Depression remains one of the most prevalent mental illnesses seen in primary care medicine.[1-3] When rigorous criteria are applied, between 5.8% and 22.3% of patients in primary care are found to suffer from a diagnosable depressive disorder.[4-6] These patients are impaired to an extent that is comparable to or greater than patients with other major chronic conditions.[7]
Randomized controlled trials have demonstrated that antidepressant medications are highly effective in acute and chronic forms of depression.[8,9] Controlled trials also provide evidence that various types of psychotherapy are effective for certain depressive conditions.[10] Although benzodiazepines reduce anxiety and may elevate mood, they do not appear to alleviate core depressive symptoms.[11,12] (The triazolo benzodiazepine alprazolam is a possible exception.[13,14] Moreover, depressed outpatients treated with antidepressants generally do not benefit from the addition of a benzodiazepine.[15,16]
The treatment provided to depressed patients in primary care and community settings has been the subject of considerable investigation.[17-21] Previous research suggests that primary care physicians tend to underutilize antidepressants and overutilize anxiolytics. Gullick and King[22] reported that benzodiazepines were prescribed twice as frequently as antidepressants to a group of depressed primary care patients referred for specialized psychiatric care. Keller and colleagues[17] found that anxiolytics were prescribed more often (55%) than antidepressants (34%) for a group of depressed individuals treated in the community before seeking treatment at university health care facilities.
Some evidence suggests that anxiolytic use has recently declined while antidepressant use has increased.[23-27] Between 1970 and 1989, the number of prescriptions for sedatives or hypnotics dispensed by US pharmacies declined by two thirds.[23] Between 1975 and 1984, there was also a modest increase in prescriptions for antidepressants.[24] Similar trends have been reported in Europe.[25,27] It is not known whether these general trends signal a shift in the choice of medications that primary care physicians use to treat their depressed patients.
In broad terms, primary care physicians and psychiatrists tend to prescribe different classes of psychotropic medications.[28,29] A 1981 survey[28] revealed that primary care physicians were more likely to prescribe anxiolytics than antidepressants and that psychiatrists were more likely to prescribe antidepressants than anxiolytics. This finding may simply reflect differences in the patient populations served by the two provider groups, however, rather than differences in prescribing practices per se. As compared with patients seen by psychiatrists, mentally ill primary care patients tend to be less seriously ill and are more likely to suffer from neurotic conditions and other anxiety-related disorders.[30]
The current study examines recent national trends in the treatment of patients diagnosed as depressed by office-based primary care physicians and psychiatrists. An assessment is presented of the pattern of psychotropic and psychological treatment provided to these two patient populations.
Methods
Data Source
The source of data for this report is the National Ambulatory Medical Care Survey (NAMCS). The NAMCS, which is conducted periodically by the National Center for Health Statistics (NCHS), samples a nationally representative group of visits to physicians in office-based practice. The current report is based on results from the 1980, 1985, and 1989 NAMCS.
Approximately 58,000 office visits were sampled in 1980, 75,000 visits in 1985, and 38,000 visits in 1989. Data from patient visits were collected with a 1-page data form that was completed by the attending physicians or their office staff. The form contained items such as the patient's age and sex, diagnoses, and medications prescribed. Only minor modifications were made in the survey form between 1980 and 1989.
Survey Design
The surveys were conducted using a three-stage sampling design. First, a probability sample was drawn of primary sampling units. A primary sampling unit was a county, a group of adjacent counties, or a standard metropolitan statistical area. Second, a probability sample was drawn of practicing physicians within these primary sampling units. Finally, a systematic random sample was drawn of the visits to these physicians. The sampling frame was a 1-week period. Physicians expecting more than 10 visits per day recorded every second, third, or fourth visit according to a predetermined sampling interval. This procedure provided a systematic random sample of patient its during the reporting period.
Sample of Physicians
The current analysis was confined to visits to psychiatrists and primary care physicians. Visits to psychiatrists included visits to physicians specializing in general psychiatry or a psychiatric subspecialty such as child psychiatry or psychoanalysis. To provide a sample size sufficient for detailed analyses, visits to physicians specializing in general practice, family practice, and internal medicine were considered together as primary care visits.
