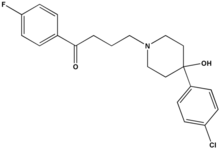
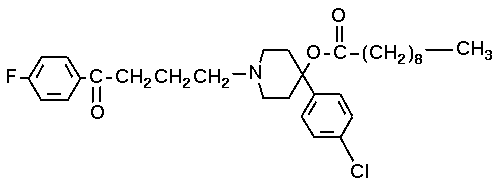
Introduction: IV haloperldol is used commonly for sedation in critically ill patients. However, IV haloperidol has been shown to cause the life-threatening ventrleular laehyarrhythmia torsades de pointes. Mechanisms by which haloperldol causes torsades de pointes have not been widely investigated in controlled studies.
Study objectives: To determine the effects of IV haloperidol on electrophysiologic parameters known to promote torsades de pointes.
Interventions: Monophasic action potential catheters were guided lender fluoroscopy into the right and left ventricles of 14 chloralose-anesthetized dogs (haloperidol, nine dogs; placebo, five dogs). Effective refractory period (ERP), action potential duration at 90% repolarization (AP[D.sub.90]), and QTc interval measurements were performed at baseline and after each of four doses of haloperidol (0.15, 0.5, 2.0, and 3.0 mg/kg) or placebo at three different pacing cycle lengths (450, 300, and 250 ms).
Measurements and results: IV haloperidol significantly prolonged left and right ventricular ERP by a magnitude of 12 to 20% at all pacing cycle lengths. ERP values in the placebo group did not change significantly from pretreatment values in either ventricle. Haloperidol significantly prolonged left ventricular AP[D.sub.90] at a pacing cycle length of 300 ms. The effects of haloperidol on right ventricular AP[D.sub.90] approached significance at a cycle length of 450 ms. Overall, haloperidol prolonged AP[D.sub.90] by 7 to 11% with less consistent and more variable effects than those for the ERP. AP[D.sub.90] was not significantly altered in the placebo groups. Haloperidol produced significant prolongation in QTc intervals. The electrophysiologic effects of haloperidol were related to dose, with a plateau reached at the 0.5 mg/kg dose for ERP measurements and at the 2 mg/kg dose for the AP[D.sub.90] and QTc interval measurements.
Conclusions: IV haloperidol prolongs ventricular ERP and AP[D.sub.90] in intact canine hearts. These electrophysiologic effects are likely associated with the clinical torsades de pointes-inducing actions of IV haloperldol in critically ill patients.
Key words: action potentials; arrhythmia; dogs; electrophysiology; haloperidol; QT intervals; torsades de pointes
Abbreviations: ANOVA = analysis of variance; APD = action potential duration: AP[D.sub.90] = action potential durationat 90% repolarization D5W = 5% dextrose in water ERP = effective refractory period
**********
Torsades de pointes is a potentially life-threatening polymorphic ventricular tachycardia that is characterized on a surface ECC by a twisting QRS morphology that is associated with prolongation of the QTc interval. (1) Torsades de pointes may be caused by many drugs from numerous different therapeutic classes, including antibiotics, antiarrhythmic agents, antidepressant agents, antipsychotic agents, and a variety of others. (2) Episodes of torsades de pointes may be prolonged and sustained, and the arrhythmia may degenerate into fatal ventricular fibrillation. (3-5)
IV haloperidol is widely used as a treatment for delusional agitation in critically ill patients. (6) Extremely high doses of IV haloperidol (as high as 975 mg per 24-h period) have been recommended by some clinicians for this indication. (6) Numerous cases of torsades de pointes associated with haloperidol appear in the literature. (7-17) The incidence of torsades de pointes associated with IV haloperidol use has been reported to be as high as 3.6% in clinically ill patients. (15)
Although the precise mechanism of torsades de pointes remains unknown, substantial evidence suggests that the arrhythmia is provoked by the initiation of early afterdepolarizations. (15) Early afterdepolarizations occur as a result of a failure of normal, complete membrane repolarization and can, therefore, be stimulated by conditions or drugs that prolong phase 2 or phase 3 membrane repolarization. (18) Early afterdepolarizations in turn result in a further delay in membrane repolarization, resulting in prolongation of the QTc interval on surface ECG. Drugs that produce early afterdepolarizations are those associated with the prolongation of monophasic action potential duration (APD) primarily through the prolongation of phase 3 membrane repolarization via blockade of delayed rectifier potassium channels. (18) Drugs that prolong APD, such as quinidine, (19) procainamide, (20) and erythromycin (21) have been shown to cause torsades de pointes.
