Nearly one half of the patients who visit a family practice have an alcohol or drug disorder. Primary care physicians have an opportunity to intervene at all stages during the course of addictive illness. Each stage can be characterized by types and severity of withdrawal and relapse prevention.[1-3] Management of alcohol and drug disorders includes assessment, intervention, prescription of medications, participation in specific addiction treatment strategies and monitoring of recovery.
Pharmacotherapy for Withdrawal Syndromes
Detoxification
Pharmacologic therapies are indicated for use in patients with addictive disorders to prevent life-threatening withdrawal complications such as seizures and delirium tremens, and to increase compliance with psychosocial forms of addiction treatment. Laboratory testing is indicated to assess the type and timing of drugs used addictively and to guide management of withdrawal and recovery.[4]
Alcohol
Management of alcohol withdrawal is based on the patient's history and current clinical status. The single best predictor of the likelihood of future withdrawal symptoms when alcohol is concerned is the patient's previous history, e.g., the presence or absence of seizures or delirium tremens (Table 1).
PCP = phencyclidine.
Alcohol withdrawal may be treated with a pharmacologic agent that exhibits cross-tolerance with alcohol. Agents that are commonly recommended include diazepam (Valium), lorazepam (Ativan), chlordiazepoxide (Limbitrol), clorazepate (Tranxeme) and phenobarbital. The usual initial dosage of diazepam or lorazepam is titrated according to elevations of blood pressure, pulse rate, degree of agitation and presence of delirium. In general, longer-acting preparations such as diazepam or chlordiazepoxide provide a smoother and safer withdrawal than other preparations. Shorter-acting preparations such as lorazepam are indicated when elimination time for benzodiazepines is prolonged, such as in patients with significant liver disease.
A loading dose of a long-acting benzodiazepine such as diazepam or chlordiazepoxide may be given initially, and the dosage may then be tapered. This method is often used in conjunction with a scale for detoxification. It is also used frequently in an inpatient setting. The physician should screen the patient for the presence of other sedating drugs to avoid untoward drug interactions, particularly oversedation. Initial loading doses for diazepam are in the range of 30 to 50 mg. Suggested parameters and dosages are presented in Table 2.
[TABULAR DATA 2 NOT REPRODUCIBLE IN ASCII]
Benzodiazepines and Other Sedative/Hypnotics
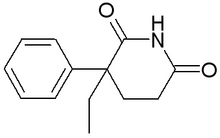
The signs and symptoms of benzodiazepine withdrawal are similar to those for withdrawal of other sedative/hypnotics (barbiturates, ethchytorvynol [Placidyl], glutethimide and meprobamate [Equanil]) (Table 1). The management of withdrawal for sedative/hypnotics (barbiturates) is similar to that for benzodiazepines (Table 3).
Information from references 5 through 8.
Withdrawal from benzodiazepines is not usually marked by significant elevations in blood pressure and pulse as commonly occur in patients undergoing alcohol withdrawal. Furthermore, supplemental doses of sedatives taken as needed are usually not required for changes in vital signs[5-8] (Table 3). Since benzodiazepines have cross-tolerance within that drug class as well as with other sedative/hypnotic drugs, benzodiazepines can be substituted for other sedative/hypnotics and vice versa. Equivalent doses can be calculated if the actual doses are known before beginning the tapering process (Table 4).
TABLE 4 Drug Dose Conversion(*) (Equivalent to 60 mg of Diazepam [Valium] and 180 mg of Phenobarbital)
NOTE: To find the dose of chlordiazepoxide equivalent to that of diazepam, multiply by 0.4. A dose of 150 mg of chlordiazepoxide is equivalent to a dose of 60 mg of diazepam. A dose of 100 mg is equivalent to a dose of 40 mg, etc.
(*)--Conversion factor x dose = diazepam or phenobarbital dose equivalent. Divide this amount in half to determine starting dosage.
A long-acting benzodiazepine is more effective than short-acting preparations in suppressing withdrawal symptoms and in producing a gradual and smooth transition to the abstinent state. In general, greater patient compliance and lower morbidity can be expected with the use of the longer-acting benzodiazepines, since withdrawal symptoms are less intense.