The 1980 survey included 172 psychiatrists and 914 primary care physicians; the 1985 survey included 178 psychiatrists and 904 primary care physicians; and the 1989 survey included 74 psychiatrists and 427 primary care physicians. The response rate among the psychiatrists was 85% in 1980, 74% in 1985, and 78% in 1989. The response rate among the primary care physicians was 73% in 1980, 66% in 1985, and 70% in 1989. Each of the three surveys sampled independently from the entire pool of eligible physicians' practices.
Visit Sample
Data from patient visits that resulted in a depressive disorder diagnosis were analyzed. Depressive disorder diagnoses included major depression (International Classification of Diseases, 9th Revision, Clinical Modification [ICD-9-CM]: 296.2, 296.3), depression not otherwise specified (311), and neurotic depression (300.40). The sample included patients diagnosed with a depressive disorder as either their first, second, or third listed diagnosis. In some analyses, a distinction was drawn between primary diagnosis (first listed diagnosis) and secondary diagnosis (second or third listed diagnosis). The analysis was limited to data from visits by patients who were at least 18 years of age at the time of the survey.
Psychotropic Drug Prescriptions
Psychotropic drugs were classified by a modification of the scheme provided in Drug Evaluations Annual.[31] Antidepressant, anxiolytic (benzodiazepine and nonbenzodiazepine anxiolytic), and antipsychotic medications were considered.
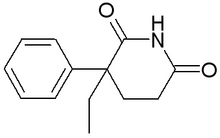
Antidepressant drugs include tricyclic antidepressants, monoamine oxidase inhibitors, and atypical antidepressants (bupropion, fluoxetine, and trazodone). Trazodone was not licensed for general use in the United States at the time of the 1980 survey, and bupropion and fluoxetine were not licensed for use at the time of the 1980 and 1985 surveys.
Anxiolytics include benzodiazepines and nonbenzoldiazepine anxiolytics. Nonbenzodiazepine anxiolytics include barbiturates, meprobamate, chloral hydrate, ethchlorvynol, ethinamate, glutethimide, methyprylon, buspirone, and the antihistamines. Alprazolam is classified as an anxiolytic rather than an antidepressant. Antipsychotic medications (eg. haloperidol and chlorpromazine) include the full range of neuroleptic medications.
Psychotherapy and Visit Duration
The survey included a "psychotherapy" variable that was defined as a nonmedication treatment "designed to produce a mental or emotional response through suggestion, persuasion, reeducation, reassurance, or support." The survey also included a visit duration variable that was defined to measure the length of time the patient spent with the physician.
Statistical Methods
One of the primary aims of the NAMCS is to provide national estimates of the volume and content of office-based care. Because the visit sampling is not entirely random, the NCHS weights each visit to inflate the sample and correct for sampling imperfections. The US Bureau of the Census population estimate for July 1 of each survey year is used to compute the annual visit rate. The percentages reported in the current report were based on the weighted estimates.
The construction of weights has three components: (1) inflation by reciprocals of sampling probabilities, (2) adjustment for nonresponse, and (3) a ratio adjustment to fixed totals. The adjustment for nonresponse replaces patient visits to nonrespondents with visits to respondents in the same specialty and same primary sampling unit. The ratio adjustment involves multiplying each visit by the ratio of physicians listed in the American Medical Association-American Osteopathic Association (AMA-AOA) master files for a given specialty over the number of sampled physicians in that specialty.
The NCHS provides tables for calculating the standard errors of the survey estimates. These tables were used to compute t test statistics. Comparisons were made for statistical significance for the two-tailed t test with infinite degrees of freedom.
A logistic regression was used to estimate the relative risk that an antidepressant would be prescribed for primary care patients who were diagnosed as having a depressive disorder. Results are presented as odds ratios (ORs) with associated 95% confidence intervals (CIs). This computation was made with unweighted data.
Results
Between 1980 and 1989, the total number of adult office visits provided annually by primary care physicians increased from 215.7 million to 244.0 million, and total annual visits to psychiatrists increased from 14.1 million to 15.3 million (Table 1). Visits that resulted in a depressive disorder diagnosis (herein termed "depression visits") accounted for a far smaller percentage of the primary care visits (1.6% to 2.1%) than of the psychiatric visits (35.8% to 42.6%).
[TABULAR DATA OMITTED]
In each survey year, depression visits to psychiatrists outnumbered depression visits to primary care physicians. In 1989, psychiatrists provided 49% more visits that resulted in a diagnosis of depression than primary care physicians. Depressive disorders were diagnosed in approximately one third of the mental disorder visits made by each provider group (Table 1).