Despite widespread use of high doses of IV haloperidol in critically ill patients and increasing numbers of reports of haloperidol associated torsades de pointes, mechanisms by which the drug causes torsades de pointes have nut been widely studied. Haloperidol is known to cause prolongation of the QTc interval on surface ECG, suggesting that the drug may prolong ventricular effective refractory period (ERP) and APD, leading to early afterdepolarizations. In addition, the relationship between haloperidol dose and its electrophysiologic effects has not been extensively investigated. Therefore, the purpose of this study was to determine the effect of IV haloperidol on these parameters that are known to be associated with torsades de pointes. The following hypotheses were tested in this investigation: (1) IV haloperidol prolongs ventricular ERP; (2) IV haloperidol prolongs ventricular APD; and (3) the effects of IV haloperidol on ventricular ERP and APD are dose-related.
MATERIALS AND METHODS
This was a randomized, placebo-controlled study conducted in 14 conditioned, heartworm-negative mongrel dogs of either sex (mean [[+ or -] SD] weight, 23.2 [+ or -] 2.7 kg; range, 18.2 to 27.2 kg). These experiments wow conducted in accordance with the Guide for the Care and Use of Laboratory Animals as adopted and promulgated by the National Institutes of Health. All procedures were approved by the Care of Experimental Animals Committee at Henry Ford Hospital.
Animal Preparation
Anesthesia was induced using a combination of diazepam, 0.17 mg/kg, oxymorphone, 0.22 mg/kg, and pentobarbital, 150 to 250 mg, dosed to effect. (22) Anesthesia was maintained using [alpha]-chloralose. 5 to 10 nN/kg/h, (21) adjusted using standard techniques. [alpha]-Chloralose was selected as the maintenance anesthetic because it exerts significantly less effect on the canine cardiovascular system than pentobarbital. (23) Animals were placed in the supine position on a surgical table covered with a warming blanket, and surface ECG leads were applied. The dogs were intubated and ventilated mechanically using a respirator (Harvard Apparatus; South Natick, MA) that was connected to a cuffued endotracheal tube. The left femoral artery and the right femoral vein were exposed surgically. A steerable, bipolar, 6F, silver-silver chloride combined contact monophasic action potential/pacing electrode catheter (EP Technologies Inc; Mountain View, CA) was advanced into the left ventricle via the femoral artery and was positioned at the apex. Another monophasic action potential catheter was advanced from the right femoral vein into the right ventricle and was positioned at the apex. Monophasic action potential signals were amplified and filtered using a universal signal amplifier (model No. 20-4615-58: Could Instruments; Valley View, OH). In addition, a catheter-tip micromanometer (Millar Instruments; Houston, TX) was advanced into the aorta via the femoral artery fin the measurement of systolic and diastolic BP. Catheters were positioned raider fluoroscopic guidance. Surface ECG leads II and AVF, amplified monophasic action potentials, right ventricular electrogram, and arterial BP were displayed on all oscilloscope (Windograf model; Gould Instruments). Paper recordings were made on an electrostatic chart recorder (Gould Instruments).
Monophasic Action Potential Recordings
Monophasic action potentials were recorded from the right and left ventricles at paper speeds varying during each recording from 25 to 100 mm/s during ventricular pacing. Paper speeds of 25 mm/s were used to visualize action potentials to assure optimal shape and to assure flint the catheter was in the correct position to make optimal ventricular contact in order that classic action potentials could be recorded. Action potential measurements were made using recordings performed at 100 mm/s. Monophasic action potentials were recorded at cycle lengths of 250, 300, and 450 ms (corresponding to paced heart rates of 240, 200, and 133 beats/min, respectively). Prior to the recording of monophasic action potentials, pacing was performed continuously for a minimum of 1 min to assure a "steady state." (21) Pacing was performed using a programmable stimulator (model DTU 210; Bloom Associates Ltd; Philadelphia, PA) generating rectangular impulses of 2 ms duration at a current equal to twice the diastolic pacing threshold. APD was measured from the beginning of phase 0 depolarization to the end of phase 4 repolarization. Left and right ventricular APDs were determined manually at 90% repolarization (AP[D.sub.90]) using standard methods, (21,24) APD measurements were determined by the average of three consecutive ventricular paced complexes prior to and following drug administration.