A taper over eight to 12 weeks or longer may be indicated in patients who have been taking benzodiazepines for several years (Table 5). The rate of taper can be adjusted according to patient tolerance. The rate of taper is a reduction in dosage of approximately 25 percent per quarter of the withdrawal period (e.g., 25 percent per week for one month).
Example: Patient taking 12 mg of lorazepam (Ativan) per day = 60 mg diazepam (Valium) x (50 percent reduction) = 30 mg.
Stimulants (Cocaine, Amphetamines and Derivatives)
Supportive rather than specific treatment is indicated in patients who are undergoing withdrawal from stimulants. Observation and monitoring for depression and suicidal ideation are advised (Table 1). Since stimulant withdrawal may cause significant irritability, a dosage of 5 to 10 mg of diazepam given orally every six hours on a fixed schedule or as needed for two to three days is recommended in patients with mild to moderate withdrawal symptoms. For severe withdrawal symptoms with persistent depression, therapy may be initiated with antidepressants such as desipramine (Norpramin), at a dosage of 50 mg per day, titrated upward every other day in 50-mg increments until a dosage of 150 to 250 mg per day is attained. The dosage is maintained for three to six months and discontinued by gradually tapering the drug over two weeks.[4,9] However, desipramine is not recommended routinely for management of withdrawal.
Opiates
Withdrawal symptoms from heroin addiction are predictable and identifiable (Table 1). Management of withdrawal can be accomplished with clonidine (Catapres) or methadone. Patients for whom clonidine is indicated include intranasal heroin users, outpatients and those who are motivated to achieve abstinency. Patients for whom methadone is indicated include intravenous users, inpatients, those who have medical and psychiatric complications and patients with a history of poor compliance when withdrawing from opiates[5,9,10] (Table 6). Federal regulations do not allow the use of methadone for detoxificafion if opiate withdrawal is the primary diagnosis. However, methadone may be used if the primary diagnosis is a medical condition and the secondary condition is withdrawal from opiates.
Information from references 5, 9 and 10.
Phencydidine and Other Psychedelic Agents
Acute symptoms of withdrawal from psychedelic agents may be diminished or reversed by using therapy with haloperidol (Haldol), 5 to 10 mg intramuscularly or orally every three to six hours as tolerated and needed for behavior control. Lorazepam, 1 to 2 mg intravenously, or diazepam, 5 to 10 mg orally every three to six hours, can also be given as needed. Behavior control may also be indicated (e.g., isolation and restraints).[5,9,11]
Medications for Relapse Prevention
Disulfiram
Disulfiram is a major aversive agent. It has been shown in a randomized, double-blind, placebo-controlled multisite trial[12] to be effective as an adjunct to other forms of addiction treatment.
The key components to effective use of disulfiram are overall patient motivation for abstinence and expectation of adverse reactions. Selected patients who have a commitment to working with other treatments for alcoholism may benefit from the addition of disulfiram therapy. The usual dosage of disulfiram is 250 mg per day, or 125 mg per day in patients who experience side effects such as sedation, sexual dysfunction and elevated liver enzymes.[12,13]
Disulfiram inhibits acetaldehyde dehydrogenase, an enzyme that catalyzes the degradation of acetaldehyde (formed by the action of alcohol dehydrogenase on alcohol). An accumulation of acetaldehyde produces an unpleasant reaction when alcohol is consumed that is similar to a severe hangover. It is potentially lethal, although only a small number of fatalities have been reported. The reaction to disulfiram is characterized by headache, diaphoresis, tachycardia, nausea and vomiting, cardiovascular collapse, delirium, seizures and, occasionally, death. Before using disulfiram, patients must have a blood alcohol level of zero and must be able to comprehend the risks and benefits of treatment.[12,13]
Methadone
Methadone maintenance is a form of pharmacologic management of opiate addiction. Methadone maintenance is performed in programs that are in compliance with federal regulations. Patients must meet admission requirements and must conform to clinic standards to participate in the program. Typically, methadone is given daily in oral doses ranging from 30 to 100 mg or greater. Methadone is administered under the supervision of a physician. Studies of methadone maintenance show initial efficacy following entrance to the program, and the medication remains effective in conjunction with other psychosocial forms of addiction treatment. Moreover, some studies show a reduction in intravenous drug use as well as in the rate of tests positive for human immunodeficiency virus infection.[5,9,14]
Methadone is an opiate agonist that acts competitively at opiate receptor sites to produce effects similar to those of other forms of opioids, such as heroin. Methadone is itself addicting, and patients commonly relapse to use of other drugs such as cocaine, alcohol, benzodiazepines and heroin. Nonetheless, methadone maintenance can be an alternative for patients who are addicted to intravenous heroin, particularly those who cannot or will not accept an abstinence-based addiction treatment program.[5,9,14]
Naltrexone
Naltrexone (ReVia) is an opioid antagonist that acts at opiate receptors to competitively inhibit effects of opiate agonists. It has no analgesic activity of its own. Preliminary controlled double-blind studies suggest that naltrexone is effective in decreasing the mean number of drinking days per relapse and in reducing the subjective craving for alcohol. Study subjects who relapsed tended to drink less alcohol and had shorter relapse periods than control subjects. Naltrexone was considered to be an adjunctive treatment, since all study subjects also were undergoing psychosocial forms of treatment for alcoholism.[15-17]
While interest in developing these agents appears warranted, caution is urged because of disappointment in the clinical efficacy of naltrexone in previous studies of patients addicted to opiates (except those who are most highly motivated).