Demographic Characteristics
Selected demographic characteristics of the patients who made psychiatric and primary care depression visits are presented in Table 2. Whites and women accounted for a majority of both samples. Over time, demographic variables of age, race, and sex of psychiatric and primary care patients with depression visits remained remarkably constant.
[TABULAR DATA OMITTED]
The distribution of visits according to age differed between psychiatrists and primary care physicians. As compared with the visits to primary care physicians, only a small proportion of the depression visits to psychiatrists were by patients over the age of 65 years.
The two provider groups differed from one another in the distribution of payment sources they received for the depression visits. Visits to primary care physicians were more likely to be paid for by Medicare or Medicaid, and visits to psychiatrists were more likely to be paid for with personal resources or commercial insurance (Table 2).
Diagnostic Characteristics
Whereas primary care physicians diagnosed medical disorders (ie, nonmental disorders) in a majority of the visits in which a depressive disorder was diagnosed (1980, 59.5%; 1985, 64.8%; 1989, 66.1%), diagnoses of medical disorders were less often made during depression visits to psychiatrists (1980, 11.9%; 1985, 9.0%; 1989, 8.8%). Hypertension was the most commonly coded comorbid medical diagnosis during primary care depression visits. It was diagnosed in 7.4% of the primary care depression visits in 1980, 7.0% in 1985, and 6.0% in 1989.
When primary care physicians diagnosed a depressive disorder, it was often coded as a secondary diagnosis (1980, 43.4%; 1985, 53.6%; 1989, 50.3%) rather than as the primary diagnosis. Almost all of the primary diagnoses in these visits were of medical rather than mental disorders (1980, 88.6%; 1985, 82.1%; 1989, 94.6%). In contrast, depressive disorder was the primary diagnosis in the vast majority of the psychiatric depression visits (1980, 81.7%; 1985, 85.2%; 1989, 89.7%).
Characteristics of Treatment
The vast majority of the primary care and psychiatric depression visits were made by patients who had previously seen their physician. In each sample, most of the visits also included a return appointment (Table 3). Instructions to follow-up on an as-needed basis were given more commonly during primary care depression visits than during psychiatric depression visits. Primary care depression visits seldom ended in referral to another physician (1980, 7.2%; 1985, 4.4%; 1989, 4.8%).
[TABULAR DATA OMITTED]
Primary care physicians more commonly offered a return appointment during visits of patients with depression than during visits of patients with other diagnoses (1980, 68.3% vs 57.9%, P < .05; 1985, 73.4% vs 57.3%, P < .01; 1989, 75.3% vs 59.9%, P = NS). Return appointments were most commonly provided, however, to primary care patients with a number of other specific chronic medical conditions, eg, essential hypertension 88.5%), congestive heart failure (83.0%), chronic obstructive pulmonary disease (85.0%), rheumatold arthritis (81.9%).
Psychotherapy was provided in the vast majority of psychiatric visits but in less than one third of primary care visits. The mean duration of visits to primary care physicians that resulted in a diagnosis of a depressive disorder was approximately half that of visits to psychiatrists by patients with diagnoses of depressive disorders.
The mean duration of primary care visits that included a diagnosis of depression was significantly (P < .001) longer than the duration of primary care visits that did not include a depressive disorder. This difference was greater in the 1980 survey (22.3 minutes vs 16.5 minutes) than in the later surveys (1985, 18.9 minutes vs 15.9 minutes; 1989, 19.2 minutes vs 16.4 minutes).
Psychotropic Drug Prescription
Primary care physicians and psychiatrists prescribed antidepressants to their depressed patients more frequently than any other class of psychotropic medication (Figure 1). As compared with psychiatrists, primary care physicians tended to prescribe antidepressants for proportionately more patients with depressive disorders. Over the period studied, psychiatrists prescribed antidepressants during an increasing percentage of their depression visits (32.7% to 45.2%), while primary care physicians prescribed antidepressants for such patients at an essentially constant rate (55.4% to 59.5%).
Between 1980 and 1989, the percentage of depression visits to primary care physicians that included antipsychotic medications declined steadily (P < .05) while the percentage of such visits to psychiatrists remained nearly constant. In 1980, antipsychotics were prescribed during a larger proportion of primary care depression visits than psychiatric depression visits (P < .05). In that year, thioridazine and perphenazine (in combination with amitriptyline) accounted for a majority of the antipsychotics prescribed during the primary care depression visits (32.1% and 37.4%, respectively). By 1989, antipsychotics were more commonly prescribed in psychiatric depression visits than primary care depression visits (P < .02).