Determination of Ventricular ERPs
ERPs were determined in the left and right ventricles. Pacing was performed at each cycle length in trains of eight beats ([S.sub.1]). An initial premature test stimulus ([S.sub.2]) of 2 ms duration was delivered in a coupling interval of 250 ms following the last paced beat. The interval between [S.sub.1] and [S.sub.2] was decreased in 5-ms decrements until the [S.sub.2] failed to produce ventricular depolarization twice. The ERP was defined as the longest [S.sub.1] [S.sub.2] interval that failed to produce a propagated response.
Measurement of QTc Intervals
QT intervals were measured manually by a single investigator (JET) from ECGs obtained during each animal's natural (unpaced) heart Pates. A minimum of five consecutive complexes was used for each QT interval measurement, and the mean value was used. The QT interval was measured from the beginning of the QRS complex to the visual return of the T wave to the isoelectric line. (25,26) When the T wave was interrupted by a U wave, the end of the T wave was defined as tie nadir between the T and the U wave. (25,26) When the T wave appeared notched, the notch was disregarded (unless it was clearly a U wave interrupting the T wave), and the QT interval was measured as described above. QT intervals were corrected for heart rate using the method of Bazett. (27)
Drug Administration
Following surreal preparation and catheter insertion, animals were allowed to stabilize for 30 min to achieve stable BP (systolic BP, > 100 mm Hg; diastolic BP, > 70 mm Hg), heart rate, and oxygen saturation of > 90%. At baseline, the following measure ments were recorded: left ventricular AP[D.sub.90]; right ventricular AP[D.sub.90]; left and right ventricular ERP; QTc interval; and arterial BP.
Haloperidol lactate was prepared in 5% dextrose in water (DSW) at a concentration of 2 mg/mL. Haloperidol doses were selected in order to approximate the range of doses that have been used in critically ill patients for the treatment of delirious agitation, told to approximate doses of IV haloperidol that have been reported to cause torsades dc pointes in patients. (15) Haloperidol, 0.15 mg/kg, was administered IV over a period of 45 s (0.2 mg/kg/min). Ten minutes following the completion of the infusion, left and right ventricular AP[D.sub.90], left and right ventricular ERP, QTc interval, and BP measurements were repeated. Sixty minutes following the first infusion, haloperidol, 0.5 mg/kg, was administered IV at a rote of 0.2 mg/kg/min (over a period of 2.5 rain; cumulative dose, 0.65 mg/kg). Ten minutes following the completion of the infusion, measurements were repeated. Sixty, minutes following the completion of the previous haloperidol infusion, haloperidol, 2 mg/kg, was administered IV at the same infusion rote (over a period of 10 min; cumulative dose, 2.g5 mg/kg). Measurements were repeated 10 min following the completion of the infusion. Sixty minutes following the completion of the previous haloperidol infusion haloperidol, 3 mg/kg was administered (over a period of 15 rain; cumulative dose, 5.65 mg/kg). Measurements were repeated 10 min following the completion of the infusion. At each close, left and right ventricular AP[D.sub.90] were recorded during continuous pacing for 30 s at each of the three cycle lengths listed above. In the control (placebo) group, D5W was administered in volumes calculated to be the same as those given with haloperidol doses of 0.15, 0.5, 2, and 3 mg/kg. D5W was administered at infusion rates that were identical to the respective haloperidol infusion rates, and measurements were per formed as described above. Intervals between successive doses of placebo were as described for the haloperidol group. On completion of the experiments, animals were killed using a commercial solution of pentobarbital and potassium chloride (Euthasol; Delmarva Lab oratories; Midlothian, VA).
