting for months after the last dose. A study published in 1996 in the British Medical Journal noted that about 1 in 140 travelers who take the drug may have mental or mood changes severe enough to interfere with normal activities. This compares to about 1 in 1100 patients who have such reactions to the antimalarial drug chloroquine. Anyone who has unexplained anxiety, depression, restlessness, confusion, or other troubling mental or mood changes after taking mefloquine should call a physician right away. Switching to a different antimalarial drug may be an alternative and can allow the side effects to stop.
Anyone taking antimalarial drugs to prevent malaria who develops a fever or flu-like symptoms while taking the medicine or within 2-3 months after traveling to an area where malaria is common should call a physician immediately.
If the medicine is being taken to treat malaria, and symptoms stay the same or get worse, check with the physician who prescribed the medicine.
Patients who take this medicine over a long time need to have a physician check them periodically for unwanted side effects.
Babies and children are especially sensitive to the antimalarial drug chloroquine. Not only are they more likely to have side effects from the medicine, but they are also at greater risk of being harmed by an overdose. A single 300-mg tablet could kill a small child. Keep this medicine out of the reach of children. Use safety vials.
Special conditions
People with certain medical conditions or who are taking certain other medicines can have problems if they take antimalarial drugs. Before taking these drugs, be sure to let the physician know about any of these conditions:
Allergies
Anyone who has had unusual reactions to antimalarial drugs or related medicines in the past should let his or her physician know before taking the drugs again. The physician should also be told about any allergies to foods, dyes, preservatives, or other substances.
Pregnancy
In laboratory animal studies, some antimalarial drugs cause birth defects. But it is also risky for a pregnant woman to get malaria. Untreated malaria can cause premature birth, stillbirth, and miscarriage. When given in low doses to prevent malaria, antimalarial drugs have not been reported to cause birth defects in humans. If possible, pregnant women should avoid traveling to areas where they could get malaria. If travel is necessary, women who are pregnant or who may become pregnant should check with their physicians about the use of antimalarial drugs.
Breastfeeding
Some antimalarial drugs pass into breast milk. Although no problems have been reported in nursing babies whose mothers took antimalarial drugs, babies and young children are particularly sensitive to some of these drugs. Women who are breastfeeding should check with their physicians before using antimalarial drugs.
Other medical conditions
Before using antimalarial drugs, people who have any of these medical problems (or have had them in the past) should make sure their physicians are aware of their conditions:
- Blood disease
- Liver disease
- Nerve or brain disease or disorder, including seizures (convulsions)
- Past or current mental disorder
- Stomach or intestinal disease
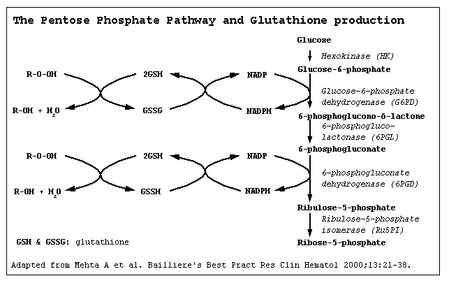
- Deficiency of the enzyme glucose-6-phosphate dehydrogenase (G6PD), which is important in the breakdown of sugar in the body
- Deficiency of the enzyme nicotinamide adenine dinucleotide (NADH) methemoglobin reductase
- Psoriasis
- Heart disease
- Family or personal history of the genetic condition favism (a hereditary allergic condition)
- Family or personal history of hemolytic anemia, a condition in which red blood cells are destroyed
- Purpura
- Hypoglycemia (low blood sugar)
- Blackwater fever (a serious complication of one type of malaria)
- Myasthenia gravis (a disease of the nerves and muscles).
Use of certain medicines
Taking antimalarial drugs with certain other drugs may affect the way the drugs work or may increase the chance of side effects.
Side effects
High doses of the antimalarial drug pyrimethamine may cause blood problems that caninterfere with healing and increase the risk of infection. People taking this drug should be careful not to injure their gums when brushing or flossing their teeth or using toothpicks. If possible, dental work should be postponed until treatment is complete and the blood has returned to normal.
The most common side effects of antimalarial drugs are diarrhea, nausea or vomiting, stomach cramps or pain, loss of appetite, headache, itching, difficulty concentrating, dizziness, lightheadedness, and sleep problems. These problems usually go away as the body adjusts to the drug and do not require medical treatment. Less common side effects, such as hair loss or loss of color in the hair; skin rash; or blue-black discoloration of the skin, fingernails, or inside of the mouth also may occur and do not need medical attention unless they are long-lasting.
More serious side effects are not common, but may occur. If any of the following side effects occur, check with the physician who prescribed the medicine immediately:
- Blurred vision or any other vision changes
- Convulsions (seizures)
- Mood or mental changes
- Hallucinations
- Anxiety
- Confusion
- Weakness or unusual tiredness
- Unusual bruising or bleeding
- Hearing loss or ringing or buzzing in the ears
- Fever, with or without sore throat
- Slow heartbeat
- Pain in the back or legs
- Dark urine
- Pale skin
- Taste changes
- Soreness, swelling, or burning sensation in the tongue.
Other rare side effects may occur. Anyone who has unusual symptoms after taking anantimalarial drug should get in touch with his or her physician.
Interactions
Some antimalarial drugs may interact with other medicines. When this happens, the effects of one or both of the drugs may change or the risk of side effects may be greater. Anyone who takes antimalarial drugs should let the physician know all other medicines he or she is taking. Among the drugs that interact with some antimalarialdrugs are:
- Beta blockers such as atenolol (Tenormin), propranolol (Inderal), and metoprolol (Lopressor)
- Calcium channel blockers such as diltiazem (Cardizem), nicardipene (Cardene), and nifedipine (Procardia)
- Other antimalarial drugs
- Quinidine, used to treat abnormal heart rhythms
- Antiseizure medicines such as vaproic acid derivatives (Depakote or Depakene)
- Oral typhoid vaccine
- Diabetes medicines taken by mouth
- Sulfonamides (sulfa drugs)
- Vitamin K
- Anticancer drugs
- Medicine for overactive thyroid
- Antiviral drugs such as zidovudine (Retrovir).
The list above does not include every medicine that may interact with every antimalarial drug. Be sure to check with a physician or pharmacist before combining an antimalarial drug with any other prescription or nonprescription (over-the-counter) medicine.
Key Terms
- Glucose
- A simple sugar that serves as the body's main source of energy.
- Hypoglycemia
- Abnormally low levels of glucose in the blood.
- Organism
- An individual of some type of life form, such as a plant or an animal.
- Parasite
- An organism that lives and feeds in or on another organism (the host) and does nothing to benefit the host.
- Protozoa
- Animal-like, one-celled organisms, some of which cause diseases in people.
- Psoriasis
- A skin disease in which people have itchy, scaly, red patches on the skin.
- Purpura
- A spotty or patchy purplish rash caused by bleeding under the surface of the skin.
Further Reading
For Your Information
Periodicals
- Schmidt, Elizabeth B. "The Road to Illville." Harvard Health Letter 19 (November 1993): 6.
Other
- Should You Take Lariam? Travel Health Information and Referral Service, 1997. http://travelhealth.com/lariam.htm.
Gale Encyclopedia of Medicine. Gale Research, 1999.