During 1980, primary care physicians were significantly more likely than psychiatrists to prescribe benzodiazepines during visits in which depression was diagnosed (P < .05). Between 1980 and 1985, psychiatrists significantly increased their prescription of antidepressants (P < .01), so that the two provider groups prescribed antidepressants for a comparable proportion of their depressed patients. Between 1985 and 1989, both provider groups reduced their prescription of benzodiazepines during depression visits. In 1989, alprazolam was prescribed in 28.0% of the primary care depression visits and in 30.9% of the psychiatric depression visits that included a benzodiazepine prescription.
Throughout the study period, both provider groups prescribed nonbenzodiazepine sedatives or hypnotics in only a small percentage of their depression visits (psychiatrists, 0.4% to 1.5%; primary care physicians, 0.3% to 2.8%).
In the 1980 survey, nearly two thirds (63.6%) of the primary care depression visits that included a benzodiazepine prescription did not include an antidepressant. This percentage fell to 58.7% in 1985 and to 43.7% in 1989. In that year, 6.9% of the primary care depression visits included a benzodiazepine without an antidepressant, 8.9% of the visits included prescriptions for both types of medication, and 48.0% of the primary care depression visits included a prescription for an antidepressant without a prescription for a benzodiazepine.
Antidepressant Prescription
A logistic regression was conducted to estimate the strength of the association between selected clinical variables and the provision of an antidepressant during primary care depression visits. The estimated relative risk of receiving an antidepressant was significantly increased for patients who were white and for patients who received an appointment for a return visit. Although visits by depressed primary care patients under 65 years of age were more likely to result in an antidepressant being prescribed than visits by younger patients, this association did not reach statistical significance (Table 4).
Discussion
Previous reports of the NAMCS findings have focused on visits to office-based psychiatrists and other physician groups for the full range of mental disorders.[30] The current study builds on this earlier work by focusing on patients in whom depression was diagnosed.
Diagnostic Issues
Concern exists that depression often escapes the detection of health professionals. In the current study, we did not address this issue directly, but rather accepted the diagnoses made by the treating physicians.
The relatively low frequency of depressive disorder diagnosis in the reported primary care samples (1.6% to 2.1%) was consistent with reports of significant under-diagnosis[4-6] and consistent with previous research that indicates primary care physicians fail to label a substantial proportion of their patients who are depressed as defined by psychiatric research criteria.[32,33] Because the NAMCS does not contain an objective measure of depression, however, firm conclusions can not be made about the rate of illness detection.
Reliance on coded diagnoses probably contributes to underestimates of the number of patients considered to be depressed by their primary care physician. Written diagnoses may be avoided because some third-party payers restrict reimbursement for the treatment of depression and other mental disorders. Some physicians may substitute diagnoses such as "fatigue" or "insomnia" in a conscious effort to reduce the stigma associated with making a formal diagnosis of depression. Other physicians may not code depressive diagnoses for visits that were focused on an acute medical problem rather than on a known chronic depressive condition. Depression may also not be coded when physicians treat medical problems in patients known to be receiving appropriate ongoing mental health care for depression from a mental health specialist.
Psychological Treatment
Primary care physicians typically spend a few more minutes with their depressed patients than with their other patients. Although primary care physicians generally do not provide formal psychotherapy during these visits, it is possible that the added time is spent providing reassurance and support. A recent study of depression in psychiatric settings found that providing such clinical management," which often consists of attention, encouragement, and sympathetic concern, is beneficial to mildly depressed patients.[10,34] We need to know more about the provision and efficacy of less formal psychological interventions provided to depressed patients by primary care physicians.
At the conclusion of the visit, depressed primary care patients are usually scheduled for a return visit, especially if the patient is being treated with an antidepressant. Frequent contacts may be one strategy that primary care physicians use to support their patients through episodes of depression. In contrast, referral to another health care provider is relatively rare.
Lack of training in psychotherapy and reimbursement schedules that discourage extended patient visits make primary care physicians unlikely to increase their provision of time-intensive formal psychological interventions such as psychotherapy or psychological counseling. One option for primary care physicians is to employ a nurse or social worker to provide these services.[35] Under such an arrangement, the physician can refer those patients who do not respond to routine clinical management for a more extensive psychological intervention. This approach may be particularly well suited to group practices and health maintenance organizations.