Statistical Analysis
AP[D.sub.90] and ERP in each ventricle across the escalating doses were analyzed using univariate repeated-measures analysis of variance (ANOVA) with the Greenhouse-Geisser sphericity correction that is designed to prevent the potential violation of the variance covariance assumption that underlies the repeated-measures ANOVA modeling. Significant differences by repeated measures ANOVA were analyzed using the Tukey pairwise multiple comparison test. QTc interval measurements in the haloperidol group were not normally distributed and were therefore analyzed using the Friedman repeated-measures ANOVA on ranks, Significant differences were analyzed using the Tukey pairwise multiple comparison test. QTc interval measurements in the placebo group were analyzed using one-way repeated-measures ANOVA.
RESULTS
Ventricular ERPs
The influence of IV haloperidol on left and right ventricular ERP measurements is presented in Figures 1 and 2, respectively. Haloperidol administration resulted in a significant prolongation of ERP of 12 to 20% compared to pretreatment values. In contrast, left and right ventricular ERPs were not prolonged significantly compared to pretreatment values in the placebo group (Table 1).
[FIGURES 1-2 OMITTED]
APD
The influence of IV haloperidol on left and right ventricular AP[D.sub.90] is shown in Figures 3 and 4, respectively. Left ventricular AP[D.sub.90] at 300 ms was prolonged significantly in the haloperidol-treated animals. In general, mean left ventricular AP[D.sub.90] was prolonged across the escalating doses of haloperidol by 7 to 11% compared to pretreatment values, although effects were not as consistent as, and exhibited greater variability than, the effects on ventricular ERP. In individual dogs, haloperidol administration resulted in prolongations of ventricular AP[D.sub.90] by as much as 39%. The administration of placebo resulted in no significant changes in left or right ventricular AP[D.sub.90] (Table 2).
[FIGURES 3-4 OMITTED]
QTc Intervals
The influence of IV haloperidol on QTc intervals is presented in Figure 5. Haloperidol produced significant prolongations in left and right ventricular QTc intervals compared to pretreatment values. QTc intervals were unchanged in the placebo group.
[FIGURE 5 OMITTED]
Effect of Haloperidol Dose on Changes in ERP and AP[D.sub.90]
Left and right ventricular ERP increased in a dose-related fashion at the 0.15 and 0.5 mg/kg doses, at which points a plateau effect was reached with little additional increase at doses of 2.0 and 3.0 mg/kg. Left and right ventricular AP[D.sub.9] increased in a dose-related fashion up to the 2.0 mg/kg dose, at which point AP[D.sub.90] effects reached a plateau. Similarly, effects on the QTc interval were dose-related up to the 2.0 mg/kg dose, with little further change following administration of the 3.0 mg/kg dose. In summary, the electrophysiologic effects of haloperidol were related to dose, with a plateau reached at the 0.5 mg/kg dose for ERP measurements, and at the 2 mg/kg dose for the AP[D.sub.90] and QTc interval measurements.
DISCUSSION
In this investigation, haloperidol was found to produce in vivo electrophysiologic changes that are known to predispose patients to the development of torsades de pointes, prolonging ventricular ERP hy 12 to 20%, and ventricular AP[D.sub.90] by up to 11%. Haloperidol prolonged ventricular ERP in a dose-related fashion, producing maximum effects on ventricular ERP at doses of 0.5 mg/kg, with little additional prolongation achieved with an additional dose of 2.0 mg/kg or 3.0 mg/kg, Haloperidol also prolonged ventricular AP[D.sub.90] and QTc intervals in a dose-related fashion, producing maximum effects at a dose of 2.0 mg/kg, with little further prolongation occurring at 3.0 mg/kg.
Numerous cases of haloperidol-associated QTc interval prolongation and/or torsades de pointes have been reported. (7-17,28,29) In addition to prolonging the QTc interval on surface ECG, IV haloperidol has been shown to increase 12 lead QT interval dispersion. (30) Haloperidol previously has been shown to inhibit voltage activated potassium conduction in rat pheochromocytoma PC12 cells (31) and to inhibit conductance through cloned inactivated cardiac human ether-a go-go-related gene potassium channels expressed in Xenopus oocytes. (32) However, few studies have investigated the in vivo cardiac: electrophysiologic effects of IV haloperidol and their relationship to haloperidol dose. In an uncontrolled study, Satoh et al (33) administered one dose (3 mg/kg) of IV haloperidol to a small group (six dogs) of beagle dogs. Ventricular ERP, AP[D.sub.90], and QTc interval were prolonged. In another non placebo-controlled study (34) in which the effects of haloperidol were compared with those of the antipsychotic agent aripiprazole in six dogs, ventricular ERP and AP[D.sub.90] were prolonged following administration of IV haloperidol, 0.03 mg/kg, and were further increased following administration of haloperidol, 3.0 mg/kg. However, no doses between 0.03 and 3.0 mg/kg were administered, precluding a more complete analysis of the relationship between dose and cardiac electrophysiologic effects.