Use of Psychosocial Addiction Treatment to Prevent Relapse
Medical management of alcohol and drug withdrawal often is not sufficient to produce sustained abstinence from recurrent use. Therefore, other types of addiction treatment are indicated to prevent relapse to alcohol and drug use following treatment of withdrawal.[18]
Cost Benefits of Treatment
Historically, addiction treatment has not been integrated within the mainstream of the health care system, even though such treatment is effective and reduces health care costs. More accurate data on treatment outcomes and costs are needed so that informed and rational decisions about addiction treatment can be formulated by consumers, insurers, physicians and policy makers. Fortunately, the results of several recent health services research studies unequivocally demonstrate the cost effectiveness of addiction treatment.[19-22]
Treatment Approaches and Effectiveness
The abstinence-based method is commonly used to treat alcohol/drug addiction (95 percent of programs surveyed). This method utilizes cognitive behavior techniques and referral to 12-step recovery programs, such as Alcoholics Anonymous (AA) and Narcotics Anonymous (NA).[23]
One-year abstinence rates of 80 to 90 percent were achieved when patients participated in weekly continuing care and/or AA meetings after discharge from the treatment program (Table 7). Also, one-year abstinence rates were associated with reduced rates of medical and psychiatric utilization[18] (Table 8).
TABLE 7 One-Year Abstinence by Continuum of Care and Self-Help Support
AA = Alcoholics Anonymous.
Information from reference 23.
TABLE 8 Medical Care Utilization One Year Before and After Treatment
Information from references 18 and 23.
Recovery in Alcoholics Anonymous
According to results of a 1992 survey conducted by AA, the following recovery rates were achieved. (1) Of those members sober in AA less than one year, 41 percent will attend AA another year. (2) Of those members sober more than one year and less than five years, 83 percent will attend AA another year. (3) Of those members sober five years or more, 91 percent will attend AA another year.[23]
Attendance in an abstinence-based treatment program such as AA can increase recovery rates from 41 to 80 percent in patients with alcolohism.[18,23] For this reason, patients with alcolohism should be referred to AA following withdrawal treatment and during maintenance therapy.
REFERENCES
[1.] U.S. Department of Health and Human Services, Public Health Service, National Institutes of Health, National Institute on Alcohol Abuse and Alcoholism. Epidemiology of alcohol use and alcohol-related consequences. In: Alcohol and health. Eighth special report to the U.S. Congress from the Secretary of Health and Human Services. September 1993:1-35.
[2.] Bennett JC, Plum F, eds. Cecil textbook of medicine. 20th ed. Philadelphia: Saunders, 1996.
[3.] Adams RD, Victor M, Ropper AH. Principles of neurology. 6th ed. New York: McGraw-Hill, Health Professions Division, 1997.
[4.] Miller NS, Gold MS, Smith DE, eds. Manual of therapeutics for addictions. New York: Wiley-Liss, 1997.
[5.] American Society of Addiction Medicine. Principles of addiction medicine. Washington, D.C. :The Society, 1994.
[6.] Miller NS, Gold MS. Abuse, addiction, tolerance, and dependence to benzodiazepines in medical and nonmedical populations. Am J Drug Alcohol Abuse 1991;17:27-37.