Psychotropic Drug Prescriptions
Primary care physicians prescribed antidepressants more commonly than any other class of psychotropic medication to the patients they diagnosed as suffering from depression. Interestingly, primary care physicians appeared to be somewhat more likely than psychiatrists to prescribe antidepressants for recognized cases of depression. This finding runs counter to claims that primary care physicians underutilize antidepressant medications. One reason that primary care physicians may be more likely than psychiatrists to prescribe antidepressants is that primary care physicians have less access to nonpharmacologic strategies such as psychotherapy. Direct comparisons between the prescribing practices of primary care physicians and psychiatrists are confounded, however, by differences in the two patient populations. In addition to differences in age and extent of comorbid medical illness noted above, the depressed patients treated by primary care physicians and psychiatrists may well differ from one another in the severity, complexity, and duration of their depressive conditions. Unfortunately, the current survey provides little data on these critical issues.
The presented pattern of psychotropic medications prescribed by primary care physicians in recognized cases of depression markedly contrasts with earlier reports of high rates of benzodiazepine prescription and low rates of antidepressant prescription. Sampling bias in the earlier studies may account for this discrepancy. The three previous studies that found either high rates of prescribing anxiolytics or low rates of prescribing antidepressants were conducted on relatively small samples that had been referred for specialized psychiatric treatment.[17,19,20-22] This recruitment process biases selection toward more complicated cases. Before referral, these patients may have received less conventional treatment to control their symptoms. In contrast, the NAMCS samples a representative study of all office-based primary care visits.
During the 1980s, primary care physicians decreased their use of antipsychotics in the outpatient treatment of depression. Possible reasons for this decrease include an increased awareness of side effects associated with antipsychotics[36] and a decline in commercial efforts to promote the antipsychotic thioridazine for the treatment of agitation and depression in the elderly. The Journal of the American Medical Association, for example, contained 28 pages of advertisements for thioridazine in 1980, but none in 1989. Previous research has demonstrated that commercial factors exert a powerful influence over the prescribing behavior of physicians.[37]
One disconcerting finding to emerge from this study was that depressed nonwhite primary care patients appeared to be less likely to receive antidepressants than their depressed white counterparts. Previous research with community samples has indicated that substantially more depressed whites than depressed blacks receive mental health services.[19,38] The current findings suggest that racial inequities may persist following entry into the health care system. The possibility that racial factors influence the type or intensity of services that depressed persons receive raises serious concerns that demand closer study.
Limitations
The current study is constrained by several limitations in the survey data. As discussed above, survey diagnoses are based on practitioner judgment rather than independent assessment by the investigators. For this reason, the results relate only to those recognized cases of depression that are coded as such.
The survey data also do not permit a detailed analysis of differences between the clinical characteristics of depressed patients seen in the two treatment settings. Some research suggests that depressed patients in outpatient psychiatric settings may have different symptom patterns[39] and be more severely impaired[7] than those in primary care settings. More detailed measures of symptom severity and complexity are needed to clarify the intricate relationships between symptom profile, prescribing practices, and treatment setting.
No information is provided on the length or dosage of the medication trials. Previous research suggests that primary care physicians tend to prescribe antidepressants in dosages below accepted therapeutic levels for psychiatric patients.[20,40] In psychiatric populations, lower dosing regimens are associated with poorer outcome than higher dosing strategies.[41] However, comparable primary care studies have not been conducted.
The NAMCS measures office visits rather than individual patients and therefore oversamples frequent users of medical care. Furthermore, the survey is limited to office-based practice and so does not include the large number of medical visits that occur in medical clinics and other organized settings. With these limitations in mind, the NAMCS provides the only available national sample of outpatient treatment of depression by primary care physicians.
Conclusions
There have been frequent claims that primary care physicians improperly use psychoactive medications for the management of depression and other mental disorders. In particular, there has been a concern that anxiolytics arc used excessively and that antidepressants are underused.[17,42]
In the current study, data are presented that suggest that the primary care treatment of recognized cases of depression may be substantially better focused than was previously assumed. In 1989, more than half of the office-based primary care visits that resulted in a diagnosis of depression included a prescription for an antidepressant, and nearly three fourths (71.1%) included either an antidepressant or psychotherapy. Moreover, fewer than one in six of the primary care depression visits resulted in a benzodiazepine being prescribed, and less than one in ten included a benzodiazepine prescribed in the absence of an antidepressant.