In the present investigation, we studied a larger group of animals than in these previous investigations, and we employed a placebo group in order to account for changes in cardiac electrophysiology that might occur as a result of anesthesia, intubation, surgical cutdowns, and other procedures employed in the experiments. These data confirmed that IV haloperidol significantly prolongs ventricular ERP and QTc interval, and, to a lesser degree, AP[D.sub.90]. In addition, in the present study, we administered a wider range of haloperidol doses than in previous studies in order to more closely simulate the range of haloperidol doses that have been administered to critically ill patients for the management of delirious agitation, to simulate the range of doses that have been reported to cause torsades de pointes, (15) and to characterize the relationship between haloperidol dose and cardiac electrophysiologic effects within the range of clinically relevant doses. It is relatively common for critically ill patients to receive single IV haloperidol doses of 5 to 10 mg (0.075 to 0.15 mg/kg in a 70-kg patient) of higher. In sonic patients, torsades de pointes occurred after relatively low doses (ie, 10 mg over 4 h, or approximately 0.14 mg/kg in a 70-kg patient). (12) In other cases, however, torsades de pointes developed after cumulative halopcridol doses of 170 to 580 mg (approximately 2.5 to 8.3 mg/kg) over periods ranging from 24 to 96 h. (12,15) These dose ranges are similar to the range of cumulative doses administered in this investigation. Therefore, the IV haloperidol doses administered in the present study are clinically relevant and similar to those previously associated with torsades de pointes. The data presented in this investigation provide important new information regarding the relationship between haloperidol dose and in vivo electrophysiologic changes known to promote torsades de pointes. In vivo effects of haloperidol on ventricular ERP occur at relatively low haloperidol doses, and the maximum effect occurred at 0.5 mg/kg, or approximately 35 mg in a 70-kg patient. These data support previous data from a study of haloperidol-induced torsades de pointes in critically ill patients, (15) in which the administration of IV haloperidol [greater than or equal to] 35 mg within a 24-h period was a significant risk factor for torsades de pointes, increasing the odds of the arrhythmia 14-fold. The prolonging effects of IV haloperidol on AP[D.sub.90] and QTc interval also occurred at the lowest dose studied, and increased in a dose-related fashion, with a plateau at 2.0 mg/kg.
The limitations of this investigation should be noted. While the results of this investigation show that haloperidol influences electrophysiologic variables known to predispose an animal to torsades de pointes, no animal actually developed torsades de pointes, and therefore direct evidence of haloperidol as a torsades de pointes-inducing agent was not provided in this study. However, the drug is well-recognized as a torsades de pointes-provoking agent in humans, and these results indicate that haloperidol increases the risk of torsades de pointes. This investigation was designed to determine the effects of haloperidol on ERP and AP[D.sub.90] at single endocardial sites in the left and right ventricle, but was not designed to assess the effects of the drug on intraventricular dispersion of refractoriness or repolarization, which may be important contributors to an increased risk of torsades de pointes. In addition, this study was not designed to determine whether the effects of haloperidol on ERP and AP[D.sub.90] are dependent on rate (ie, "reverse-use dependent") as are the effects of many inhibitors of delayed rectifier potassium channels. The assessment of the potential in vivo rate dependency of haloperidol requires ablation of the atrioventricular node and pacing at longer cycle lengths (slower heart rates) than were tested in the present investigation. Further study is required to determine whether the electrophysiologic effects of haloperidol are dependent on heart rate.