[7.] Rickels K, Schweizer E, Case WG, Greenblatt DJ. Long-term therapeutic use of benzodiazepines. I. Effects of abrupt discontinuation. Arch Gen Psychiatry 1990;47:899-907 [Published erratum appears in Arch Gen Psychiatry 1991;48:51].
[8.] Schweizer E, Rickets K, Case WG, Greenblatt DJ. Long-term therapeutic use of benzodiazepines. II. Effects of gradual taper. Arch Gen Psychiatry 1990;47:908-15.
[9.] Gorelick DA. Overview of pharmacologic treatment approaches for alcohol and other drug addiction. Intoxication, withdrawal, and relapse prevention. Psychiatr Clin North Am 1993;16:141-56.
[10.] Gold MS. Pharmacological therapies of opiate addiction. In: Miller NS, Gold MS, eds. Pharmacologic therapies for drug and alcohol addictions. New York: Marcel Dekker, 1995.
[11.] Giannini AT. Phencyclidine. In: Miller NS, ed. ComprehensiVe handbook of drug and alcohol addiction. New York: Dekker, 1991:383-94.
[12.] Fuller RK, Branchey L, Brightwell DR, Derman RM, Emrick CD, Iber FL, et al. Disulfiram treatment of alcoholism. A Veterans Administration cooperative study. JAMA 1986;256:1449-55.
[13.] Banys P. The clinical use of disulfiram (Antabuse): a review. J Psychoactive Drugs 1988;20:243-61.
[14.] Weddington WW. Methadone maintenance for opioid addiction. In: Miller NS, Gold MS, eds. Pharmacological therapies for drug and alcohol addictions. New York: Dekker, 1995:411-18.
[15.] Volpicelli JR, Alterman AI, Hayashida M, O'Brien CR Naltrexone in the treatment of alcohol dependence. Arch Gen Psychiatry 1992;49:876-80.
[16.] O'Malley SS, Jaffe AJ, Chang G, Schottenfeld RS, Meyer RE, Rounsaville B. Naltrexone and coping skills therapy for alcohol dependence. A controlled study. Arch Gen Psychiatry 1992;49:881-7.
[17.] O'Malley SS. Opioid antagonists in the treatment of alcohol dependence: clinical efficacy and prevention of relapse. Alcohol Alcohol 1996;31 (Suppl 1):77-82.
[18.] Miller NS. Treatment of the addictions: applications of outcome research for clinical management. New York: Haworth, 1995.
[19.] Gerstein DR, Johnson RA, Harwood H, Fountain D, Suter N, Malloy K. Evaluating recovery services: the California Drug and Alcohol Treatment Assessment (CALDATA). Sacramento, Calif.: State of California Department of Drug and Alcohol Programs, 1994.
[20.] Iglehart JK. The American health care system. Managed care. N Engl J Med 1992;327:742-7.
[21.] Holder HD, Blose JO. The reduction of health care costs associated with alcoholism treatment: a 14year longitudinal study. J Stud Alcohol 1992;53: 293-302.
[22.] Turnure C. Minnesota Consolidated Fund, annual cost offsets. Minnesota Department of Human Services, 1993.
[23.] Chappel JN, Long-term recovery from alcoholism. Psychiatr Clin North Am 1993; 16:177-87.
NORMAN S. MILLER, M.D., is associate professor of psychiatry and neurology and chief of the division of addiction programs at the University of Illinois School of Medicine, Chicago. He received a medical degree from Howard University, Washington, D.C., and completed a residency in psychiatry at Johns Hopkins Hospital, Baltimore, and a residency in neurology at the University of Minnesota, Minneapolis.
MARK S. GOLD, M.D., is professor of psychiatry at the University of Florida Brain Institute, Gainesville. He received a medical degree from the University of Florida College of Medicine, Gainesville, and served a residency in psychiatry at Yale University, New Haven, Conn.
Address correspondence to Norman S. Miller, M.D., University of Illinois at Chicago Department of Psychiatry (MC 913), 912 S. Wood Street, Chicago, IL 60612-7327. Reprints are not available from the authors.
COPYRIGHT 1998 American Academy of Family Physicians
COPYRIGHT 2000 Gale Group