Recent analysis of 1985 NAMCS data has revealed that a substantial proportion of the antidepressants prescribed to patients without mental disorders are prescribed for nonpsychiatric, antidepressant-responsive conditions.[43] Coupled with the current findings, these analyses suggest that the use of antidepressants in primary care is more sharply defined than has been suggested by earlier research.
Much remains to be learned about how primary care physicians routinely treat depression. Surveying clinical care in the manner employed by the NAMCS provides a general overview of treatment practices. Beyond such general surveys, detailed clinical research is needed to better understand what pharmacological and psychological strategies primary care physicians employ in their routine daily work. As the primary care treatment of depression becomes better defined, researchers will have an opportunity to compare prospectively the relative efficacy and cost of this care with the treatments routinely provided by mental health specialists.
References
[1.] Von Korff M, Shapiro S, Burke JD, et al. Anxiety and depression in a primary care clinic. Arch Gen Psychiatry 1987; 44:152-6. [2.] Kessler LG, Burns BJ, Shapiro S, et al. Psychiatric diagnoses of medical service users: evidence from the epidemiologic catchment area program. Am J Public Health 1987; 77:18-24. [3.] Barrett JE, Barrett JA, Oxman TE, Gerber PD. The prevalence of psychiatric disorder in a primary care practice. Arch Gen Psychiatry 1988; 45:1100-6. [4.] Hoeper EW, Nycz GR, Cleary PD, et al. Estimated prevalence of RDC mental disorder in primary medical care. Int J Mental Health 1979; 8:6-15. [5.] Jones LR, Badger LW, Ficken R.P, et al. Inside the hidden mental health network: examining mental health care delivery of primary care physicians. Gen Hosp Psychiatry 1987; 9:287-93. [6.] Schulberg HC, Saul M, McClelland M, et al. Assessing depression in primary medical and psychiatric practices. Arch Gen Psychiatry 1985; 42:1164-70. [7.] Wells KB, Stewart A, Hays RD, et al. The functioning and well-being of depressed patients: results from the Medical Outcomes Study. JAMA 1989; 262:914-9. [8.] Rogers SC, Clay PM. A statistical review of controlled trials of imipramine and placebo in treatment of depressive illness. Br J Psychiatry 1975; 127:599-603. [9.] Kocsis JH, Frances AJ, Voss C, et al. Imipramine treatment for chronic depression. Arch Gen Psychiatry 1988; 45:253-7. [10.] Elkin I, Shea T, Watkins JT, et al. National Institute of Mental Health treatment of Depression Collaborative Research Program: general effectiveness of treatments. Arch Gen Psychiatry 1989; 46:971-82. [11.] Schatzberg AF, Cole JO. Benzodiazepines in depressive disorders. Arch Gen Psychiatry 1978; 35:1359-65. [12.] Lipman RS, Covi L, Rickels K, et al. Imipramine and chlordiazepoxide in depressive and anxiety disorders. Arch Gen Psychiatry 1986; 43:68-77. [13.] Rickels K, Chung HR, Csanalosi IB, et al. Alprazolam, diazepam, imipramine, and placebo in outpatients with major depression. Arch Gen Psychiatry 1987; 44:862-6. [14.] Rickels K, Feighner JP, Smith WT. Alprazolam, amitriptyline, doxepin, and placebo in the treatment of depression. Arch Gen Psychiatry 1985; 42:134-41. [15.] Feet PO, Larsen S, Robak OH. A double blind study in outpatients with primary non-agitated depression treated with imipramine in combinations with placebo, diazepam, or dixyrazine. Acta Psychiatr Scand 1985; 72:334-40. [16.] Kravitz HM, Fogg L, Fawcett J, Edwards J. Antidepressant or antianxiety? A study of the efficacy of antidepressant medication. Psychiatry Res 1990; 32:141-9. [17.] Keller MA, Klerman GL, Lavori PW, Coryell W, Endicott J. Treatment received by depressed patients. JAMA 1982; 248: 1848-55. [18.] Uhlenhuth EH. Depressives, doctors, and antidepressants. JAMA 1982; 