In conclusion, in an anesthetized canine normal heart model, haloperidol influences electrophysiologic parameters known to predispose animals to torsades de pointes. The drug significantly prolongs ventricular ERP by 12 to 20%, and prolongs left ventricular AP[D.sub.90] by 7 to 11%. The maximum effects of haloperidol occur at doses of 0.5 to 2.0 mg/kg, with little additional prolongation achieved with an additional dose of 3.0 mg/kg. Haloperidol significantly prolonged the QTc interval in this model. Therefore, to minimize the risk of torsades de pointes associated with IV haloperidol, the drug should be used with caution and at relatively low doses in patients with risk factors for torsades de pointes, and concomitant use of haloperidol with other drugs known to prolong ventricular repolarization should be avoided.
* From the Department of Pharmacy Services (Drs. Rasty, Amin, and Tisdale). Division of Cardiovascular Research (Drs. Mishima and Sabbah), and the Henry Ford Heart & Vascular Institute (Dr. Borzak), Henry Ford Hospital and the Eugene Applebaum College of Pharmacy & Health Sciences, Wayne State University (Dr. Tisdale), Detroit. MI.
REFERENCES
(1) Jackman WM, Friday KJ, Anderson JL, et al. The long QT syndromes: a critical review, new observations and a unifying hypothesis. Prog Cardiovasc Dis 1988; 31:115-172
(2) Viskin S. Long QT syndromes and torsade de pointes. Lancet 1999; 354:1625-1633
(3) Vlasses PH, Ferguson RK, Rocci ML, et al. Lethal accumulation of procainamide metabolite in severe renal insufficiency. Am J Nephrol 1986; 6:112-116
(4) Woosley RL, Chen Y, Freiman JP, et al. Mechanism of the cardiotoxic actions of terfenadine. JAMA 1993; 269:1532-1536
(5) Gitler B, Berger LS, Buffa SD. Torsades de pointes induced by erythromycin. Chest 1994; 105:368-372
(6) Tesar GE, Stern TA. Rapid tranquilization of the agitated intensive care unit patient. J Intensive Care Med 1988; 3:195-201
(7) Zee Cheng CS, Mueller CE, Seifert CF, et al. Haloperidol and torsades de pointes [letter]. Ann Intern Med 1985; 102:418
(8) Fayer SA. Torsades de pointes ventricular tachyarrhythmia associated with haloperidol. J Clin Psychopharmacol 1986; 6:375-376
(9) Kriwisky M, Perry GY, Tarchitsky D, et al. Haloperidol induced torsades de pointes. Chest 1990:98:482-484
(10) Henderson RA, Lane S, Henry JA. Life threatening ventricular arrhythmia (torsades de pointes) after haloperidol overdose. Hum Exp Toxicol 1991; 1:59-62
(11) Metzger E, Friedman R. Prolongation of the corrected QT and torsades de pointes cardiac arrhythmia associated with intravenous haloperidol in the medically ill. J Clin Psychopharmacol 1993; 13:128-132
(12) Wilt JL, Minnema AM, Johnson RF, et al. Torsade de pointes associated with the use of intravenous haloperidol. Ann Intern Med 1993; 119:391-394
(13) DiSalvo TG, O'Gara PT. Torsade dc pointes caused by high-dose intravenous haloperidol in cardiac patients. Clin Cardiol 1995; 18:285-290
(14) Hunt N, Stern TA. The association between intravenous haloperidol and torsades de pointes: three cases and a literature review. Psychosomatics 1995; 36:541-549
(15) Sharma N, Rosman H, Padhi ID, et al. Torsades de pointes associated with intravenous haloperidol in critically ill patients. Am J Cardiol 1998; 81:238-240
(16) O'Brien JM, Rockwood RP, Suh KI. Haloperidol-induced torsades de pointes. Ann Pharmacother 1999; 33:1046-1050
(17) Perrault LP, Denault AY, Carrier M. et al. Torsades de pointes secondary to intravenous haloperidol after coronary bypass grafting surgery. Can J Anaesth 2000; 47:251-254
(18) Tan HE, Hou CJY, Lauer MR, et al, Electrophysiologic mechanisms of the long QT interval syndromes and torsade de pointes. Ann Intern Med 1995; 122:701-714
(19) Kaseda S, Gilmour RF, Zipes DP. Depressant effect of magnesium on early afterdepolarizations and triggered activity induced by cesium, quinidine, and 4-aminopyridine in canine cardiac Purkinje fibers. Am Heart J 1989; 118:458-466
(20) Habbab MA, el-Sharif N. Drug-induced torsades de pointes: role of early afterdepolarizations and dispersion of repolarization. Am J Med 1990; 89:241-246
(21) Rubart M, Pressler ML, Pride HP, et al. Electrophysiological mechanisms in a canine model of erythromycin associated long QT syndrome. Circulation 1993; 88:1832-1844
(22) Sabbah HN, Shimoyama H, Kono T, et al. Effects of long-term monotherapy with enalapril, metoprolol, and digoxin on the progression of left ventricular dysfunction and dilation in dogs with reduced ejection fraction. Circulation 1994; 89: 2852-2859
(23) Holzgrefe HH, Everitt JM, Wright EM. Alpha-chloralose as a canine anesthetic. Lab Anim Sci 1987; 37:587-595
(24) Franz MR. Method and theory of monophasic action potential recording. Prog Cardiovasc Dis 1991; 33:347-368
(25) Spargias KS, Lindsay SJ, Kawar GI, et al. QT dispersion as a predictor of long-term mortality in patients with acute myocardial infarction and clinical evidence of heart failure, Eur Heart J 1999; 20:1158-1165
(26) Brendorp B, Elming H, Jun L, et al. QTc interval as a guide to select those patients with congestive heart failure and reduced left ventricular systolic function who will benefit from antiarrhythmic treatment with dofetilide. Circulation 2001; 103:1422-1427
(27) Bazett HC. An analysis of the time relations of electrocardiograms. Heart 1920; 7:35-70
(28) Douglas PH, Block PC. Corrected QT interval prolongation associated with intravenous haloperidol in acute coronary syndromes. Catheter Cardiovasc Interv 2000; 50:352-355
(29) Hatta K, Takahashi T, Nakamura H, et al. The association between intravenous haloperidol and prolonged QT interval. J Clin Psychopharmacol 2001; 21:257-261
(30) Tisdale JE, Rasty S, Padhi ID, et al. The effect of intravenous haloperidol on QT interval dispersion in critically ill patients: comparison with QT interval prolongation for assessment of risk of torsades de pointes. J Clin Pharmacol 2001; 41:1310-1318
(31) Nakazawa K, Ito K, Koizumi S, et al. Characterization of inhibition by haloperidol and chlorpromazine of a voltage-activated K+ current in rat phaeochromocytoma cells. Br J Pharmacol 1995; 116:2603-2610
(32) Suessbrich H, Schonherr R, Heinemann SH, et al. The inhibitory effect of the antipsychotic drug haloperidol on HERG potassium channels expressed in Xenopus oocytes. Br J Pharmacol 1997; 120:968-974
(33) Satoh Y, Sugiyama A, Tamura K, et al. Effect of magnesium sulfate on the haloperidol-induced QT prolongation assessed in the canine in vivo model under the monitoring of monophasic action potential. Jpn Circ J 2000; 64:445-451
(34) Sugiyama A, Satoh Y, Hashimoto K. In, vivo canine model comparison of cardiohemodynamic and electrophysiological effects of a new antipsychotic drug aripiprazole (OPC-14597) to haloperidol. Toxicol Appl Pharmacol 2001; 173:120-128
Drs. Amin and Rasty were supported in part by investigator-initiated unrestricted grants from Hoechst-Marion Roussel. Dr. Amin also was supported by an American College of Clinical Pharmacy Cardiovascular Fellowship, funded by the American College of Clinical Pharmacy and Merck and Co.
Manuscript received February 27, 2003; revision accepted October 3. 2003.
Reproduction of this article is prohibited without written permission firm the American College of Chest Physicians (e-mail: permissions@ehestnet.org).
Correspondence to: James Tisdale, PharmD, Department of Pharmacy Practice, School of Pharmacy and Pharmacal Sciences Purdue University, W7555, Myers, Building, 1001 West Tenth St, Indianapolis, IN 46202; e-mail: jtisdale@iupui.edu
COPYRIGHT 2004 American College of Chest Physicians
COPYRIGHT 2004 Gale Group