248:1879-80. [19.] Weissman MM, Myers JK, Thompson WM. Depression and its treatment in a US urban community - 1975-1976. Arch Gen Psychiatry 1981; 38:417-21. [20.] Keller MB, Lavori PW, Klerman GL, et al. Low levels and lack of predictors of somatotherapy and psychotherapy received by depressed patients. Arch Gen Psychiatry 1986; 43:458-66. [21.] Weissman MM, Klerman GL. The chronic depressive in the community: unrecognized and poorly treated. Compr Psychiatry 1977; 18:523-32. [22.] Gullick EL, King LJ. Appropriateness of drugs prescribed by primary care physicians for depressed outpatients. J Affective Disord 1979; 1:55-8. [23.] Wysowski DK, Baum C. Outpatient use of prescription sedative-hypnotic drugs in the United States, 1970 through 1989. Arch Intern Med 1991; 151:1779-83. [24.] Baum C, Kennedy DL, Knapp DE, Juergens JP, Faich GA. Prescription drug use in 1984 and changes over time. Med Care 1988; 26:105-14. [25.] Williams P, Bellantuono C, Fiorio R, Tansella M. Psychotropic drug use in Italy: national trends and regional differences. Psychol Med 1986; 16:841-50. [26.] Reidenberg MM. Effect of the requirement for triplicate prescriptions for benzodiazepines in New York State. Clin Pharmacol Ther 1991; 50:129-31. [27.] Battegay R, Wacker HR. Prescription habits for psychotropic drugs at a university psychiatric outpatient-clinic. Compr Psychiatry 1983; 24:502-7. [28.] Beardsley RS, Gardocki GJ, Larson DB, Hidalgo J. Prescribing of psychotropic medication by primary care physicians and psychiatrists. Arch Gen Psychiatry 1988; 45:1117-9. [29.] Olfson M. Depressed patients who do and do not receive psychiatric consultation in general hospitals. Gen Hosp Psychiatry 1991; 13:39-44. [30.] Shurman RA, Kramer PD, Mitchell JB. The hidden mental health network: treatment of mental illness by nonpsychiatrist physicians. Arch Gen Psychiatry 1985; 42:89-94. [31.] Drug evaluations annual, 1991. Chicago: American Medical Association, 1991. [32.] Perez-Stabte E, Miranda J, Munoz RF. Depression in medical outpatients: underrecognition and misdiagnosis. Arch Intern Med 1990; 150:1083-8. [33.] Zung WWK, Magill M, Moore JT, et al. Recognition and treatment of depression in a family medicine practice. J Clin Psychiatry 1983; 44:3-6. [34.] Freedman DX. Editorial note (especially for the media). Arch Gen Psychiatry 1989; 46:983. [35.] Klerman GL, Budman S, Berwick D, Weissman MM, Damico-White J, Bemby A, et al. Efficacy of a brief psychosocial intervention for symptoms of stress and distress among patients in primary care. Med Care 1987; 25:1078-88. [36.] Siomopuolos V. Psychiatric iatrogenic disorders. Am Fam Physician 1986; 34:111-6. [37.] Avorn J, Chen M, Hartley R. Scientific versus commercial sources of influence on the prescribing behavior of physicians. Am J Med 1982; 73:4-8. [38.] Sussman LK, Robins LN, Earls F. Treatment-seeking for depression by black and white Americans. Soc Sci Med 1987; 3:187-96. [39.] Emmons CA, Fetting JH, Zonderman AB. A comparison of the symptoms of medical and psychiatric patients matched on the Beck Depression Inventory. Gen Hosp Psychiatry 1987; 9:398-404. [40.] Tyrer P. Drug treatment of psychiatric patients in general practice. BMJ 1978; 2:1008-10. [41.] Goethe JW, Szarek BL, Cook WL. A comparison of adequately vs inadequately treated depressed patients. J Nerv Ment Dis 1988; 176:465-70. [42.] Hohmann AA, Larson DB, Thompson JW, Beardsley RS. Psychotropic medication prescription in US ambulatory medical care. DICP Ann Pharmacother 1991; 25:85-9. [43.] Broadhead WE, Larson DB, Yarnall KSH, Blazer DG, Tse CK. Tricyclic antidepressant prescribing for nonpsychiatric disorders: an analysis based on data from the 1985 National Ambulatory Medical Care Survey. J Fam Pract 1991; 33:24-32.
COPYRIGHT 1992 Dowden Health Media, Inc.
COPYRIGHT 2004 Gale Group